 |
A middle-aged female presents with a minimally injected right eye of one days duration. She says her eye has been very itchy, and she admits to rubbing it a lot. There is a mild punctate epitheliopathy that appears consistent with a mechanical abrasion from the rubbing. However, she seems to be in a disproportionate amount of discomfort relative to the condition. She is diagnosed with allergic conjunctivitis and prescribed a topical steroid and antihistamine.
She returns the next day reporting significantly more discomfort. Biomicroscopy reveals a greater amount of punctate epitheliopathy and a great increase in focal stromal edema. Inspection of past records reveals a history of non-descript recurrent epitheliopathy in her right eye only. She also has a large herpetic cold sore on her lip. She is now diagnosed with herpetic disciform keratitis. The topical steroid is continued, and Viroptic (trifluridine, Monarch Pharmaceutical) is prescribed prophylactically.
She returns the following day with 80% of her epithelium eroded. An atypical adverse reaction to Viroptic is suspected, and the medication is immediately substituted with oral acyclovir while the steroid is maintained. But, through the next several days, the patients cornea continues to worsen with profound epithelial erosion and subsequent stromal infiltration, despite discontinuation of all topical medications, the use of non-preserved tears and a bandage soft contact lens. With her cornea thinning and the condition worsening, the patient sees an ophthalmologist. However, despite the ophthalmologists best efforts,the patients cornea continues to deteriorate.
Curiously, the patient begins to alternate office visits between practitioners, presenting as an emergency in one office even though she has an appointment at the other. Despite everyones best efforts, her cornea fails to heal.
Finally, when all diagnostic options appear to have been exhausted, a curious finding is noted during one of the patients visits: There are no proparacaine bottles in the exam room. Upon direct confrontation, the patient admits to taking bottles from each office at every visit. This brings us to this months topic: the abuse of topical anesthetics.
Corneal Toxicity
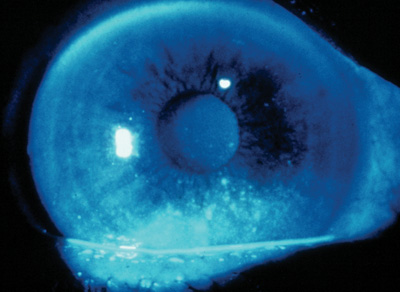
Corneal toxicity to topical anesthetics is a well-known phenomenon. Punctate epitheliopathy from topical medication toxicity in another patient.1-11 The toxicity affects the cornea in several ways. Proparacaine, for instance, has toxic effects on stromal keratocytes that are related to drug concentrations and temporal exposure.12 Proparacaine also appears to inhibit corneal epithelial migration and adhesion. Epithelial cell spreading is completely abolished, and most cells detach from the substratum with prolonged use, leading to corneal non-healing.13 Abuse of topical anesthetics also appears to produce irreversible damage to the apical cell attachments at the level of the corneal endothelial cells.14
The mechanism of corneal damage on a clinical level is unclear. Most likely, the abuse of topical anesthetics leads to a self-induced neurotrophic keratitis. Neurotrophic keratitis is characterized by impaired healing of the corneal epithelium due to interrupted innervation.15,16 When ocular surface sensation is impaired, reflex tear secretion is reduced, yielding an aqueous tear deficiency. Trophic input to the corneal epithelial cells also appears to be reduced, decreasing mitotic activity and further compromising healing mechanisms. Data on the neurotransmitter and neuropeptide contents of corneal nerves indicate that they are integral players in the mechanisms by which corneal neurochemicals and associated neurotrophins modulate corneal physiology, homeostasis and wound healing.17
 |
|
Punctate epitheliopathy from topical medication toxicity in another patient. |
Often, the diagnosis of topical anesthetic abuse is made ex juvantia (by exclusion) when all other treatments fail. This diagnosis is further complicated because patients often lie about abusing anestheticssomething to consider in the differential diagnosis of any keratitis that is unresponsive to treatment.20
Management
Management involves the total discontinuation of topical anesthetics by the patient and copious use of artificial tears. A bandage contact lens may be necessary. Topical NSAIDs, such as Voltaren (diclofenac, Novartis Ophthalmics), have been used for pain management while discontinuing topical anesthetics.19 Corneal transplantation is often necessary.
Psychiatric counseling may also be warranted here. The reasons patients abuse topical anesthetics vary. Some may seek to quietly self-induce injury and then sue a doctor for malpractice. Others may suffer from Munchausen syndrome, in which the patient enjoys the attention associated with illness. Most likely, patients simply dont appreciate the potential harm and potency of simple eye drops.
We learned early on in optometry school that patients may steal topical anesthetics from an exam room in order to self-medicate. As this scenario illustrates, it does happen. So, create safeguards in your practice to limit patient access to high-hazard pharmaceuticals, such as proparacaine.
Drs. Sowka and Kabat are members of Alcons speakers alliance. They have no financial interest in any of the products mentioned.
1. Rapuano CJ. Topical anesthetic abuse: a case report of bilateral corneal ring infiltrates. J Ophthalmic Nurs Technol 1990 May-Jun;9(3):94-5.
2. Sugar A. Topical anesthetic abuse after radial keratotomy. J Cataract Refract Surg 1998 Nov;24 (11):1535-7.
3. Varga JH, Rubinfeld RS, Wolf TC, et al. Topical anesthetic abuse ring keratitis: report of four cases. Cornea 1997 Jul;16(4): 424-9.
4. Kim JY, Choi YS, Lee JH. Keratitis from corneal anesthetic abuse after photorefractive keratectomy. J Cataract Refract Surg 1997 Apr;23(3):447-9.
5. Chern KC, Meisler DM, Wilhelmus KR, et al. Corneal anesthetic abuse and Candida keratitis. Ophthalmology 1996 Jan; 103(1):37-40.
6. Rocha G, Brunette I, Le Francois M. Severe toxic keratopathy secondary to topical anesthetic abuse. Can J Ophthalmol 1995 Jun;30(4):198-202.
7. Chen HT, Chen KH, Hsu WM. Toxic keratopathy associated with abuse of low-dose anesthetic: a case report. Cornea 2004 Jul;23(5):527-9.
8. Pharmakakis NM, Katsimpris JM, Melachrinou MP, Kolio- poulos JX. Corneal complications following abuse of topical anesthetics. Eur J Ophthalmol 2002 Sep-Oct;12(5):373-8.
9. Sun MH, Huang SC, Chen TL, Tsai RJ. Topical ocular anesthetic abuse: case report. Chang Gung Med J 2000 June;23(6): 377-81.
10. Webber SK, Sutton GL, Lawless MA, Rogers CM. Ring keratitis from topical anaesthetic misuse. Aust N Z J Ophthalmol 1999 Dec;27(6):440-2.
11. Rosenwasser GO, Holland S, Pflugfelder SC, et al. Topical anesthetic abuse. Ophthalmology 1990 Aug;97(8):967-72.
12. Moreira LB, Kasetsuwan N, Sanchez D, et al. Toxicity of topical anesthetic agents to human keratocytes in vivo. J Cataract Refract Surg 1999 Jul;25(7):975-80.
13. Dass BA, Soong HK, Lee B. Effects of proparacaine on actin cytoskeleton of corneal epithelium. J Ocul Pharmacol 1988 Fall;4(3):187-94.
14. Risco JM, Millar LC. Ultrastructural alterations in the endo-thelium in a patient with topical anesthetic abuse keratopathy. Ophthalmology 1992 Apr;99(4):628-33.
15. Bonini S, Rama P, Olzi D, Lambiase A. Neurotrophic keratitis. Eye 2003 Nov;17(8):989-95.
16. Lambiase A, Rama P, Bonini S, et al. Topical treatment with nerve growth factor for corneal neurotrophic ulcers. N Eng J Med 1998 Apr 23;338(17):1174-80.
17. Muller LJ, Marfurt CF, Kruse F, Tervo TM. Corneal nerves: structure, contents and function. Exp Eye Res 2003 May;76(5): 521-42.
18 Solomon A, Siganos CS, Frucht-Pery J. Presumed herpetic keratitis and topical anesthetic abuse. Acta Ophthalmol Scand 1996 Oct;74(5):518-9.
19. Dornic DI, Thomas JM, Lass JH. Topical diclofenac sodium in the management of anesthetic abuse keratopathy. Am J Ophthalmol 1998 May;125(5):719-21.
20. Ardjomand N, Faschinger C, Haller-Schober EM, et al. A clinico-pathological case report of necrotizing ulcerating keratopathy due to topical anaesthetic abuse. Ophthalmologe 2002 Nov;99(11):872-5.

