Earn New Surgical SkillsOptometric surgery is increasingly becoming a core responsibility of the profession. Today, 17 states (and counting) allow ODs to perform laser or other minor surgical procedures. Here to offer tips and advice on surgery implementation and technique is the December 2023 issue of Review of Optometry, the magazine's 30th annual surgery report. Inside, experts offer advice on performing SLT, equipping your office for surgery and handling complications of in-office procedures, along with a review of the newest IOLs on the market. Check out the other articles featured in the December issue: |
Injections, laser procedures and surgical interventions are all valuable in-office treatments that optometric physicians can provide for their patients. As with any potential procedure, these categories of treatment are not without their own set of risks and difficulties. Outlined below are both common and uncommon complications for laser procedures, minor surgical methods and injections, all of which are broken down by procedure type.
The key to avoidance and mitigation of most adverse reactions or outcomes consists of proper surgical technique, maintaining asepsis and possessing a thorough understanding of instrumentation and ocular anatomy; however, even with the best of techniques, issues can arise. The eyecare provider stating they have never had a complication with any procedure likely has not performed enough or has performed very few. Be prepared to manage the most common complications and the most severe.
Laser Procedures
There are three main types of optometric laser treatments that may cause varied effects.
Nd:YAG Capsulotomy (YAG cap)
Posterior capsular opacification (PCO) is the most common complication after cataract surgery. Proliferation and growth of lens epithelial cells can severely impact patients’ daily living activities and lead to visual symptomatology. PCO can develop months to years following extraction.1 Hydrophobic acrylic intraocular lenses (IOLs) have demonstrated a lower incidence of PCO when compared with silicone and hydrophilic acrylic IOLs.1
YAG cap is a routine and efficient laser procedure that can be performed in your office to treat PCO; however, any laser procedure will present the possibility of causing complications, due to laser energy that enters the eye. Contraindications to look for before performing a YAG capsulotomy include corneal scars or opacities that limit adequate view of the PCO, uveitis, cystoid macular edema (CME), macular pathology, horseshoe tears or high risk of retinal detachment (RD).2 The presence of these conditions would need to be considered on a case-by-case basis or referred for ophthalmology clearance before performing capsulotomy.
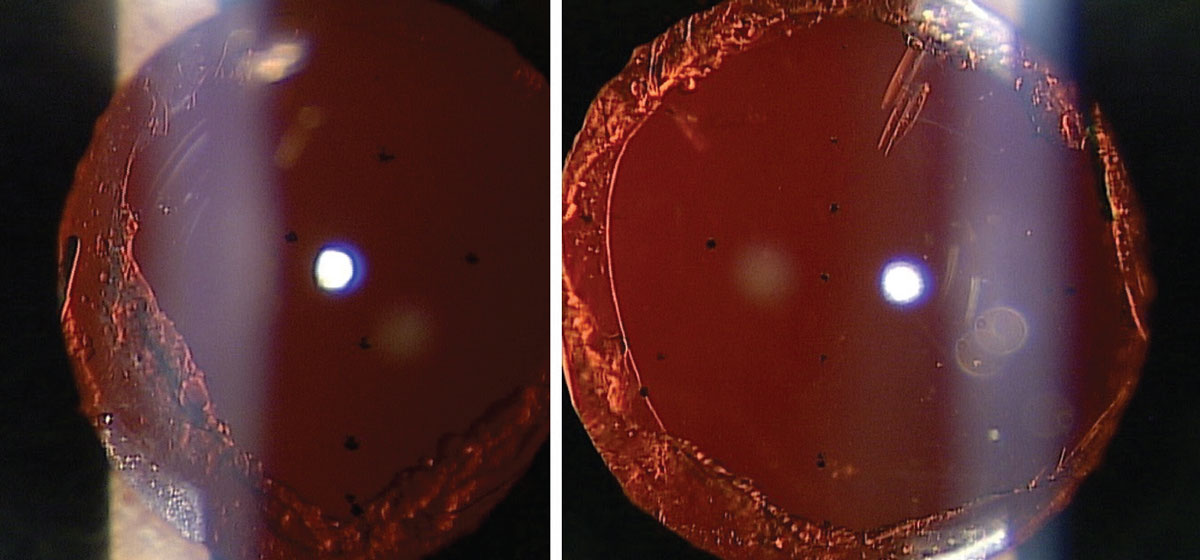
IOL pitting. Damage or pitting of the IOL can occur when laser shockwaves move anteriorly and hit the IOL (Figure 1). Factors potentially leading to IOL pits are misalignment of the laser focus, patient movement or IOL material. Silicone IOLs tend to be more susceptible to IOL pits than acrylic ones.2 Methods to prevent pitting are to increase the posterior offset (200µm to 300µm from the posterior capsule) and starting treatment in the periphery to avoid the visual axis. Thankfully, IOL pits are not visually significant and will rarely affect patients’ visual functioning. Various studies have shown the rate of IOL pits ranges from 7.8% to 19.8%.3,4
 |
|
Fig. 1. IOL pits caused by YAG capsulotomy. Click image to enlarge. |
Inflammation. Transient anterior iritis is a possible complication after YAG cap, typically resolving in a few days on topical corticosteroid or topical nonsteroidal anti-inflammatory drug (NSAID) therapy. Various studies have shown the rate of uveitis after capsulotomy is between 0.3% to 9.9%.3
Intraocular pressure (IOP) elevation. Transient increase in IOP is another possible complication with any of the laser procedures discussed in this section. It may occur after capsulotomy due to debris deposition in the trabecular meshwork or inflammatory swelling of the ciliary body associated with angle closure.2,4
One risk factor for IOP elevation is higher total laser energy used during the procedure. Elevated IOP can be prevented by using topical hypotensive medications both pre- and postoperatively, such as alpha-agonists or beta-blockers. Topical hypotensive drops may also be prescribed short-term in patients at risk of prolonged IOP elevation and subsequent damage, including those with advanced glaucoma or steroid responders. Various studies report rates of IOP elevation after capsulotomy ranging between 0.4% to 12.6%.3
How to Avoid the "Worst Case Scenario"As it relates to any laser procedures, injections or surgical procedures, this would entail permanent vision loss. One such scenario for laser procedures consists of retinal or macular burns that developed following a procedure that was accidentally performed with the wrong laser. This most often occurs when a YAG capsulotomy is performed accidentally on SLT mode. There have been rare case reports in the literature regarding YAG capsulotomies done with an SLT laser.18,19 This will result in the SLT laser beam traveling through the posterior capsule until it hits a pigmented structure, most likely the heavily pigmented retinal pigment epithelium in the macula or foveal region. Laser energy applied directly to the macular or foveal region has a high likelihood of causing irreversible, permanent vision loss. For this reason, it is highly recommended for all eyecare providers to perform a “time-out” prior to every procedure, but especially for laser procedures. The time-out is your opportunity to take a few seconds and have the treating clinician as well as a second individual (usually a technician) confirm the correct laser is being used with the correct laser settings, laser lens and that the correct eye is being treated. A time-out takes just a matter of seconds and is invaluable to help ensure the worst-case scenario does not happen in your office. |
Cystoid macular edema. This condition can occur due to movement of the vitreous or damage to the blood-aqueous barrier, causing the release of inflammatory mediators in the retina.2,4 Although rare, CME should be treated with topical corticosteroids and NSAID, just like with treating post-cataract surgery CME. Any cases of non-resolving CME should be referred to ophthalmology for treatment. The rate of CME after capsulotomy ranges between 0.1% to 2.9%, as various studies show.3,4
Retinal detachment. This is one of the most severe, yet rare, complications after YAG cap. The exact mechanism that leads to an RD or retinal tear is unknown; however, it has been shown that the presence or absence of a posterior vitreous detachment at the time of capsulotomy is not a factor in increasing the risk for RD in the first year after laser treatment.4 Increased risk of RD is found in patients with a history of RD, lattice degeneration, axial length greater than 24mm and posterior capsule rupture during cataract surgery.4 Any cases of RD should be urgently referred to ophthalmology for treatment and management. Luckily, the rate of retinal detachment after YAG cap is low, ranging from 0.2% to 2.3%.3,4
It has been thoroughly concluded in the literature that complications such as IOL pitting, iritis, IOP elevation, CME and retinal detachment are much more common when total laser energy is higher.3 One study also concluded that capsulotomy aperture diameter should not exceed 4.0mm in order to decrease the risk of complications.6 Accordingly, the lowest total laser energy that will complete the procedure successfully should be used to minimize risk of these complications emerging.
Selective Laser Trabeculoplasty (SLT)
This procedure is increasingly used as first-line therapy for open-angle glaucoma and ocular hypertension. SLT uses laser energy to cause biologic effects where inflammatory cells clean up the debris in the trabecular meshwork, consequently increasing aqueous outflow. Although the mechanism of action of SLT is not fully understood, it is believed that there is a subclinical SLT-induced inflammatory process, which helps facilitate IOP lowering.7
IOP elevation. Most IOP elevations are initially seen one hour postoperatively and usually resolve within 24 hours without any long-term complications.2,8,9 Transient elevation may be more commonly seen in eyes with a heavily pigmented trabecular meshwork.2,8 This can be prevented through use of topical hypotensive medications pre- and postoperatively.10 Additionally, clinical experience has shown the incidence of IOP elevation in heavily pigmented angles goes down when treating fewer degrees of the trabecular meshwork (180µm or less instead of 360µm) as well as reducing treatment energy (0.4mJ to 0.6 mJ per pulse instead of the typical 0.8mJ to 1.0 mJ). Rates of IOP elevation after SLT have been reported to be around 0.01% to 27%.2,8-12
 |
|
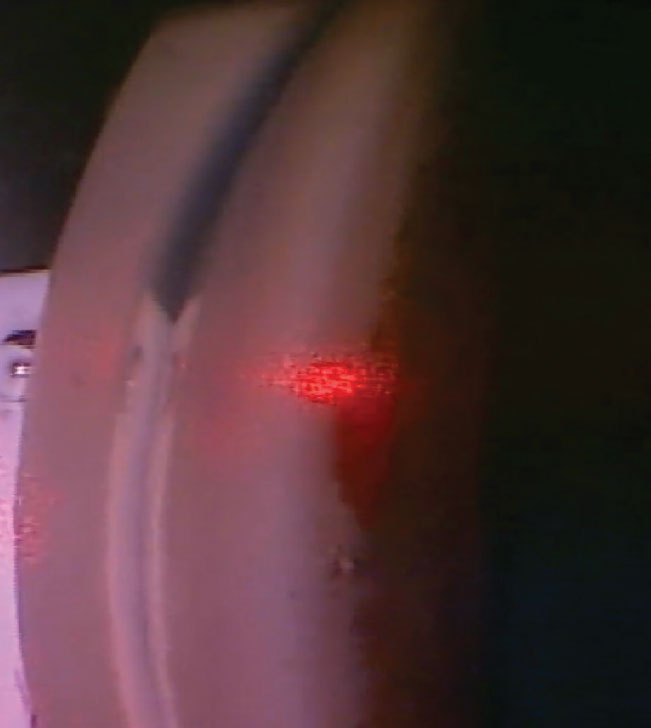
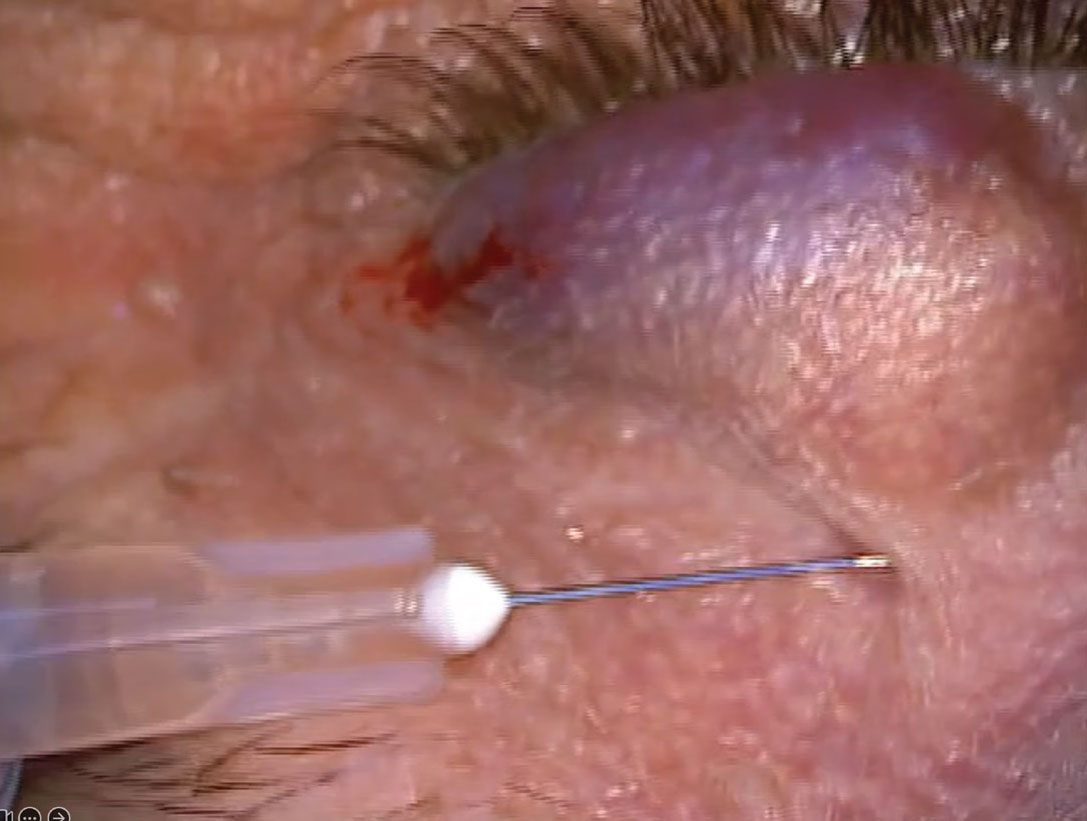
Fig. 2. Angle bleed during SLT. Click image to enlarge. |
Inflammation. Transient anterior uveitis typically occurs one to three days after SLT and resolves in approximately five days.8 Risk factors for anterior uveitis include patients with a heavily pigmented trabecular meshwork or history of previous argon laser trabeculoplasty.8 Transient anterior uveitis after SLT has been reported in up to 83% of patients.2,8 Topical steroids can be used to treat any iritis. It is important to note that the mechanism of SLT is inflammatory, thus some degree of inflammatory reaction is expected.
Hyphema/angle bleed. After SLT, hyphema is a very rare complication. Only two cases have been reported, both in patients with open-angle glaucoma who developed a hyphema three days after SLT, which self-healed without intervention.8 If bleeding is seen during SLT (Figure 2), hold gentle pressure with the SLT laser lens on the eye to stop the bleed.
Corneal changes. SLT may result in some corneal changes, such as corneal edema, corneal haze and endothelial cell count changes, occurring one to two hours after procedure.8 These changes are usually not visually or clinically significant and self-resolve. The incidence of corneal edema after SLT is 0.8%.8 There have been eight reported cases of SLT-induced keratitis causing a hyperopic shift.8 Keratitis can be treated with frequent use of artificial tears and lubricating ointment, while corneal edema and haze can be treated with sodium chloride hypertonic ophthalmic solution or topical corticosteroid.
Laser Peripheral Iridotomy (LPI)
This laser type is used as a form of treatment for patients with narrow angles, primary angle closure, primary angle closure glaucoma and occasionally in pigment dispersion syndrome. It eliminates the pupillary block component in primary angle closure and allows the flow of aqueous humor from the posterior to anterior chamber.13
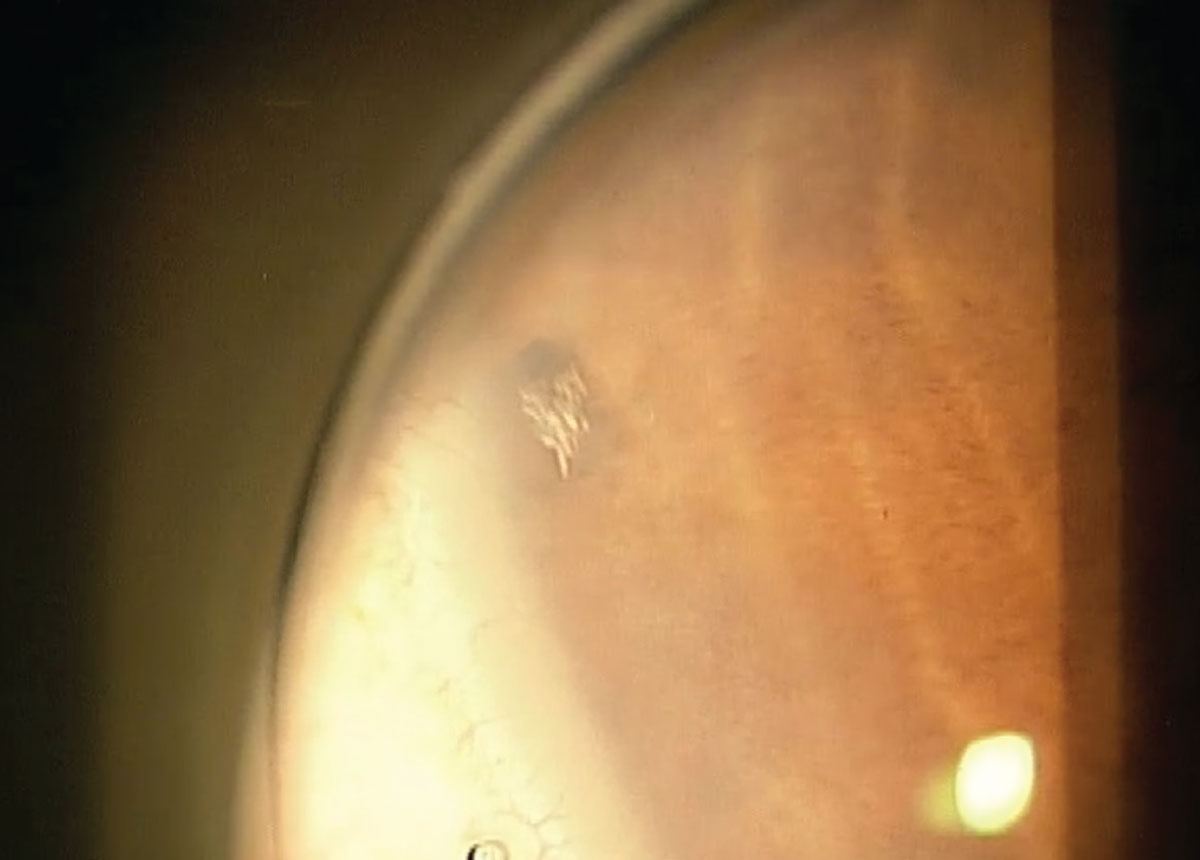
Non-patency of the iridotomy. An LPI may become non-patent after the procedure (Figure 3). Studies show that repeat LPI was required in 1% of patients two weeks after initial LPI and in 20% of cases within six months of initial treatment.14 The endpoint to watch for during an LPI is a “pigment plume,” which indicates that the laser has penetrated through the iris tissue. Ensure that the diameter of the LPI is at least 0.2mm to 0.5mm at the conclusion of the procedure to prevent small iris strands from growing over the iridotomy and causing non-patency. If maximal laser energy has been put into the eye during the initial procedure (100mJ to 150mJ), it may be beneficial to stop treatment and complete the procedure at the one-week follow-up examination. Oftentimes with thicker brown irises, it is common to re-treat the following week. Retroillumination and direct viewing of the PI hole with a gonioscopy lens can be done to examine for PI patency.
 |
|
Fig. 3. Non-patency of an LPI one week postoperatively. Click image to enlarge. |
IOP elevation. Increased pressure may occur more often after an LPI due to the higher amount of total laser energy used or iris pigmentation blocking the trabecular meshwork and decreasing aqueous outflow.14 IOP elevation after LPI has been seen in 6% to 10% of cases.14 Use of topical hypotensive medications pre- and postoperatively can minimize elevations. Should they occur, low elevations (<10mm Hg) can be treated with topical medications such as alpha-agonists, beta-blockers or carbonic anhydrase inhibitors. High IOP elevations (>10mm Hg) can instead be treated with oral carbonic anhydrase inhibitors, such as acetazolamide, in addition to topical therapy. Risk factors and side effects of acetazolamide should be considered for each patient.
Hyphema. Iris bleeding is seen in 30% to 40% of LPIs.14 If bleeding does occur (Figure 4), hold gentle pressure with the laser lens on the eye for 30 to 60 seconds. If a hyphema develops after the procedure, it can be treated with topical therapy, including corticosteroids, cycloplegics and hypotensive medications. Do note that there is no increased risk of bleeding in patients on antithrombotic therapy. As such, these medications do not need to be discontinued before an LPI.14
 |
|
Fig. 4. Iris bleed during a YAG LPI. Click image to enlarge. |
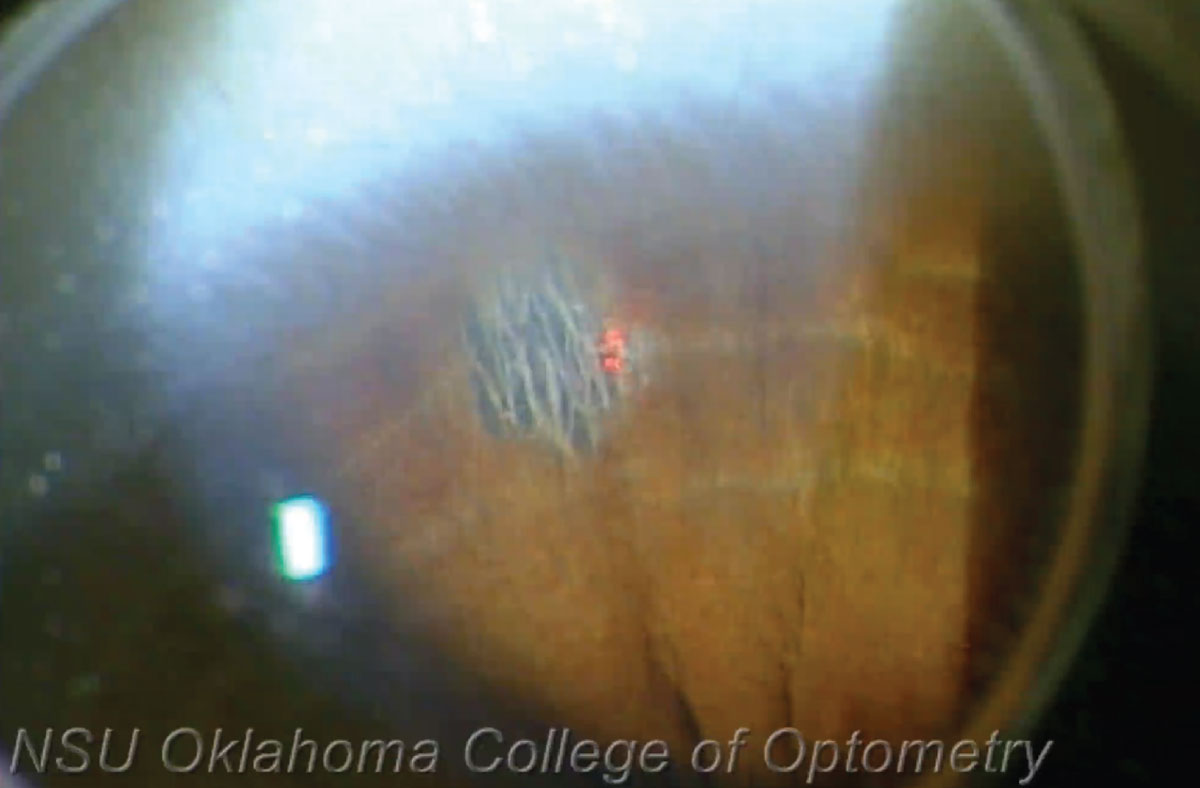
Change in endothelial cell count. Endothelial cells may be hit by the laser during an LPI (Figure 5), which can lead to decreased endothelial cell counts. One study comparing endothelial cell density in eyes who underwent LPI compared with control eyes showed no statistical difference between the groups.15 Another study compared eyes treated with LPI vs. phacoemulsification and found the LPI group to have a greater decrease in endothelial cell count than the phaco group.16 Proper laser beam alignment on the iris can avoid this.
 |
|
Fig. 5. Endothelial cell hit during YAG LPI. Click image to enlarge. |
Cataract development. Lenticular injury during an LPI may lead to the development of cataracts. Cataract progression was seen in 23% to 39% of LPI cases up to six years postoperatively.14 On the contrary, a subset of the ZAP study (Zhongshan Angle Closure Prevention Trial) published in 2022 showed that prophylactic Nd:YAG LPI did not cause significant cataract progression after six years in the 889 patients who received an LPI in one eye.17 This group concluded that LPI treatment of asymptomatic narrow angles does not increase the risk of developing clinically meaningful cataract worsening over time. Nevertheless, if cataract progression were to occur, patients should be referred to ophthalmology for management. Avoid lens damage by proper laser beam alignment on the iris.
Injections
The conditions of chalazion and blepharospasm both may be treated with injections (of different kinds) that carry with them potential side effects.
Intralesional Injection for Chalazion
Steroid injection for chalazia can be considered if more conservative options fail or if it is patient preference for treatment. It’s typically done with Kenalog (triamcinolone acetonide, Bristol-Myers Squibb). Intralesional injection is a beneficial option for chalazia near the lacrimal punctum and can resolve a chalazion in a little over two weeks.
Steroid deposition. This is a common complication after intralesional steroid injection (Figure 6). One study found an incidence of 92.3%, and these deposits remained for a mean of 18 days.20 One possibility to decrease steroid deposition risk is to use a lower concentration of triamcinolone. One risk factor for steroid deposition is darker skin, thus caution should be exercised in these patients.
 |
|
Fig. 6. Steroid deposition after intralesional triamcinolone injection for chalazion. Click image to enlarge. |
Depigmentation. Steroid injections can lead to skin depigmentation or fat atrophy at the injection site, more so with darker skin. These may self-resolve anywhere from seven to 12 months after injection, but it may be permanent.21,22 One study reported an incidence of 15%, but the patients in this study were pigmented patients.23 As depigmentation is a risk factor in darker skin tones, caution should be exercised with these patients.
Vascular occlusion. In very rare cases, intravascular injections may lead to retrograde infiltration, which could lead to a central retinal artery or vein occlusion. Two case reports have outlined individual patients who had a retinal and choroidal vascular occlusion after periocular injection of corticosteroid.24,25 Avoid this by injecting with low pressure to minimize retrograde arterial flow of steroid particles or by aspirating the needle and syringe, ensuring it isn’t in a blood vessel.
Botulinum Toxin for Benign Essential Blepharospasm
Botox can be a beneficial treatment option for patients with benign essential blepharospasm, with the effects lasting up to three months.
Eyelid ptosis. Upper eyelid ptosis, caused by the diffusion of the toxin into the levator palpebrae muscle, is a possible complication from toxin injection.26 The mechanism of action of botulinum toxin leads to the cessation of levator muscle activity.
Patients at risk for developing postoperative ptosis include those with levator function weakness and those with loose skin or an attenuated orbital septum, allowing easier diffusion of the toxin.26 Upper eyelid ptosis can occur 48 hours after injection or seven to 10 days after injection, and it usually resolves within two to six weeks.26 One study reported that ptosis complications occurred in one patient (3.6%) on the fourth day after injection and resolved in two months, while others reported ptosis rates of 9.2% to 10.3% after injection.27
If ptosis should occur, optional management may include use of apraclonidine 0.5% to stimulate Müller’s muscle and allow for minimal elevation of the upper eyelid.26,28 Techniques to avoid an upper eyelid ptosis include injecting at least 1cm above the bony supraorbital notch between the inner and outer canthi. Use higher concentration of botulinum toxin to allow for precise minimal volume injections and decreased risk of toxin migration to non-targeted areas.26
Surgical Procedures
Be aware of difficulties that can arise with chalazion incision and eyelid lesion removal.
Chalazion Incision and Curettage
When more conservative therapies or steroid injection fail to resolve a chalazion, surgical intervention with the procedure of incision and curettage can be considered. This intervention drains the contents of the chalazion and avoids recurrence, as the entire lesion and capsule are removed.
 |
|
Fig. 7. Ecchymosis after intradermal anesthetic injection before chalazion incision and curettage. Click image to enlarge. |
Ecchymosis. Eyelid bruising is common after chalazion incision and curettage (Figure 7). One study reported ecchymosis in 56% of patients with resolution in approximately five days.20 Monitor eyelid bruising for resolution, typically resolving one to two weeks after surgery.29 Ecchymosis can be prevented by avoiding anesthetic injection into eyelid blood vessels.
Meibomian gland damage. Incision and curettage risks tarsal plate and meibomian gland morphology alterations. If tarsus excision is performed too close to the eyelid margin, eyelid notching may occur. Be careful not to excise closer than 2mm to 3mm from the eyelid margin.30 Chronic meibomian gland obstruction and atrophy can occur if large horizontal incisions are made across many glands. Avoid this by keeping incisions vertical and parallel to the meibomian gland anatomy.30 If meibomian gland structure is affected and leads to instability of the tear film, manage it with treatments for evaporative dry eye, including warm compresses, eyelid scrubs, in-office heat therapies and lipid based artificial tears.29
Infection. This is a possibility with any surgery, but it can be minimized by maintaining aseptic technique throughout the procedure. Antiseptic agents such as povidone-iodine should be used in the preoperative preparation; prophylactic topical ophthalmic antibiotic ointment can be prescribed postoperatively. Should any postoperative infection occur, treat it with oral antibiotics such as Augmentin (amoxicillin-clavulanic acid, US Antibiotics) or cephalexin. Doxycycline, clindamycin or Bactrim (trimethoprim-sulfamethoxazole, Hoffmann-La Roche) can be used in cases of methicillin-resistant Staphylococcus aureus (MRSA).28,29
Suspected malignancy. Take caution with recurring or non-resolving chalazia, which may raise suspicion for malignancy. A recurrent chalazion should be biopsied to rule out malignancies such as sebaceous gland carcinoma and adenoid cystic carcinoma.31-33 Sebaceous carcinoma has a mortality rate of 23%, with 50% of these masquerading as benign or inflammatory lesions.29 They have a 20% risk of recurrence even after removal.29
Eyelid Lesion Removal with RF and Other Surgical Instruments
Radiofrequency removal of eyelid lesions is a quick and effective technique that results in great cosmetic outcomes and minimal to no scarring.
Infection. Likelihood of infection is very rare with removal of eyelid lesions via radiofrequency or other means (scalpel or surgical scissors). Maintain aseptic technique throughout the procedure with use of antiseptics such as povidone-iodine in the preoperative preparation; prescribe prophylactic ophthalmic antibiotic ointment postoperatively for one week.34 Should any postoperative infection occur, it can be treated with oral antibiotics.34
Excessive tissue excised. Scarring can occur if excision is performed too deeply.34 This can be avoided by using proper technique and remaining superficial with the radiofrequency device or other surgical instruments. Moist healing is also important in the postoperative period. Thankfully, scarring from radiofrequency is typically less pronounced than other surgical techniques. Use of a topical antibiotic ointment or other lubricating ointment will ensure the surgical site remains moist to aid healing and reduce scab or scar formation.34 One study reported a notch-shaped defect in four patients due to an over-resection, although these improved in three months postoperatively with a good cosmetic outcome.35
Takeaways
A doctor cannot truly master an interventional procedure until they are able to anticipate all possible complications and adjust on the fly to mitigate long-term consequences.
Educating patients about possible risks and complications is crucial before performing any laser or surgical procedure, and an informed consent form should be obtained before all. It is vital for optometric physicians to be aware of these possible complications and methods so they may use the proper tools and techniques to avoid them. Should complications occur, be sure to have protocols in place to allow for the best patient outcomes.
Dr. Komal Patel is an assistant professor at the Oklahoma College of Optometry (NSUOCO). She completed a Primary Care residency at NSUOCO specializing in ocular disease and advanced procedures. Dr. Patel is a diplomate of the American Board of Optometry and a fellow of the American Academy of Optometry. Dr. Nate Lighthizer is the associate dean, director of continuing education and chief of specialty care clinics at NSUOCO. He is a founding member and immediate past president of the Intrepid Eye Society. Dr. Lighthizer’s full disclosure list can be found here.
1. Ursell PG, Dhariwal M, O’Boyle D, Khan J, Venerus A. 5 year incidence of YAG capsulotomy and PCO after cataract surgery with single-piece monofocal intraocular lenses: a real-world evidence study of 20,763 eyes. Eye (Lond). 2020;34(5):960-8. 2. Freisberg LJ, Lighthizer N, Skorin Jr. L, Stonecipher K, Zimmerman AB. The Ophthalmic laser handbook. Lippincott Williams & Wilkins; 2021. 3. Bhargava R, Kumar P, Phogat H, Chaudhary KP. Neodymium-yttrium aluminium garnet laser capsulotomy energy levels for posterior capsule opacification. J Ophthalmic Vis Res. 2015;10(1):37-42. 4. Karahan E, Er D, Kaynak S. An overview of Nd:YAG laser capsulotomy. Med Hypothesis Discov Innov Ophthalmol. 2014;3(2):45-50. 5. Halilović EA. Correlation between eye aperture diameter and complications in the posterior eye segment after Nd-YAG capsulotomy. Bosn J Basic Med Sci. 2008;8(2):106-9. 6. Moussa G, Kalogeropoulos D, Ch’ng SW, et al. “Comparing outcomes of advanced nurse practitioners to ophthalmologists performing posterior YAG capsulotomy, a six-year study of 6308 eyes”. Eye (Lond). 2023;37(3):554-9. 7. Shaarawy TM, Sherwood MB, Hitchings RA, Crowston JG. Selective laser trabeculoplasty. Glaucoma. 2nd ed. London: Elsevier/Saunders; 2015. 8. Song J. Complications of selective laser trabeculoplasty: a review. Clin Ophthalmol. 2016;10:137-43. 9. Zhou Y, Aref AA. A review of selective laser trabeculoplasty: recent findings and current perspectives. Ophthalmol Ther. 2017;6(1):19-32. 10. Shi JM, Jia SB. Selective laser trabeculoplasty. Int J Ophthalmol. 2012;5(6):742-9. 11. Hirabayashi MT, Rosenlof TL, An JA. Comparison of successful outcome predictors for MicroPulse® laser trabeculoplasty and selective laser trabeculoplasty at 6 months. Clin Ophthalmol. 2019;13:1001-9. 12. Abe RY, Maestrini HA, Guedes GB, et al. Real-world data from selective laser trabeculoplasty in Brazil. Sci Rep. 2022;12(1):1923. 13. Shaarawy TM, Sherwood MB, Hitchings RA, Crowston JG. Peripheral iridotomy for angle-closure glaucoma. Glaucoma. 2nd ed. London: Elsevier/Saunders; 2015. 14. Radhakrishnan S, Chen PP, Junk AK, Nouri-Mahdavi K, Chen TC. Laser peripheral iridotomy in primary angle closure: a report by the American Academy of Ophthalmolgy. Ophthalmology. 2018;125(7):1110-20. 15. Kumar RS, Baskaran M, Friedman DS, et al. Effect of prophylactic laser iridotomy on corneal endothelial cell density over 3 years in primary angle closure suspects. Br J Ophthalmol. 2013;97(3):258-61. 16. Park HYL, Lee NY, Park CK, Kim MS. Long-term changes in endothelial cell counts after early phacoemulsification vs. laser peripheral iridotomy using sequential argon:YAG laser technique in acute primary angle closure. Graefes Arch Clin Exp Ophthalmol. 2012;250(11):1673-80. 17. Chang DST, Jiang Y, Kim JA, et al. Cataract progression after Nd:YAG laser iridotomy in primary angle-closure suspect eyes. Br J Ophthalmol. 2023;107(9):1264-8. 18. Liyanage SE, Kumaran N, De Alwis D. Macular burns resulting from the accidental use of selective laser trabeculoplasty mode during a laser capsulotomy. Br J Ophthalmol. 2014;98(1):141-2. 19. Ledesma-Gil G, Yannuzzi LA, Freund KB, Mainster MA. Dual-mode capsulotomy and selective laser trabeculoplasty lasers continue to cause severe, permanent macular injuries. Ophthalmology. 2020;127(12):1766-8. 20. Korn BS, Kikkawa DO. Video atlas of oculofacial plastic and reconstructive surgery. 2nd ed. Elsevier; 2017. 21. Park J, Chang M. Eyelid fat atrophy and depigmentation after an intralesional injection of triamcinolone acetonide to treat chalazion. J Craniofac Surg. 2017;28(3):e198-e9. 22. Ahmad S, Baig MA, Khan MA, Khan IH, Janjua TA. Intralesional corticosteroid injection vs. surgical treatment of chalazia in pigmented patients. J Coll Physicians Surg Pak. 2006;16(1):42-4. 23. Nabie R, Soleimani H, Nikniaz L, et al. A prospective randomized study comparing incision and curettage with injection of triamcinolone acetonide for chronic chalazia. J Curr Ophthalmol. 2019;31(3):323-6. 24. Yağci A, Palamar M, Eğrilmez S, Sahbazov C, Ozbek SS. Anterior segment ischemia and retinochoroidal vascular occlusion after intralesional steroid injection. Ophthalmic Plast Reconstr Surg. 2008;24(1):55-7. 25. Thomas EL, Laborde RP. Retinal and choroidal vascular occlusion following intralesional corticosteroid injection of a chalazion. Ophthalmology. 1986;93(3):405-7. 26. Collier H. Ptosis explored: a known complication following facial botulinum toxin injections. J Aesthetic Nurs. 2013;2(1):8-17. 27. Okumus S, Coskun E, Erbagci I, et al. Botulinum toxin injections for blepharospasm prior to ocular surgeries. Clin Ophthalmol. 2012;6:579-83. 28. Onofrey BE, Skorin Jr. L, Holdeman NR. Ocular therapeutics handbook: a clinical manual. Lippincott Williams & Wilkins; 2020. 29. Zeller JE. Keep an eye on chalazion. J Nurse Pract. 2022;18(9):943-6. 30. Dutton JJ. Atlas of oculoplastic and orbital surgery. 2nd ed. Lippincott Williams & Wilkins; 2018. 31. Salmon JF. Kanski’s clinical ophthalmology: a systematic approach. 9th ed. Elsevier; 2020. 32. Nema HV, Nema N. Ocular tumors. Springer; 2021. 33. Menon V, Deshmukh R, Mulay K. A rare masquerade of chalazion: adenoid cystic carcinoma. Indian J Ophthalmol. 2019;67(8):1371-3. 34. Fowler GC. Pfenninger & Fowler’s procedures for primary care. Elsevier; 2020. 35. Eshraghi B, Torabi HR, Kasaie A, Rajabi MT. The use of a radiofrequency unit for excisional biopsy of eyelid papillomas. Ophthalmic Plast Reconstr Surg. 2010;26(6):448-9. |

