 |
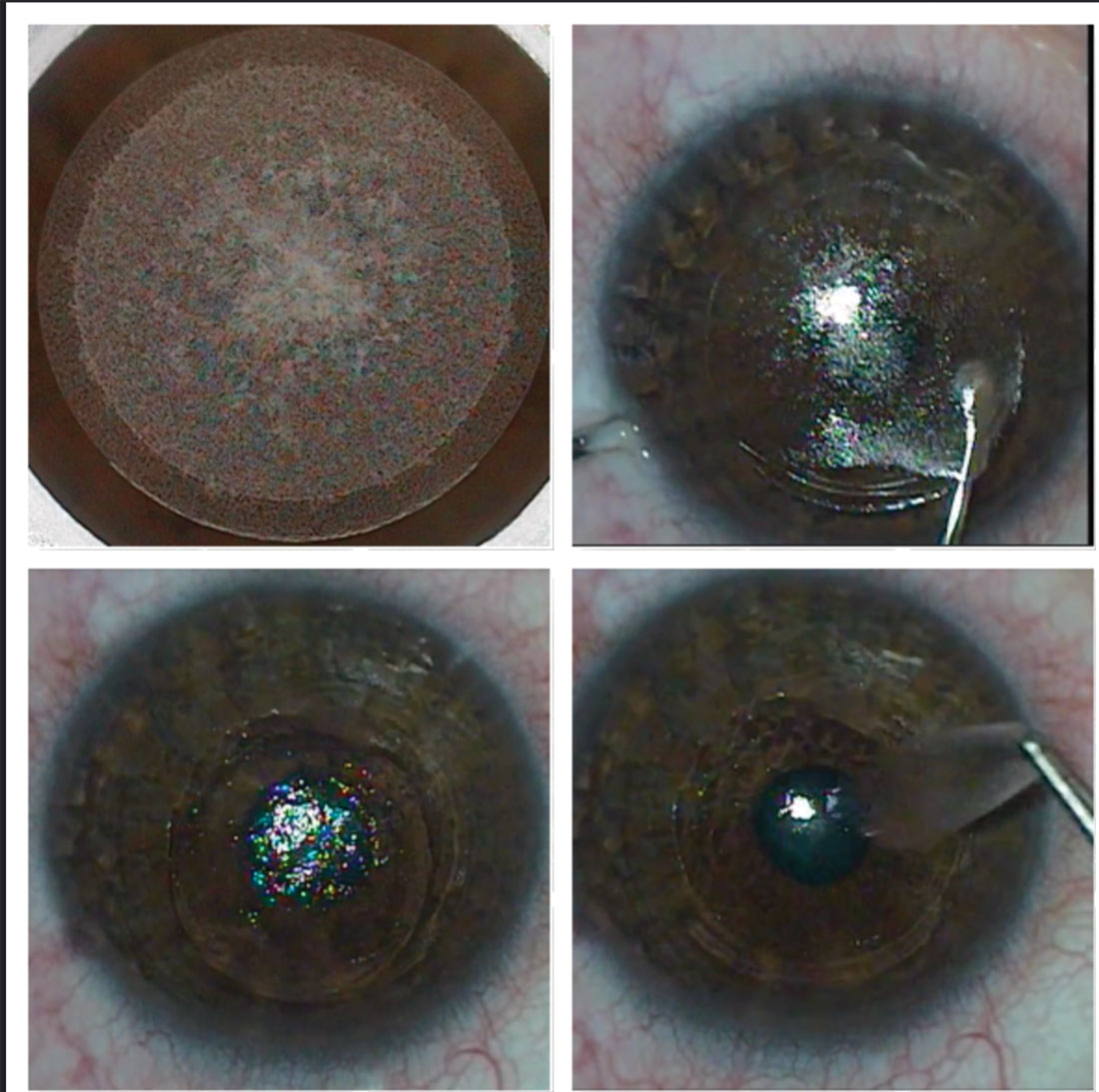
| Study suggests using a thinner cap to achieve a thicker residual stromal bed and a lesser decrease in corneal biomechanical strength in the SMILE procedure. Photo: Bobby Saenz, OD, Anthony Vanrachack, OD, and Alexandra Wiechmann, OD. Click image to enlarge. |
It’s been reported that flapless surgeries such as photorefractive keratectomy (PRK) and small-incision lenticule extraction (SMILE) result in fewer changes in corneal biomechanics than flap-based approaches such as LASIK. In a new study, researchers evaluated the change in corneal stiffness after these procedures.
Within each group, 120 eyes completed one year of postoperative follow-up. Age, gender, spherical equivalent and central corneal thickness–matched cases undergoing SMILE with a 120μm cap, LASIK with a 110μm flap and PRK were enrolled. One-year change in various metrics of corneal biomechanics were compared between the surgical groups.
The changes in all indices with SMILE were significantly greater than with LASIK and PRK, except the change in deformation amplitude ratio (posterior movement of the corneal apex) between SMILE and LASIK. No significant change was found in the stress-strain index (regional variation of corneal stiffness) with PRK. “Although the stress-strain index was designed to indicate material stiffness of the cornea with low correlation with the tissue’s geometric parameters or the IOP, it seems that the stress-strain index does not capture material stiffness fully when there are two layers of tissue that experience two different biomechanical stress environments (cap/flap vs. stroma),” the authors wrote in their paper.
A lower residual stromal bed target in the SMILE group and the 10µm difference between the cap and the flap explains the difference between the two procedures, they noted.
“In other words, the role of lower residual stromal bed thickness with smaller diameter of tissue removal in SMILE combined to generate the biomechanical changes despite the potentially greater stiffness in the cap vs. the flap,” the study authors explained. “This observation also explains why the decrease in the dynamic corneal responses in PRK was lower than in the other two procedures.”
A previous study reported greater biomechanical change with LASIK than SMILE. However, both flap and cap were matched at 90μm, both of which would have produced a greater residual stromal bed thickness than this study, which had much greater cap and flap thicknesses, the authors noted.
“This comparison is important because it indicates that, if the cap and flap thicknesses are matched, then LASIK shows greater biomechanical change than SMILE, with presumably similar residual stromal beds,” they explained. “Although SMILE preserves the greatest amount of anterior cornea with a cap thickness of 120μm, this also produces the smallest residual stromal bed and the greatest decrease in stiffness.”
The study concluded that the residual stromal bed is more important in determining stiffness decreases than the thickness of the cap in SMILE.
“When a thinner cap was used in a published study, LASIK showed greater biomechanical weakening than SMILE, which showed that, if residual stromal beds were similar between procedures, SMILE produces a fundamentally stronger result,” the authors explained. “Further evidence is given by PRK, the procedure that involved the removal of the anterior layer but maintained the thickest residual stromal bed, in which case there was less of a decrease in biomechanical stiffness of the cornea than in the other two procedures. Based on these findings, we suggest using a thinner cap, and hence a thicker residual stromal bed and a lesser decrease in corneal biomechanical strength, in the SMILE procedure.”
Hashemi H, Roberts CJ, Elsheikh A, et al. Corneal biomechanics after SMILE, femtosecond-assisted LASIK and photorefractive keratectomy: a matched comparison study. Vis Sci Technol. 2023;12(3):12. |

