2023 Pharma IssueIn the March issue of Review of Optometry, experts provide exciting updates on incoming dry eye treatments, oral steroid prescribing protocols and advancements in presbyopia management. Plus, learn how to fight insurance denials for new meds. Check out the other articles featured in this issue:
|
A top priority for any healthcare provider is ensuring optimal outcomes for their patients. However, restrictive drug formularies can make it difficult to execute the care plan of their choice. Prior authorization denials are a challenge seen across the continuum of care, and optometrists must be prepared to face the issue head-on. That’s often easier said than done when dealing with a problem that places undue burden on the entire clinical practice, including providers, staff and patients.
A recent 2021 AMA survey revealed that 88% of physicians characterized the burden associated with prior authorizations as high or extremely high. The survey also found that physicians and their staff spend an average of almost two business days—13 hours—each week completing prior authorizations. Additionally, survey participants reported that prior authorization often delays care and results in negative clinical outcomes.1
“Prior authorizations remain a major burden for doctors and patients alike. There are many times when I will write for an ophthalmic drop/medication only to have it denied and substituted for a generic without my consent,” notes Patrick Vollmer, OD, of Shelby, NC. “Insurance companies are making healthcare decisions for our patients—is the medication the doctor prescribes really medically necessary?”
Prior authorization denials frustrate both providers and patients and waste time, resources and money, emphasizes Dr. Vollmer. “Many doctors will quickly become exasperated with prior authorizations (and with good reason) and avoid them all together by writing for a generic drug from the beginning.”
So, what can optometrists do to contend with prior authorization denials and ensure their patients receive the necessary care at an affordable cost? This article will explore into the ins and outs of navigating this issue, including appeals, when to fight and when to change course, creative solutions and patient education.
 |
| Click image to enlarge. |
Navigating Insurance Hurdles
Taking a preemptive approach can help optometrists when working through the prior authorization process. In a busy clinical environment without a prior authorization specialist, Nova Southeastern’s Jessica Steen, OD, and colleagues do their best to anticipate and minimize potential medication challenges that could delay or prevent a patient from receiving a prescribed medication for a reasonable cost.
“This starts,” she notes, “by using the expertise of pharmaceutical sales representatives who have knowledge of the most current information of insurance carrier coverage in our area for specific products.”
“Given the frequent changes to insurance coverage, another option for ODs is to check EHR platforms to estimate cost beforehand,” suggests Joseph Shovlin, OD, of Scranton, PA.
Comprehensive documentation is critical to the prior authorization process. Dr. Steen emphasizes the need for clear and accurate records, including start and stop dates for each medication prescribed for a patient. If a medication was discontinued, optometrists should clearly describe and document the reason, such as failure to reach clinical effect, or include a description of the specific adverse event that led a patient to stop using the medication, she explains.
“For payers that have step-therapy policies, clearly organized information about previous medication failures and the specific reason for each failure supports your clinical decision-making and helps identify medical necessity of a prescribed medication,” Dr. Steen says.
“Current successful use of a chronic care product, whether that was a previously filled prescription or use of a professional sample with documented clinical success and patient tolerability, also help to support medical necessity of continued use of the product,” she adds.
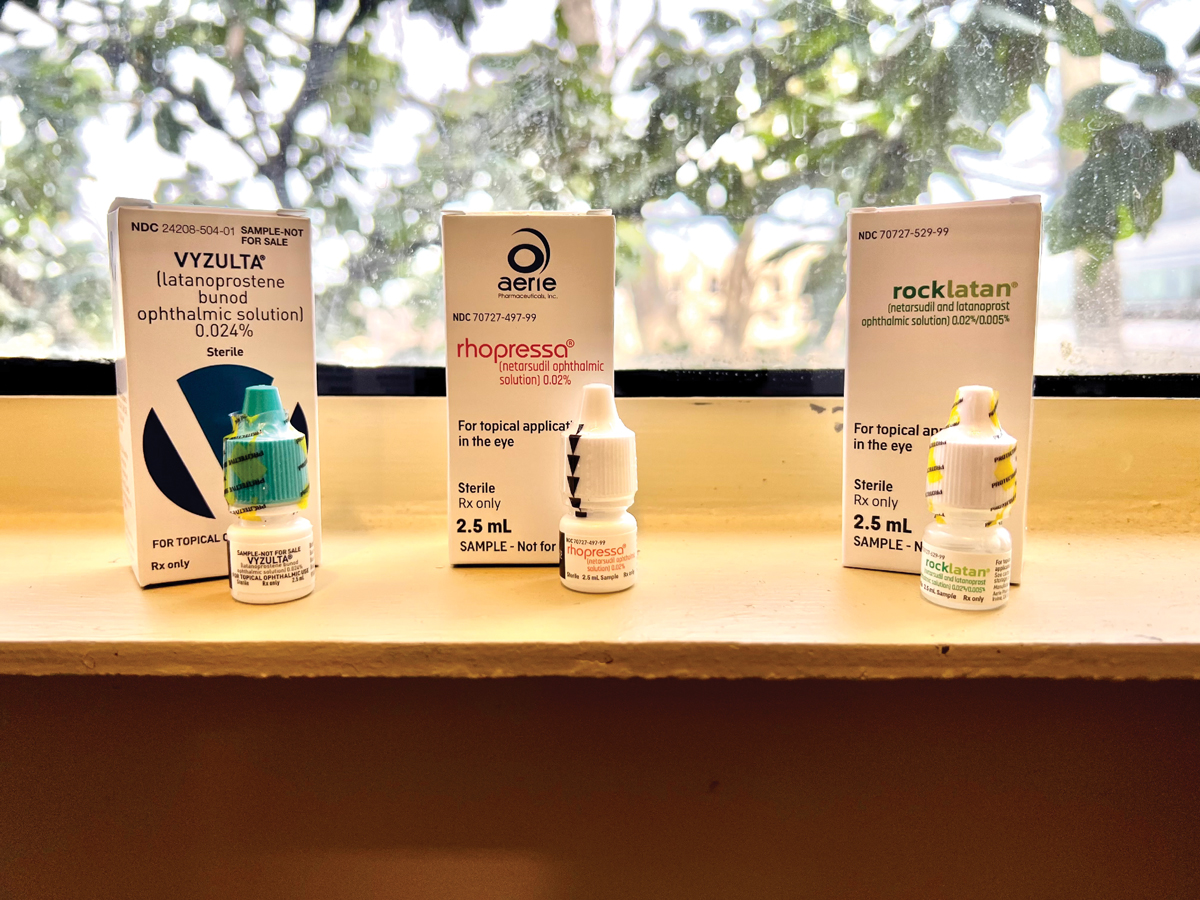
Another challenge ODs may have to deal with is continued adherence to medical therapy due to pre-specified quantity limits. “For example, a 2.5mL bottle of a prostaglandin analog may be the quantity limit for a 30-day supply for bilateral use,” says Dr. Steen.
“If the patient has difficulty successfully instilling the medication and requires the use of two drops to ensure that one makes it into the eye or they misplace a bottle, the patient may require more medication than the pre-specified quantity limit for continued use which may require additional communication with the payer,” she explains further.
It is also important that optometrists recognize that only prescribing generic medications does not guarantee that they will be able to avoid prior authorization requests, advises Dr. Steen, whose practice has received a number of prior authorization requests from a specific pharmacy benefit manager prior to coverage determination of generic latanoprost 0.005%.
“While the prior authorizations in these cases have been straightforward—asking only whether the indication for medication use is reduction of intraocular pressure (IOP) or treatment of a cosmetic condition—there is still an additional step which needs to be taken that may delay the patient’s ability to have access to a prescribed medication,” she notes.
 |
|
A shared-cost treatment model can end up being the best approach when treating conditions such as dry eye disease with the newest—and priciest—medications. Photo: Vin Dang, OD. Click image to enlarge. |
When to Appeal and Regroup
If a prior authorization is denied, prescribers have the opportunity to appeal the decision by submitting additional documentation. If the appeal doesn’t work but the drug is medically necessary, Dr. Steen recommends requesting a peer-to-peer discussion.
“The physician with whom you speak may not always be familiar with management of ocular conditions, current clinical best practices and standard of care, but they will be familiar with the specific criteria for medication coverage,” she explains, while noting that a peer-to-peer discussion gives optometrists the opportunity to communicate medical necessity.
This also gives the provider a chance to “describe the specific circumstances of the patient’s need, including their treatment history and the next steps in their care if the denial stands,” Dr. Steen says.
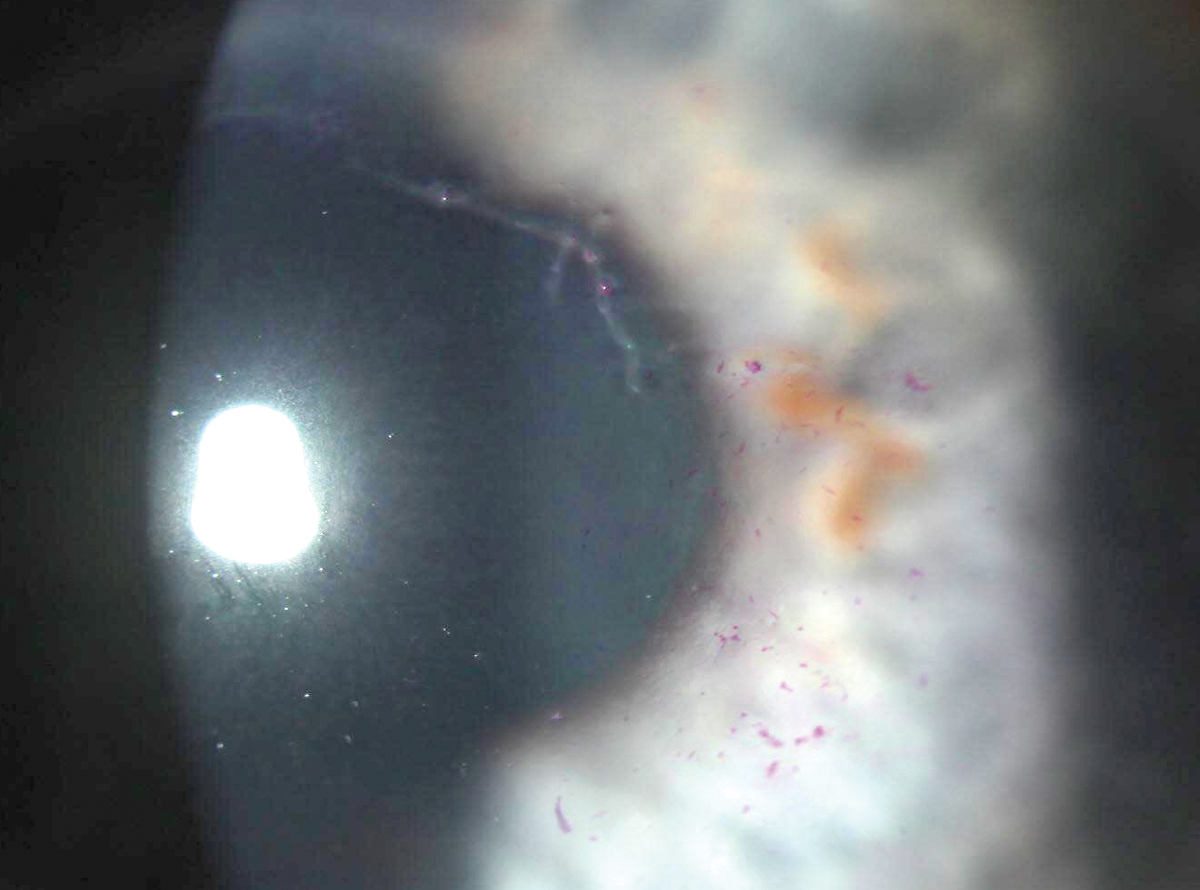
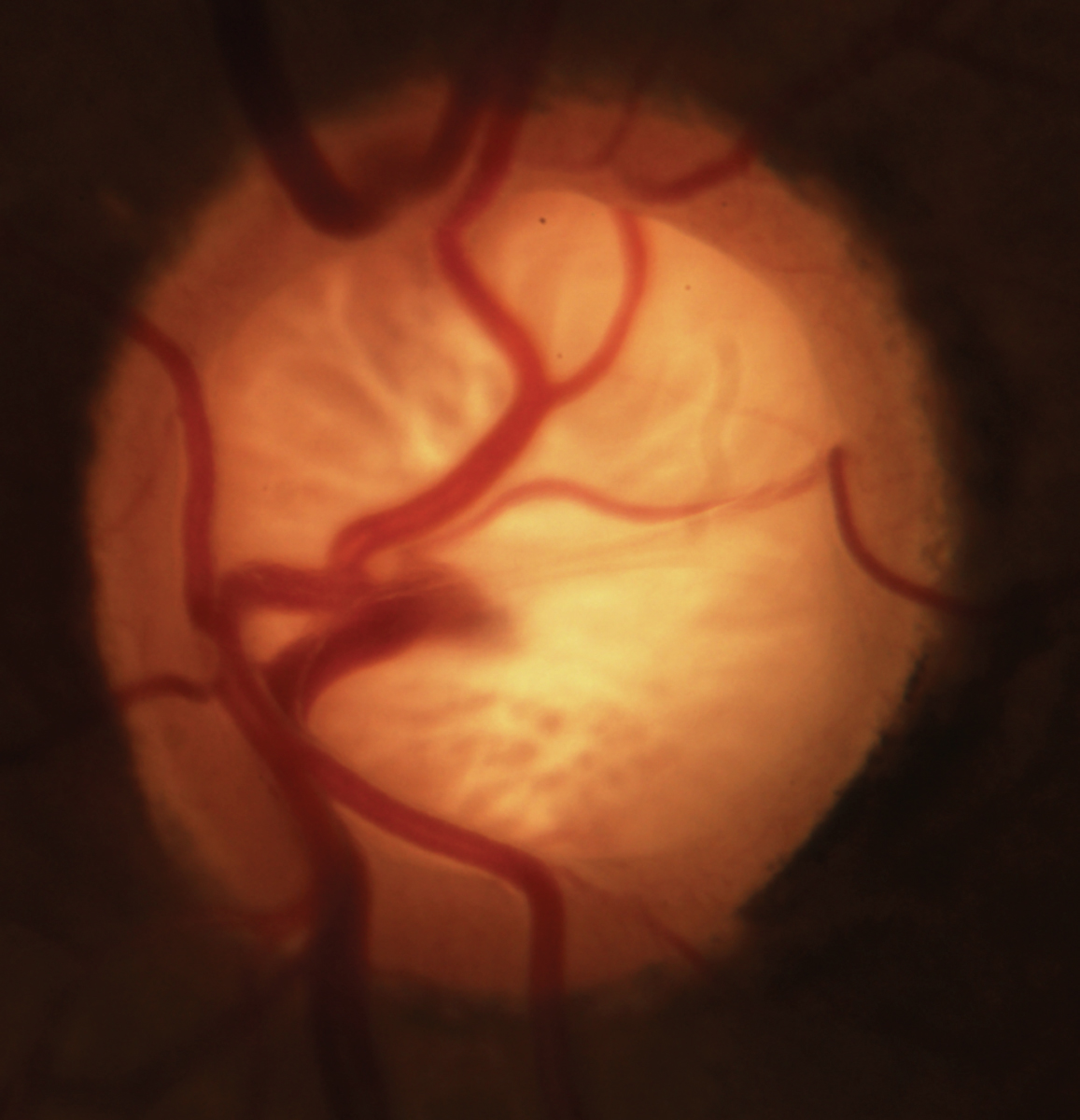
Optometrists must use their discretion and clinical experience to determine when an appeal is necessary and when a change in care plan is a better use of their practice’s time and resources. A prime example is glaucoma management.
“There is a significant cost to the patient, society and eventually the insurance company when the patient’s vision declines. There are increasing expenses for a patient who is declining in glaucoma vs. one who is stable and being managed at a simpler level of intervention,” says James Thimons, OD, of Meriden, CT. “And yet, the majority of doctors are being pushed to use a preset generic drug or panel of drugs by the insurance company: latanoprost, bimatoprost and travoprost.”
This makes it challenging to access newer agents in the space such as Rocklatan (netarsudil 0.02% and latanoprost 0.005%, Aerie) and Vyzulta (latanoprostene bunod 0.024%, Bausch + Lomb).
“The FDA trials clearly demonstrate that there’s a heightened level of efficacy in achieving more IOP control at higher levels with those two drugs than there is with latanoprost,” explains Dr. Thimons.
“And as we all know, every study and every doctor who speaks about glaucoma says every millimeter of IOP is important,” he continues. “These are not small numbers. These are two, three and four millimeter differences. That’s sight-saving and potentially life-changing for the patient if that drug works.”
When deciding what approach to take, ODs must decide whether or not the drug works for their patient and, unfortunately, the insurance company will often force the use of the generic product to prove inferiority, explains Dr. Thimons. In some instances, he notes, it may be worth starting with the generic.
“As the provider, you set the goal pressure for the patient, and then if you don’t meet that goal at four weeks, you move forward with a claim that the drug failed,” he says. “Detailed documentation is key and it must be entered into the medical record.”
He acknowledges that this isn’t a perfect system, but their practice has found success with this approach.
Before approving the branded agent, some companies may require ODs to add another agent to the generic drug. Another potential challenge is the issue of “soft steroids,” which insurance carriers often refuse to cover due to the higher cost.
“They may even want you to add an additional drop to lower IOP along with a generic topical steroid—that might raise IOP—instead of going with a medication less likely to cause an increase in pressure,” explains Dr. Shovlin.
 |
|
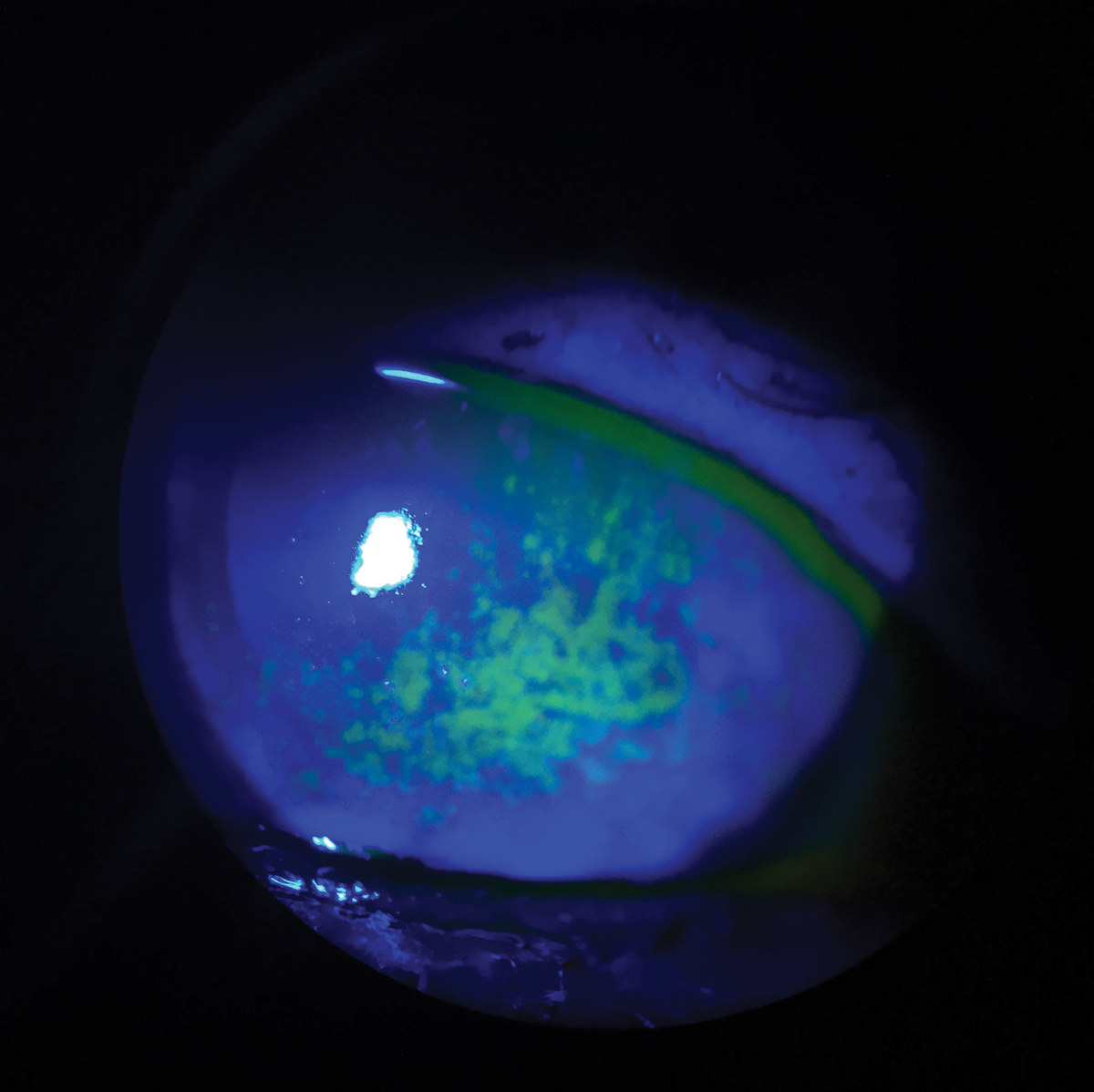
Prior authorization denials and associated delays can impact vision and outcomes. Antivirals used early are important in patients with herpes zoster ophthalmicus. Photo: Aaron Bronner, OD. Click image to enlarge. |
Given the demands of the prior authorization process, some ODs and their patients may even opt to proceed with selective laser trabeculoplasty, which is just as likely to be successful and is always covered by insurance, notes Dr. Thimons.
“Optometrists also need to understand that there is a percentage of patients who were not going to get covered regardless of how many times we pound on the door,” he advises. “In those cases, you will have to come up with alternatives. Cataract surgery is an outstanding system for lowering IOP, and in conjunction with a MIGS procedure can be incredibly effective.”
An example where appealing a prior authorization denial may not be the best course of action is ocular surface treatment.
“Dry eye may be a scenario where a lengthy battle with the insurance company is not the right avenue for you or your patient,” Dr. Thimons says. “While I am not arguing that we shouldn’t use the best products, this is a situation where it may be worth exploring other options. There are a number of ways that doctors can maintain the level of care that’s important for the patient without having to fight these battles all the time.”
A shared cost treatment model can end up being the best approach when it comes to the treatment of conditions like dry eye, suggests Dr. Thimons.
“Five hundred dollars for Restasis (cyclosporine 0.05%, Allergan) is sinful, but it happens every day in my practice. I think that is where doctors have to draw the line and come up with creative alternatives that are clinically proven and don’t have the associated costs of a variable pricing market from the manufacturers and pharmacies.”
As previously mentioned, prior authorization denials and the associated delays can have a significant impact on vision and outcomes. For instance, this is of particular concern, according to Dr. Shovlin, “when we need a good fluoroquinolone (later generation) for a corneal ulcer and the generic (first generation) is
offered.
“Also, antivirals used early are important in patients with herpetic disease,” he adds. “We have one carrier who only covers Viroptic (trifluridine 1%, Monarch) for epithelial herpes simplex, which we can’t even get because they don’t cover Zirgan (topical ganciclovir ointment, Bausch + Lomb), a newer medication.”
Fortunately, oral antiviral medications generally work as well as topical agents for epithelial herpes, Dr. Shovlin says.
 |
|
In glaucoma, “every millimeter counts” and sometimes that means fighting for access to the latest and most effective meds. Otherwise, vision will continue to decline and expenses ultimately will rise. Photo: Michael Dorkowski, OD, Jim Williamson, OD, and Andrew Rixon, OD. Click image to enlarge. |
Finding Creative Solutions
In cases where a prior authorization denial cannot be resolved—or fighting the decision is not the best use of resources—optometrists will have to find creative solutions to ensure the best possible outcomes for their patient.
Many pharmaceutical companies have discount or access cards that allow doctors to prescribe branded drugs, typically without a prior authorization, suggests Dr. Vollmer. For example, Bausch + Lomb’s Access Program allows patients to pay a flat fee for a variety of branded drugs that includes steroids, antivirals, antibiotics and glaucoma medications.
“Programs like this one are very beneficial because many times they limit or eliminate the need for a patient to fail on a generic medication first,” he says. “When I personally use this method, I find that pushback is greatly diminished. A piece of advice I can offer to all prescribers is this: get to know your independent pharmacists really well.”
Dr. Vollmer made a connection with one such individual in his community who is willing to take these access programs on and get his patients the drugs they need.
“I simply tell the patient, ‘This may not be the pharmacy you use, but this one will honor your access card.’ I never receive any patient pushback over this because they realize they are going to save a lot of money for a superior drug,” he notes. “The pharmacy is happy to do this because you are bringing them business. I have found that this ‘triangle’ is greatly beneficial for all parties.”
If all of these options fail and Dr. Vollmer has to prescribe a generic drug that is approved from the patient’s healthcare plan, such as generic prostaglandin instead of Vyzulta for a new glaucoma patient, he will make sure to see the patient back on regularly scheduled visits and check that the patient’s pressures are where they need to be.
“I may be forced to place the patient on dual therapy with another drug to get the pressures to target,” he says. “In some instances where I know the patient does especially well on a branded medication, I will save my samples for that patient to limit their financial burden. I have a 31-year-old in my clinic who I do this for, and he is very appreciative.”
As discussed above, dry eye is an area of care that can benefit greatly from out-of-the-box thinking. For instance, Dr. Thimons has used the Mark Cuban Cost Plus Drug Company—which aims to address rising drug costs—to get Restasis for his patients at a fraction of the cost a traditional insurance company charges.
Other options include programs such as GoodRx, which gathers current prices and discounts to help patients find the lowest cost for their prescriptions. Dr. Shovlin notes that ordering from Canada can work for some, but he acknowledges that it can be confusing for the patient and may not be the right approach for everyone. When doing this, he also emphasizes the importance of making certain you are ordering the same medications.
“This is the first legitimate agency to battle against this ridiculous cost override on the part of the pharmaceutical and insurance companies,” Dr. Thimons says. “We’ll see whether that plays out long-term, but that’s one of the alternatives that I use in the ocular surface space.”
When contending with prior authorization denials, Dr. Thimons has found that empowering patients to take the lead can prove successful. In cases where there is an issue with commercial insurance coverage, he has advised patients to connect with their HR departments. Dr. Thimons and colleagues will craft letters outlining the issue and their patients take it from there. When brought to their attention, HR departments can petition the insurance companies to expand coverage for specific medications or procedures.
 |
|
The majority of doctors are being pushed to use a preset generic drug or panel of drugs by the insurance company, making it challenging to access newer agents in glaucoma therapy. Photo: Abigail Kirk, OD. Click image to enlarge. |
Patient Education and Support
A key component of dealing with prior authorizations is educating patients and helping them understand the process. This goes a long way in building trust and avoiding upset patients who are blindsided by the cost of a prescription.
“Patient education is crucial, and especially important for patients with conditions like glaucoma who often are dealing with multiple medications,” says Dr. Thimons. “I will have a conversation with these patients from the beginning explaining their options.”
This includes a discussion about laser procedures and medication options as well as potential hurdles with insurance coverage.
“By doing this, I have prepared them for a potential preauthorization denial and discussed alternatives,” Dr. Thimons explains. “This preliminary discussion is probably one of the most valuable steps I have integrated into my clinic in the last 10 years, for both my practice and patients.”
Patient education for a condition like dry eye is different and sometimes more extensive because it is not as linear, according to Dr. Thimons. He begins these conversations by discussing the potential causes of their dry eye symptoms, and then advises the patient that there are a variety of pathways to treat this condition, but some may not be covered by their insurance.
“I emphasize the importance of tailoring an approach to meet their needs while making sure they understand that we may have to fight their insurance company, depending on coverage,” Dr. Thimons says. “I want to avoid getting an angry phone call from a patient because they are shocked when a drug we prescribed is $500. That is why I shifted my approach and take control of the conversation from the beginning.”
“I am going to be the one to deliver the bad news first,” he adds. “For the most part, I am very blunt. I cannot control what an insurance company does and doesn’t do, but I make it clear that I can work with my patients to still provide good care and here are our options. In the case of dry eye, that includes a discussion about shared cost options, omega-3 fatty acids, Regener-Eyes, autologous tears, interventional procedures and more. Dr. Thimons will also direct patients to educational resources.
Ultimately, you want to position yourself as not only an expert eyecare provider, but also as a patient advocate. By educating patients on potential insurance-related hurdles in advance, you are ensuring they are prepared while also making sure that they know you have their best interests in mind.
Prior authorizations can overwhelm clinical practices and have a significant impact on the entire care team as well as their patients. Having clear systems and plans in place can help mitigate some of the challenges associated with this issue.
“Avoiding burnout for your staff and yourself while also serving your patients is a very hard job these days,” notes Dr. Thimons. “Doctors are the emissaries in the middle of this battle. We don’t create the pricing, but we are responsible for our patients’ well-being. We know what works best and yet sometimes we’re denied. Navigating this challenge requires creative strategies, collaboration and support across the optometric profession.”
1. 2021 AMA prior authorization (PA) physician survey. American Medical Association. www.ama-assn.org/system/files/prior-authorization-survey.pdf. Accessed February 15, 2023. |


