 |
Q:
Several medications, such as amiodarone, quickly deposit in the cornea. Should I be concerned? Short of asking the prescriber to discontinue the drug, is there anything I can do to lessen the deposition and protect against acuity loss?
A:
“There’s really nothing you can do clinically to halt the progression of the verticillata relative to amiodarone—or other new agents, such as Vyzulta (latanoprostene bunod, Bausch + Lomb)—other than discontinue the drug,” says Jim Thimons, OD, medical director and founding partner of Ophthalmic Consultants of Connecticut. Fortunately, he says, acuity is most often unaffected.
These findings occur due to the deposition of cellular lipids in the basal epithelium secondary to the cationic amphiphilic properties of amiodarone and other drugs, Dr. Thimons explains. He notes, however, that in cases of severe symptomatology, an option is to debride the epithelium because the deposits are above Bowman’s membrane. A new corneal surface will grow, improving vision and reducing the verticillata, if only transiently. If a patient continues taking the drug after their epithelium is debrided, Dr. Thimons says the verticillata will grow back, so intermittent debridement may be necessary.
Putting Things Into Perspective
“I have never had an experience where the reduced acuity was solely from or significant enough because of the verticillata that I’ve had to do much other than observe,” Dr. Thimons says, adding that the idea that amiodarone severely impacts vision is misleading. While the drug rarely affects acuity related to verticillata, it is possible to demonstrate decreased acuity as a result of optic neuropathy—a rare but noted side effect.
Throughout his extensive time in clinical practice, Dr. Thimons has seen a significant number of amiodarone patients. Of those, he only rarely had to intervene and debride the epithelium.
“The acuity issue has not been a big concern, at least in my experience,” he says.
He adds that many of these patients have other issues that are both related (ocular surface disease) and unrelated to the drug and can cause acuity problems, such as cataract or macular disease.
The observed frequency of new amiodarone patients has declined in Dr. Thimons’ area of the country. He notes that the drug isn’t used as commonly because of competing agents that are being marketed as having fewer side effects (Multaq/dronedarone).
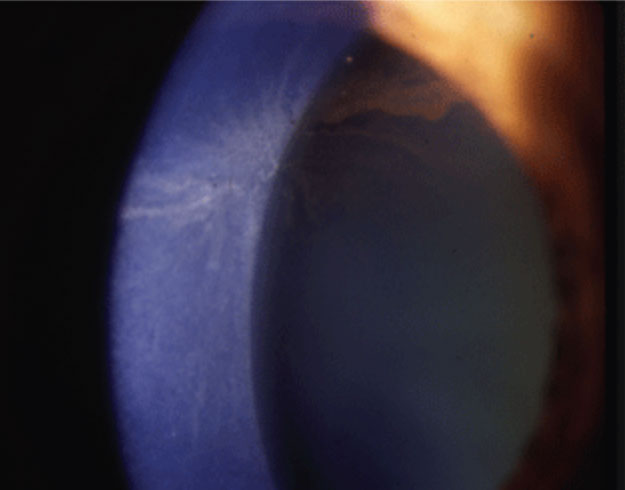 |
| Amiodarone causes corneal verticillata. Photo: Jay S. Pepose, MD, PhD. Click image to enlarge. |
Working With Limited Options
Because amiodarone is intended for cardiac intervention and persistent ventricular fibrillation, Dr. Thimons recommends continuing drug therapy to avoid putting patients at cardiac risk.
“You tolerate the ocular symptomatology because the risk associated with cessation is actually quite real,” he notes.
There are two steps Dr. Thimons would take, including maximizing the ocular surface.
“In patients with this treatment regimen, I would have no difficulty believing that the ocular surface is compromised as well, in that one of the more common side effects of the drug is dry eye,” he says. “If you maximize the surface, you’ll improve the overall visual function without having to be more aggressive with the management of the amiodarone complications.”
The other is removing any cataracts that are present. Dr. Thimons notes that cataracts exacerbate effects on vision in patients with pre-existing corneal issues. Taking them out of the equation, he adds, will improve overall visual function without having to interfere with the amiodarone therapy, which could cause significant cardiac risk.

