 |
A 65-year-old Caucasian female, who worked as an elementary school administrator, presented for an eye evaluation because of recent-onset ocular redness, lid swelling and watery/mucoid discharge, OU. Her symptoms began in the right eye two days prior, then developed in the left eye. She also reported a sore throat of approximately seven days’ duration.
Her ocular history was significant for silicone hydrogel contact lens wear, which she had discontinued two days prior to her visit. Her systemic history revealed hypercholesterolemia, for which she was properly medicated. She reported allergies to sulfur-based drugs and tetanus toxoid.
Clinical Findings
Her best-corrected acuities were 20/30 OD, 20/30 OS at distance and near. External examination was normal and there was no afferent pupillary defect. The pertinent anterior segment findings are demonstrated in the photographs.
There was a grade I cellular response in the right anterior chamber and a grade II response in the left. Notable were a small group of faint subepithelial infiltrates in the temporal right cornea. The balance of the biomicroscopic exam was normal OU and Goldmann applanation pressures measured 16mm Hg OU. The fundus evaluation was normal in each eye.
Additional testing included upper and lower eyelid eversion to examine the conjunctival surface for papillae, follicles and pseudomembrane formation; preauricular, submandibular, sublingual and submental lymph node palpation; sodium fluorescein examination of the anterior segments and corneal sensitivity testing.
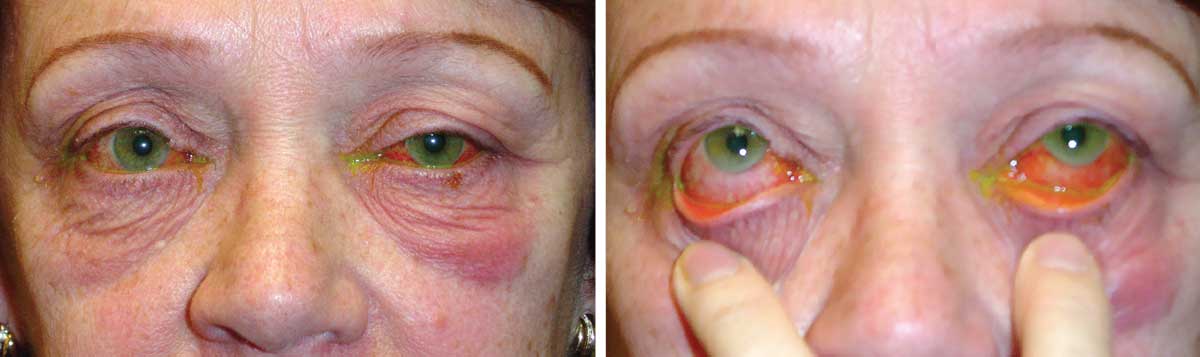 |
| How our patient presented at the clinic. What do these images suggest about her condition? Click to enlarge. |
Diagnosis
The condition presented in this month’s issue is pharyngoconjunctival fever (PCF) producing a secondary anterior iritis, OS > OD.
PCF is the result of an adenoviral infection, typically strains 3 or 7.1-5 It produces a follicular conjunctivitis with watery, mucoid discharge and red, edematous eyelids. Ocular symptoms include ocular itching and burning, foreign body sensation and a history of recent upper respiratory tract infection or close contact with someone with a red eye.5
Laboratory diagnostic testing may be considered but diagnosis is generally made based on clinical sequelae alone. Polymerase chain reaction (PCR) testing has been shown to provide rapid diagnosis of adenovirus infection and more recently a bedside immunochromatographic test has demonstrated a 95% sensitivity in detection of human adenovirus.2,4
Due to the sporadic nature of PCF, its frequency is difficult to assess. According to a study of 3,313 adenovirus isolates, only 1.7% represented cases of PCF.1 However, once PCF is released into a population it has the ability to progress to an epidemic level.3 There are multiple reported incidences at schools and summer camps with 40% absentee rate due to adenovirus 3.3
Proper care must be taken to inform patients about the contagious nature of PCF and to take proper precautions for at least one week following the cessation of symptoms.
Treatment is mainly supportive in the form of artificial tears, four to eight times daily. Cool compresses along with topical vasoconstrictors or mast cell stabilizing/antihistamine combinations, BID-QID, are also helpful.5 In the most severe cases, where a pseudomembrane is present, this must be removed. If there is bleeding, prophylactic topical antibiotic treatment can be considered to prevent bacterial superinfection. Topical steroids should be considered in cases where the subepithelial infiltrates reduce vision or when pseudomembranes are removed and increased inflammation exists. Cycloplegia may be necessary if there is concurrent iritis. Frequent hand washing and good personal hygiene are encouraged to prevent spread of the infection. Follow up should be scheduled at one to two weeks unless the condition worsens.
Intervention and Resolution
In this case, slit lamp exam revealed a moderate follicular conjunctival response OS>OD. There was no palpable preauricular lymphadenopathy or pseudomembrane formation. Laboratory diagnostic testing was not performed. It is likely that she contracted the virus from her work environment. The treatment included supportive therapy in the form of artificial tears and cool compresses as well as a topical antibiotic/steroid combination four times daily to reduce the signs and symptoms of inflammation and protect against bacterial infection.
In office, long-lasting cycloplegia was administered. The patient was advised to discontinue contact lens wear until the condition resolved and throw away her old lenses and case to avoid any contamination. She was also educated to the contagious nature of the condition and asked to abstain from reporting to work, taking extra caution with personal hygiene. The conjunctivitis, lid edema and iritis resolved over the course of nine days of treatment. At that point, the steroid combination was discontinued and she was allowed to return to work and resume contact lens wear.
Dr. Gurwood thanks Jason Price, OD, for contributing this case.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
| 1. Cooper RJ, Hallett R, Tullo AB, Klapper PE. The epidemiology of adenovirus infections in greater Manchester, UK 1982-96. Epidemiology and Infection 2000;125(2):333-45. 2. Fujimoto T, Okafuji T, Okafuji T, Ito M, Nukuzuma S, Chikahira M, Nishio O. Evaluation of a bedside immunochromatographic test for detection of adenovirus in respiratory samples, by comparison to virus isolation, PCR, and real-time PCR. J Clin Microbiol. 2004:42(12):5489-92. 3. Harley D, Harrower B, Lyon M, Dick A. A primary school outbreak of pharyngoconjunctival fever caused by adenovirus type 3. Communicable Diseases Intelligence. 2001;25(1):9-12. 4. Morris DJ, Cooper RJ, Barr T, Bailey AS. Polymerase chain reaction for rapid diagnosis of respiratory adenovirus infection. The Journal of Infection. 1996;32(2):113-7. 5. Rhee DJ, Pyfer MF. Acute Conjunctivitis. In : Rhee DJ, Pfyfer MF. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease, 3rd ed. Philadelphia, PA, Lippincott Williams and Wilkins 1999:121. |

