 |
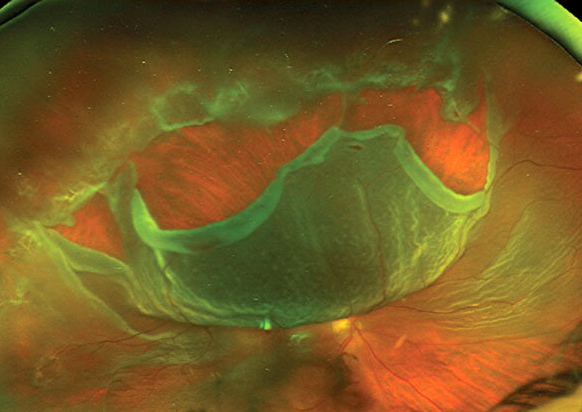
| A large dataset from Sweden found a sizable group of patients who went on to develop RRD could have been adequately served temporarily by a spectacle lens prescription until vision deteriorated further. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
With the rate of cataract surgery increasing comes an increase in complication post-op, such as rhegmatogenous retinal detachment (RRD). In a new study, Swedish researchers analyzed preoperative visual acuity to see if they could discern the risk of RRD after cataract surgery. They concluded that there must be strong indications of need for IOL implantation in those with a high risk of retinal detachment, and the patient must be given adequate information on the risk-benefit trade-offs. Many could get by adequately with spectacle correction, for instance, they argued.
Preoperative visual acuity in nearly 60,000 patients undergoing cataract surgery between during 2015 and 2017 was analyzed (n=58,624), with data retrieved from the Swedish National Cataract Register. This was then cross-referenced with patients undergoing surgery for retinal detachment at the Skåne University Hospital in Lund from 2015 to 2020. The main outcome was the risk-benefit ratio of measuring preoperative visual acuity before cataract surgery and the risk of RRD.
Groups were divided into the following: those aged 60 and younger, those aged 60 and younger with axial length over 25mm and male aged 60 and younger with axial length over 25mm.
In a previous study, the same group identified pseudophakic patients with a high risk of long-term complications such as RRD, especially men under the age of 60 with axial length exceeding 25mm who had almost 10% risk within five years. These patients should be thoroughly informed of the risks associated with cataract surgery, and the indications for cataract surgery should be strong.
In the group of patients under 60 years with an axial length over 25mm with a 6.4% risk of RRD in less than five years, more than 15% saw 0.8 or better. “The risk-benefit ratio is subjective to each patient, but in our opinion, these patients could have avoided cataract surgery and obtained the same improvement in vision with better spectacles,” the authors noted in the present study.
Between the group being small and the considerable variation in the visual acuity within the group, the authors noted it’s important to inform patients with relative good visual acuity that new spectacles may be an alternative to cataract surgery.
Also, in the same group more than 55% saw better than 0.5 logMAR, which used to be the indications in several regions for surgery, based on a 2010 study from Spain that found cataract surgery was usually deemed inappropriate in patients whose visual function was not impaired or only slightly impaired. In this new study, the patients with RRD had similar visual acuity in the operated eye as the whole study group, but there was a large difference in the fellow eye, where the RRD patients had better visual function.
“This indicates that cataract surgery is not necessary for many who have a risk for RRD as their binocular vision is still adequate,” the authors noted in their paper.
Many of the patients probably underwent cataract surgery on the eye with poorer vision, and then later on the better eye, especially in the case of myopic patients to avoid anisometropia. “Postoperative refraction must be considered when choosing the intra-ocular lens for the first eye to avoid putting them at risk for RRD with cataract surgery on the fellow eye,” the authors noted.
Although there are few complications during surgery and shortly after, based on these findings, the authors concluded that a greater awareness of the long-term risk of RRD is required in high-risk patients when considering cataract surgery.
“We illustrate in this study that many times the visual acuity for these patients is surprisingly good preoperative of cataract surgery where perhaps the best option for the patient is to wait with the surgery,” the authors concluded. “We hope that in the future there will be an individual risk assessment for each patient to consider before doing the surgery.”
Thylefors J, Jakobsson G, Zetterberg M, Sheikh R. Visual acuity prior to cataract surgery and risk of retinal detachment-a population-based study. Clin Ophthalmol. 2023;2023(17):1975-80. |

