 |
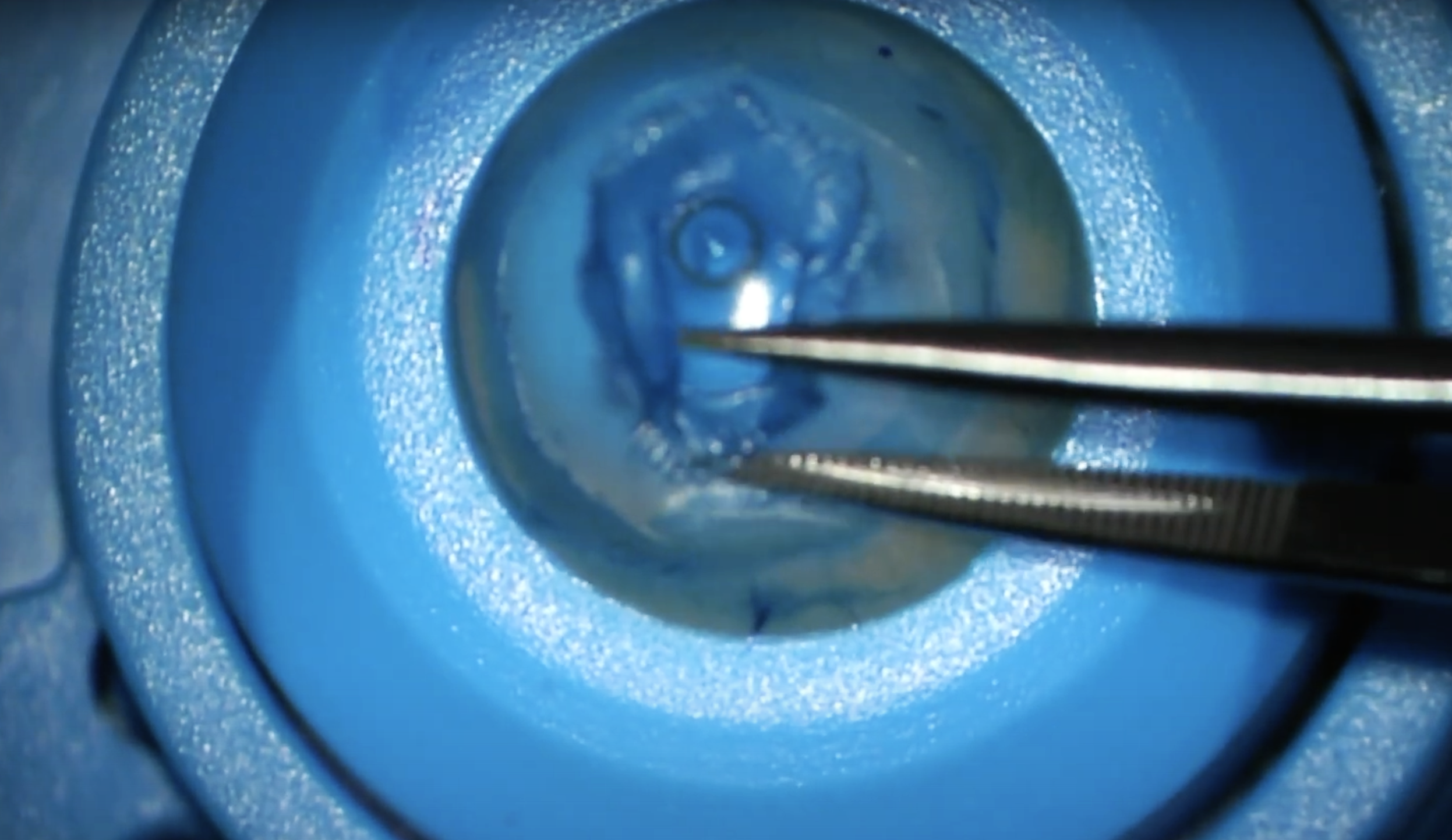
As an acellular graft, Bowman’s layer onlay grafting prevents the risk of micro-perforation and reduces the chances of allograft rejection. Photo: Brendan Cronin, MD. Click image to enlarge. |
Keratoconus is best caught in the subclinical stage when procedures such as corneal collagen cross-linking or intrastromal ring segment implantation can make a difference and strengthen the cornea. For advanced cases, transplants are often the only options.
In 2011, researchers proposed a less invasive alternative to DALK or PK for advanced keratoconus called Bowman layer (BL) inlay transplantation, which involved adding a donor BL inside a stromal pocket. Now, to avoid the challenges of thin cornea dissection such as perforation, they proposed BL onlay transplantation, where a BL graft is placed (“stretched”) onto the cornea after epithelial removal, allowed to dry in, and covered with a soft bandage lens until graft re-epithelialization. They conducted an interventional study using this minimally invasive epi-off approach and found that it produced good results while allowing for continued scleral contact lens wear.
In the prospective case series, 21 eyes of 20 patients with demonstrated keratoconus progression underwent BL onlay grafting. Patients were subdivided into less advanced (group 1, n=7) and more advanced (group 2, n=14) disease based on Kmax (69D cut-off). Mean follow up was 21 months. The researchers reported that all surgeries were uneventful.
There was an overall Kmax change from 76D preoperatively to 72D at six to 36 months postop. In group 2, Kmax decreased by 6D and didn’t change in group 1. The researchers observed that average best spectacle-corrected visual acuity remained stable in group 1 and improved postoperatively in group 2 from 0.8 to 0.4 logMAR. Best contact lens-corrected visual acuity remained stable.
Two eyes required graft repositioning after inadvertent bandage lens removal and four eyes required re-transplantation for incomplete re-epithelialization within the first postoperative weeks. One eye underwent re-grafting 12 months postoperatively after traumatic corneal erosion. At the last follow-up, all grafts had completely re-epithelialized.
The researchers concluded that BL onlay transplantation has “the potential to flatten far advanced keratoconic corneas without the risk of severe intraoperative complications since the technique is completely extraocular and has a diminished risk of allograft rejection due to the acellular character of an isolated BL membrane.” They also pointed out that this grafting technique doesn’t detract from the corneal donor tissue pool since BL onlay grafts can be prepared from donor corneas deemed unsuitable for DALK or PK.
“BL onlay grafting seems especially effective for patients with very steep and thin corneas who still have a subjectively acceptable visual performance with scleral lenses,” the researchers wrote in their paper. “This new technique may therefore be a promising alternative compared to more invasive treatment options for this challenging group of patients.”
Van der Star L, Vasiliauskaité I, Oellerich S, et al. Bowman layer onlay grafting as minimally invasive treatment for the most challenging cases in keratoconus. Am J Ophthalmology 2023. [Epub ahead of print]. |

