 |
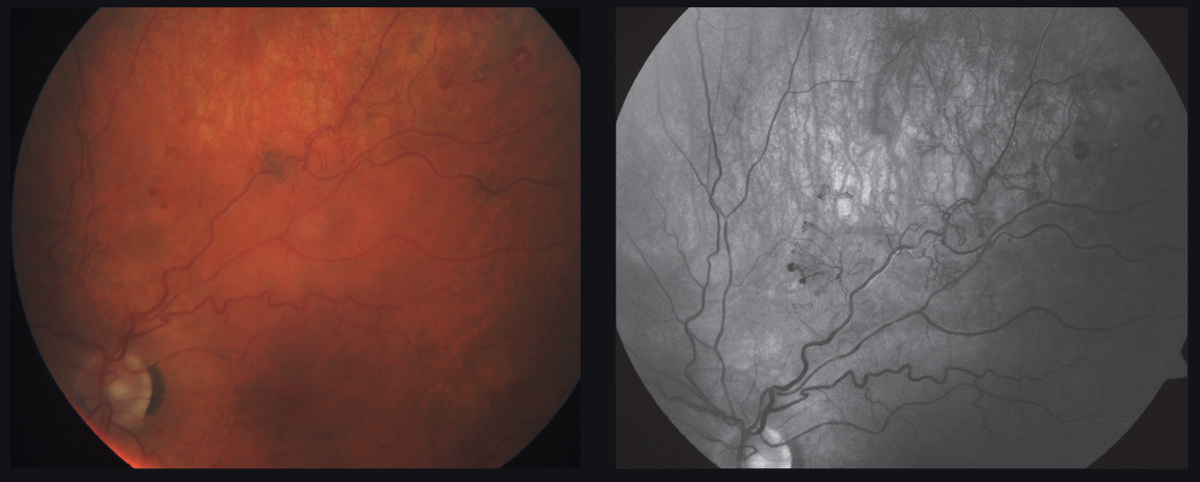
| Currently, not even evidence exists to support the claim that COVID-19 is associated with RVO. Photo: Carrie Ho, OD. Click image to enlarge. |
Retinal vascular occlusion as a potential result of COVID-19 infection has been a debated topic among the medical community; however, a critical analysis of recently published literature found that the link between the two is simply based on an assumption of a causal relationship rather than on supportive clinical evidence, which as of the time of this study, fails to demonstrate a true association.
The researchers performed a PubMed search for articles published between October 2020 and May 2021 using the following keywords: retinal vein occlusion (RVO), retinal artery occlusion (RAO), retinal vascular occlusion and COVID-19. Of the 31 articles that fit the criteria, the 17 that researchers used in the analysis included claims of a causal association with COVID-19. Among the reports, there were 10 cases of RVO (seven central RVO, one hemi-retinal vein occlusion [HRVO], one probable HRVO and one branch RVO), six cases of central CRAO and one case of cilioretinal artery occlusion.
A possible true association with COVID-19 was determined if patients had deranged coagulation and inflammatory parameters at the time of RVO with no confounding factors present, as these findings align with current knowledge about the virus pathophysiology.
After observing the methods and variables of each case report, the researchers concluded that most of the presumed associations between COVID-19 and RVO are weakened by the presence of comorbidities. Nine of the 17 patients in the case reports had comorbid conditions, the most common being hypertension, with others including non-insulin-dependent diabetes, hyperlipidemia, sickle cell disease, marijuana use, chronic smoking, hyperuricemia, polycystic ovarian disease (PCOD) and arsenic exposure.
“A previous case report had no venous tortuosity which is a major characteristic of central RVO,” the researchers wrote. “Furthermore, the eye had vitreous hemorrhage and HBA1c was 13% which points more toward diabetic retinopathy. The youngest patient, 17 years of age described by another study, had PCOD and history of arsenic intake in the form of a homeopathic medication as risk factors. Arsenic has been known to induce platelet aggregation and venous thrombosis. Furthermore, PCOD by itself is a cause of venous thrombosis.”
The researchers pointed out several other instances that could falsely suggest an association, such as in one report where patient findings simulated that of paracentral acute middle maculopathy more than those classically observed in central RAO.
All the inconsistencies and variables among the cases in this analysis show a weak association between COVID-19 and RVO. The researchers concluded, “Clinicians can continue to manage these patients according to the standard guidelines until there is more robust evidence to support this association to alter the diagnostic and treatment approach.”
Sharma A, Parachuri N, Kumar N, et al. Myths and truths of the association of retinal vascular occlusion with COVID-19. Retina. December 3, 2021. [Epub ahead of print]. |

