 |
A 62-year-old African-American male presented to the eye clinic for a glaucoma follow-up. Additionally, the patient reported that distance and near vision seemed blurrier, even though at his last eye doctor visit he changed his spectacles. According to his wife, he had been acting confused, not recognizing people he knew well. His past medical history was remarkable for hypertension, vitamin D deficiency, traumatic brain injury, cerebrovascular accident (left middle cerebral artery infarction) and heart disease. He was considered a glaucoma suspect because of slightly increased cup-disc ratios seen in both eyes.
Clinical Findings
The patient’s best-corrected entering visual acuities were 20/20 OD and 20/20 OS at distance and near. His external examination was normal and there was no evidence of an afferent pupillary defect. Confrontation visual fields demonstrated restriction in the left inferior quadrant OD and restriction in the left superior quadrant OS. Biomicroscopy found unremarkable anterior segments, both eyes with Goldmann applanation pressures measuring 13mm Hg OU.
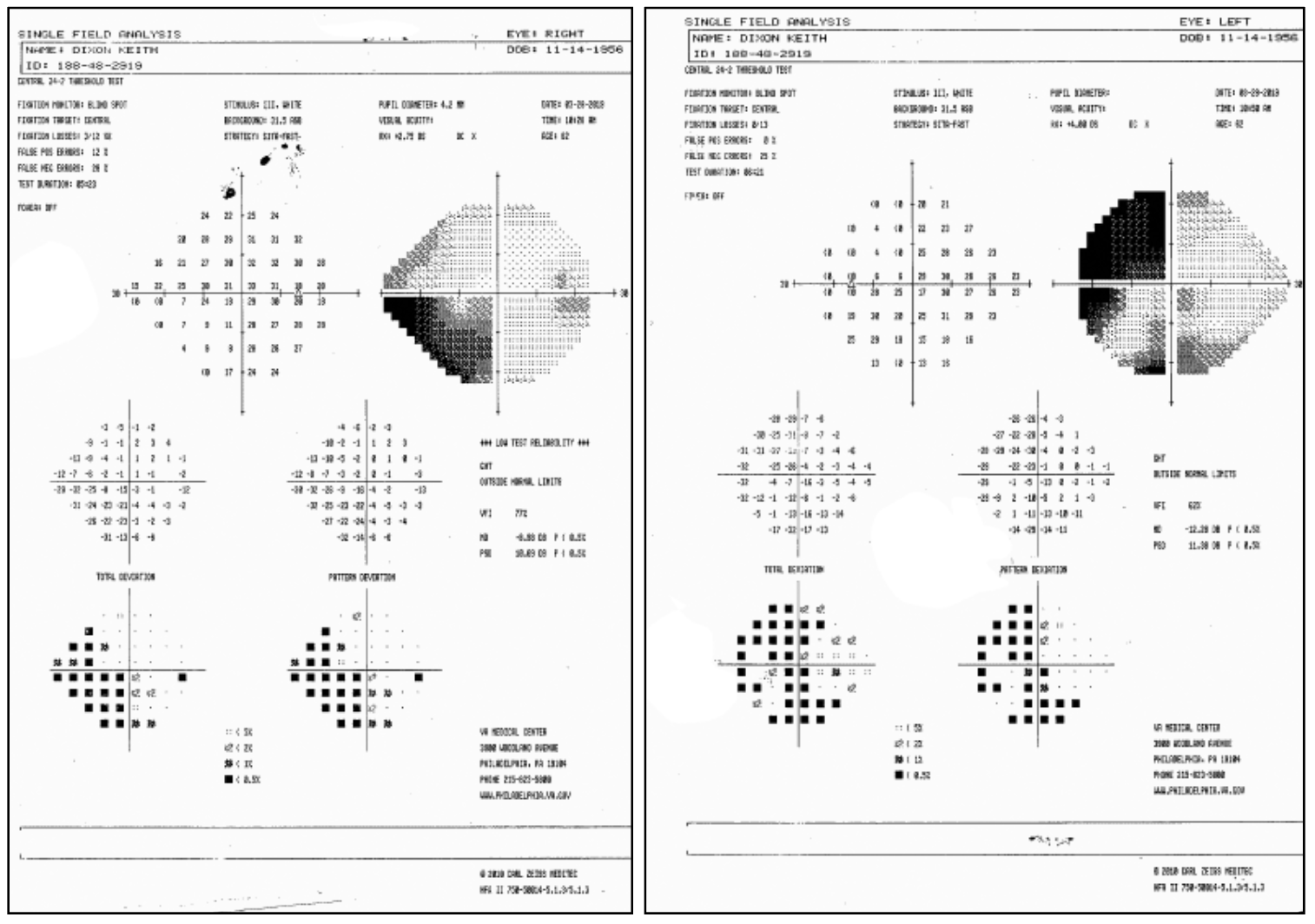 |
| The patient’s visual field results (OD at left, OS at right). Click image to enlarge. |
Additional studies included a glaucoma workup to rule out a conversion to the treatable form of the disease secondary to the slightly increased cup-disc ratios OU. This included optical coherence tomography OU and automated visual fields (see the printouts). The structural tests demonstrated normal nerve fiber layers, both eyes. Pachymetry was also completed, finding normal central corneal thickness (560µm).
Poor facial recognition was confirmed with photographs of family. Finally, a referral to neurology with the suggestion of neuroimaging to rule out new stroke was made.
Visual Field Disturbances
The diagnosis is crossed-quadrant homonymous hemianopsia (CQHH) also known as checkerboard visual field phenomenon. The neuroimaging uncovered multiple neurologic lesions.
Vertebro-basilar ischemia and bilateral lesions of the striate cortex can cause this significantly rare visual field defect.1-11 Other visual field defects associated with bilateral occipital lobe lesions include bilateral altitudinal defects, bilateral central homonymous hemiscotomas with macular sparing.11 These defects constitute less than 6% of homonymous visual field defects.5 Cerebrovascular accidents (CVA) in the occipital lobe are the most common etiology, followed by trauma and tumor.5,6
Visual disturbances and hallucinations may occur in CQHH.1 The visual field defect occurs typically from lesions that arise above the calcarine fissure on one side and below the calcarine fissure on the contralateral side. These classic defects can also occur via small lesions that are limited to the optic radiations.1 Vision can either be preserved or lost abruptly or gradually, but, in these cases the loss always respects the vertical meridian.1-15 The visual field defects may occur at the same time or at different times; they may be congruous or incongruous.1-11
It is common for patients to misinterpret their homonymous visual field loss as a monocular loss on the side where the vision defect is (if it’s a left homonymous loss, patients may interpret their vision issue to only be in the left eye). Given the possibility of that phenomenon and because of the way the afferent nerves are interdigitated in the visual pathway, bilateral visual field testing is always recommended; even in the setting of solely monocular complaints.6
Typically, patients with CQHH do not have central vision involvement; this is because anatomically, there is collateral blood supply to the occipital region which sub-serves detailed acuity.1 When central vision is affected, it is decreased symmetrically in both eyes.11 Typically, when simultaneous damage occurs to the occipital lobes, the vision loss occurs rapidly and can last for minutes to days or be permanent. In many cases, homonymous hemianopias improve significantly within days or remain stable after present for more than three months.11 Bilateral optic atrophy can occur via trans-synaptic neuronal degeneration.11
Other differential diagnoses that present with homonymous visual field deficits include CVA, tumor, trauma, vasospastic etiology (migraine) and inflammatory or infectious processes. Known risk factors for aneurysm include trauma, hypertension, atherosclerosis, prior CVA, tertiary syphilis, coronary artery disease and multiple sclerosis. Cardiovascular risk factors, especially disease to the basilar artery or vasculature near the heart, have the potential to cause bilateral occipital lobe lesions.11
Pathophysiology and Clinical Manifestations
Cortical blindness occurs when the visual pathway is disrupted. Here, the pupillary light reflexes remain intact because the optic tracts are spared.10 Anytime the brain is affected, other related neurologic phenomena may occur.
Anton syndrome is when patients deny that they have any visual disruption.10 Hallucinations can also arise from relatively small lesions of the occipital lobe.10 Patients may experience macropsia (things appear larger than they are) or micropsia (things appear smaller than they are).10 Objects may also appear to have blur around the edges or elongate, a phenomenon known as dysmetropsia.10 Color perception may change as well.10
Depending on how the brain is injured, patients may experience Balint’s syndrome (inability to visualize more than one object in the visual field at one time; an inability to identify different items in a visual scene simultaneously; they see the sink but not the dishes in the sink) or optic ataxia (the inability to accurately point to or reach for objects with an intact ability when directed by sound or touch; the patient can see an object may be unable to reach for it until they make physical contact it).
Agnosia is defined as an inability to process sensory information. The common forms of this include prosopagnosia (inability to recognize faces of familiar people) and simultagnosia (inability to see multiple objects at once; they can see a tree but not realize it’s in a forest).10
The posterior cerebral arteries have some association with 70% of strokes with homonymous hemianopia.13 Other sources of homonymous visual loss include traumatic brain injury, cerebral anoxia, lobectomy, arteriovenous malformation, cancer, degenerative disorders, and progressive multifocal leukoencephalopathy.13 These defects can significantly alter attention, perception and fixation within the visual system. This, in essence, can lead to hemianopic alexia (difficulty reading) and mobility dysfunction, particularly in unfamiliar environments.13 Moreover, patients with occipital lobe lesions can experience cerebral polyopia (seeing more than one image, often arranged in rows without having a strabismus), cerebral achromatopsia (lost color perception without retinal dysfunction), akinetopsia (motion blindness), palinopsia (recurrent visions of an object in the visual field), flashes of light, hallucinations and higher level disorders in the visual perception.11
An occipital infarction can cause dull pain over the ipsilateral brow via referred pain through the ophthalmic branch of the trigeminal nerve.11 Patients may also experience posterior reversible encephalopathy syndrome (PRES), resulting in intermittent headaches, confusion, epilepsies and vision loss.11
After a CVA in the occipital lobe has occurred, the risk of a second infarction is 16% within six months.11
Our Case
Once it was clear that the local diagnosis of open-angle glaucoma was not plausible, the patient was referred to neurology. With imaging, the appropriate but rare diagnosis was uncovered. The current goal is slowing or stopping cognitive decline and to reduce the risk of additional events. A vision rehabilitation referral was also made to improve quality of life.
Dr. Gurwood thanks Felicia Cicco for her contributions to this manuscript.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
|
1. Cesareo M, Pozzilli C, Ristori G, et al. Crossed quadrant homonymous hemianopsia in a case of multiple sclerosis. Clin Neurol Neurosurg. 1995;97(4):324-327. 2. Sachdev MS, Kumar H, Jain AK, et al. Transsynaptic neuronal degeneration of optic nerves associated with bilateral occipital lesions. Indian J Ophthalmol. 1990;38(4):151-152. 3. Dumitrascu A, Nohai I, Stoica S, et al. Psycho-cognitive syndrome, blindness and tetraplegia after severe traumatic brain injury in polytraumatic context (road acc.) with favorable recovery of cognitive and motor deficits. Balneo Research Journal. 2018;9(3):343-345. 4. Hokazono K, Ribeiro-Monteiro ML. Homonymous quadrantic macular ganglion cell complex loss as a sign of trans-synaptic degeneration from occipital lobe lesion. Am J Ophthalmol Case Rep. 2018;13(3):76-79. 5. Papageorgiou E, Anthis N, Stathi T, et al. Case series: bilateral homonymous visual field defects due to bilateral ischemic strokes. Optom Vis Sci. 2018;95(11):1077-1082. 6. Kamal S, Al-Othman B, Bayan K, et.al. Checkerboard Visual Field Defect in Occipital Stroke. Journal of Neuro-Ophthalmology. 2020;40(2):13-14. 7. Hamilton R, Keenan JP, Catala M, Pascual-Leone A. Alexia for Braille following bilateral occipital stroke in an early blind woman. Neuroreport. 2000;11(2):237-240. 8. Ogawa K, Ishikawa H, Suzuki Y, et al. Clinical study of the visual field defects caused by occipital lobe lesions. Cerebrovasc Dis. 2014;37(2):102-108. 9. Conforto AB, de Souza M, Puglia P Jr, et al. Bilateral occipital infarcts associated with carotid atherosclerosis and a persistent hypoglossal artery. Clin Neurol Neurosurg. 2007;109(4):364-367. 10. Kirmani M, Garg M, Sharma P. Parietal and occipital lobe syndromes: neuropsychological approach. International Journal of Indian Psychology. 2016;3(2):1-8. 11. Fraser JA, Newman NJ, Biousse V. Disorders of the optic tract, radiation, and occipital lobe. Handb Clin Neurol. 2011;102(1):205-221. 12. Pöppel E, Brinkmann R, Von Cramon D, Singer W. Association and dissociation of visual functions in a case of bilateral occipital lobe infarction. Arch Psychiatr Nervenkr. 1978;225(1):1-21. 13. Chokron S, Perez C, Peyrin C. Behavioral consequences and cortical reorganization in homonymous hemianopia. Front Syst Neurosci. 2016;10(57):1-12. 14. Arcaro MJ, Thaler L, Quinlan DJ, et al. Psychophysical and neuroimaging responses to moving stimuli in a patient with the Riddoch phenomenon due to bilateral visual cortex lesions. Neuropsychologia. 2019;128(5):150-165. 15. Danchaivijitr C, Kennard, C. Cortical visual disorders—functional localization and pathophysiology. Blue Books of Neurology. 2008;32(1):332-356. |

