Referral to a neuro-ophthalmologist is fairly common when optic disc edema (ODE) arises. However, disc edema has various causes, each of which requires different workup. The goal of a research effort was to differentiate each cause of ODE in patients and multiple clinical characteristics of consecutive patients presenting at neuro-ophthalmology clinics.
Included in the retrospective study were 654 patients with ODE over a five-year period (70.6% women, mean age 41.2 years). Fundus photographs were obtained and clinical data of retinal nerve fiber layer thickness, best-corrected visual acuity (BCVA) and visual field mean deviation were retrieved.
The women were significantly younger than men (38.7 years vs. 47.6 years). After reviewing the data, the most common cause seen for ODE was idiopathic intracranial hypertension (IIH), making up 53.7% of cases. The other four most common causes were nonarteritic anterior ischemic optic neuropathy (NAION) contributing to 17.4%, non-IIH papilledema with 10.9%, optic neuritis with 7.0% and uveitis with 2.6%.
|
To learn more about papilledema and IIH, see this feature. |
The top three ODE causes in women only were IIH, non-IIH papilledema and NAION. For men, they were NAION, IIH and non-IIH. Of all the causes, visual acuity was worst at presentation for those with optic neuritis and best in those with IIH. Disc edema was found most severe in patients with non-IIH papilledema and least severe with optic neuritis. Despite this, those with non-IIH papilledema were not significantly different in visual acuity or visual field parameters at presentation compared with IIH papilledema. Those with papilledema, whether due to IIH or non-IIH etiology, had better visual function at presentation compared with the other top ODE causes.
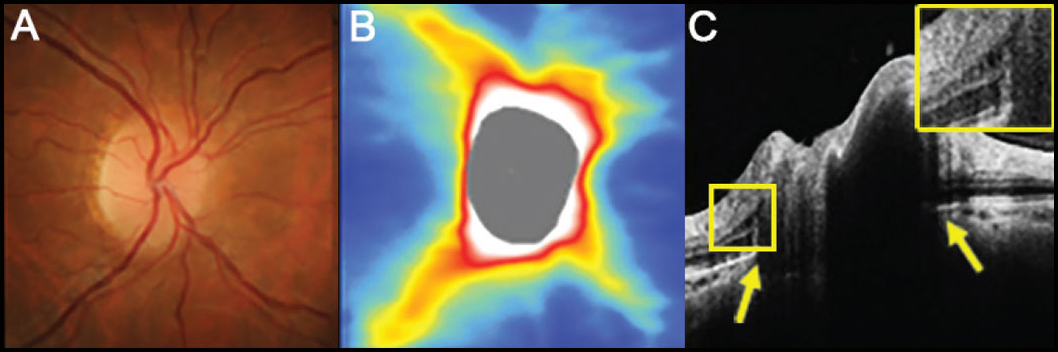 |
| The results of this study uniquely demonstrated that non-IIH papilledema cases have higher rates of disc edema, indicated through high RNFL thickness, when compared with NAION and optic neuritis. In figure (A), the disc has minimal visible cup with some subtle blurring of the superonasal disc margin. Figure (B) shows an OCT thickness heat map demonstrating thick superior and inferior RNFL while (C) presents a high-density OCT line scan shows anterior protrusion of Bruch’s membrane at its opening (yellow arrows) and intraretinal cystic spaces temporal to the disc margin (inset). Photo: Henrietta Wang, BOptom. Click image to enlarge. |
The study authors expanded on their findings in a paper for Journal of Neuro-Ophthalmology, highlighting that despite non-IIH presenting similarly to IIH in terms of BCVA and visual field mean deviation, it had higher rates of disc edema when compared with NAION and optic neuritis. NAION was the only condition seen at a higher rate among men and presented with much worse BCVA and visual field defects than papilledema. However, it still presented with equal visual deficits to optic neuritis.
The researchers argue that “our results reinforce the value of laterality in differentiating in the causes of ODE.” This is because papilledema most commonly presented with bilateral ODE, consistent with prior research. As well, IIH had a much greater proportion of bilateral cases than all other causes.
They continue that “our results suggest ODE severity can differentiate between etiologies, and a clinician may reasonably suspect optic neuritis and NAION to present with less severe ODE than papilledema. Moreover, non-IIH papilledema may present with greater ODE.” Together, these findings can better help clinicians distinguish, to some degree, the most common causes for ODE presentation.
Jhaveri A, Pandya B, Shamshad F, et al. The leading causes of optic disc edema seen in tertiary care, academic neuro-ophthalmology clinics. J Neuroophthalmol. January 12, 2024. [Epub ahead print]. |

