 |
Now that we know meibomian gland dysfunction (MGD) is a common contributor to ocular surface disease, we can apply a number of new treatments that directly address the unique biology affected. From supplements and lid hygiene to in-office debridement and expression therapies, MGD treatment continues to evolve.
One approach, intense pulsed light (IPL) therapy—an off-label use of an FDA-approved device—has become more mainstream for patients with confirmed MGD, particularly if they also present with rosacea. The technology is now on its second iteration with the advent of low-level light therapy (LLLT), a new two-step approach.
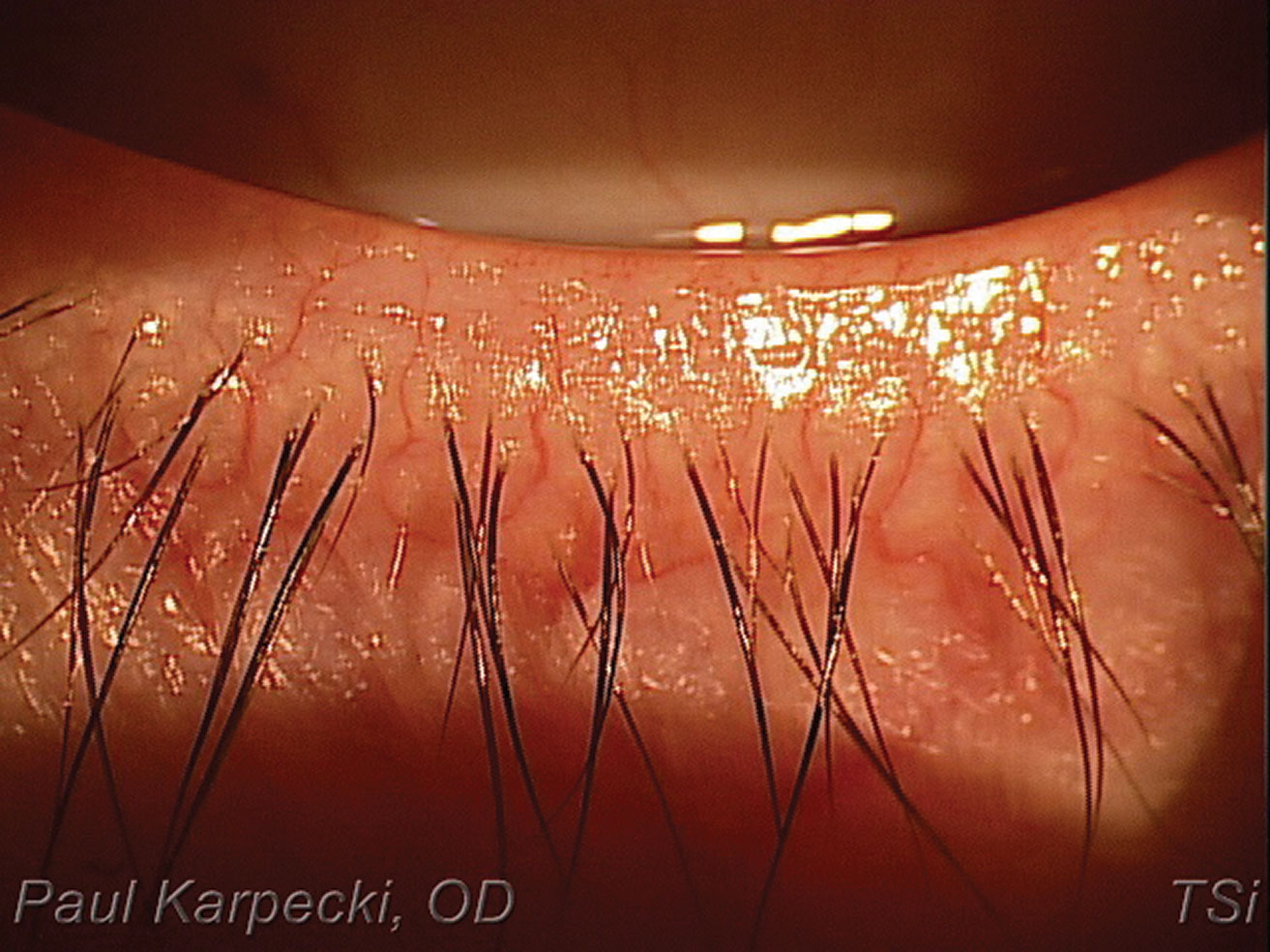 |
| Patients with hyperemia and telangiectatic vessels are ideal IPL candidates. Click image to enlarge. |
What We Know about IPL
The value of IPL in dry eye was first identified in 2002, when patients treated for skin problems reported improvement in their dry eye symptoms as well.1 The finding was good news, as more than 80% of rosacea patients have concomitant MGD.2
IPL treatments are performed with 500nm to 1,200nm light pulses for 20 to 30 minutes and can be repeated every three to five weeks. IPL can achieve clinical improvement via several potential mechanisms:3
- Thrombosis of abnormal blood vessels below the skin surrounding the eyes.
- Heating the meibomian glands and liquefying the meibum.
- Activation of fibroblasts and enhancing the synthesis of new collagen fibers.
- Eradication of Demodex and decreasing the bacterial load on the eyelids.
- Interference with the inflammatory cycle by regulation of anti-inflammatory agents and matrix metalloproteinases.
- Reducing the turnover of skin epithelial cells and decreasing the risk of physical obstruction of the meibomian glands.
- Changes in the levels of reactive oxidative species.
IPL therapy is generally considered safe; however, traditional treatment should not be considered in patients with darker skin tones (Fitzpatrick skin types of 5 or 6) due to the risk of melanin damage and resultant hypopigmentation.4
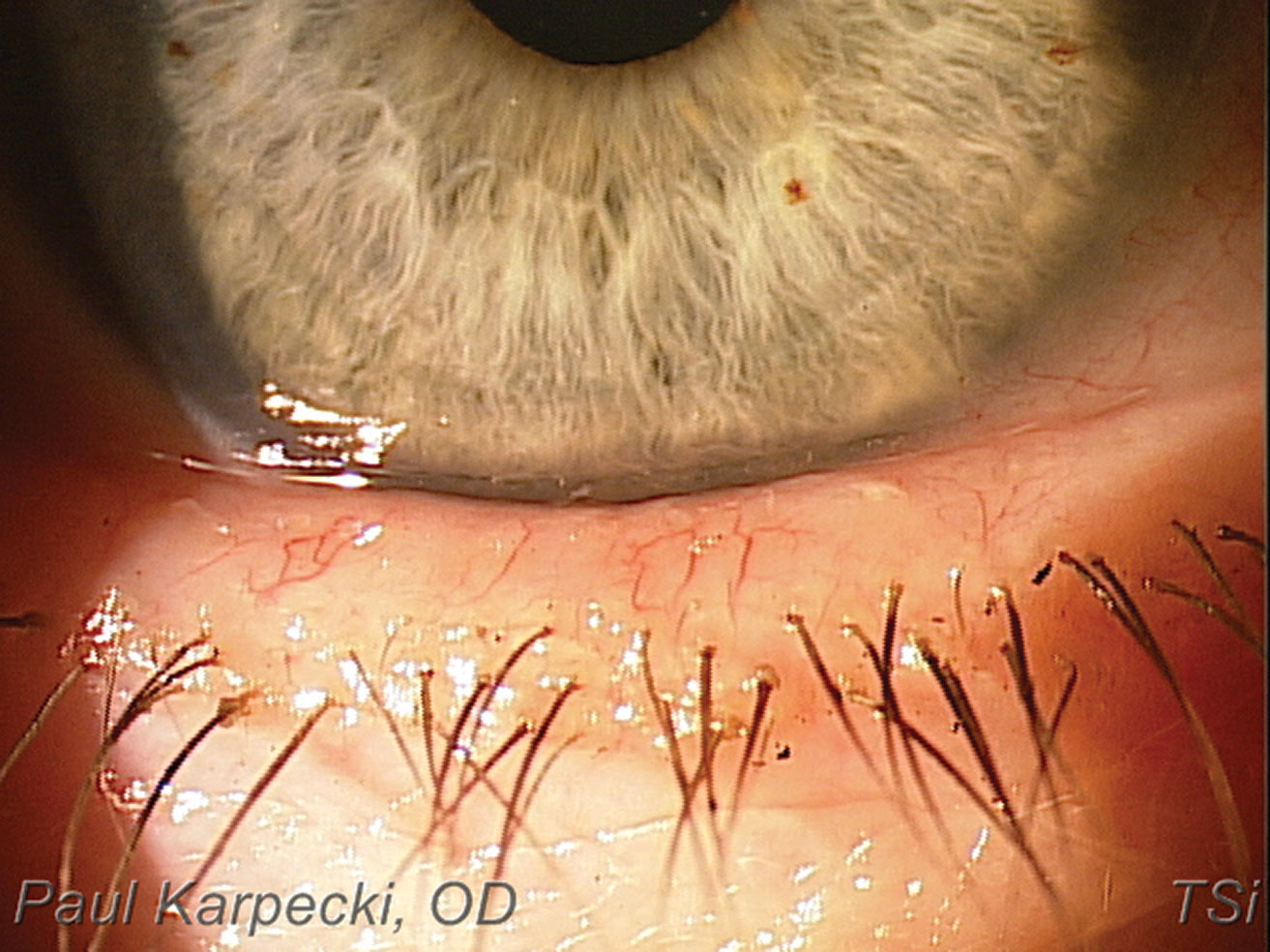 |
| Telangiectasia & blepharitis in a patient with rosacea. Click image to enlarge. |
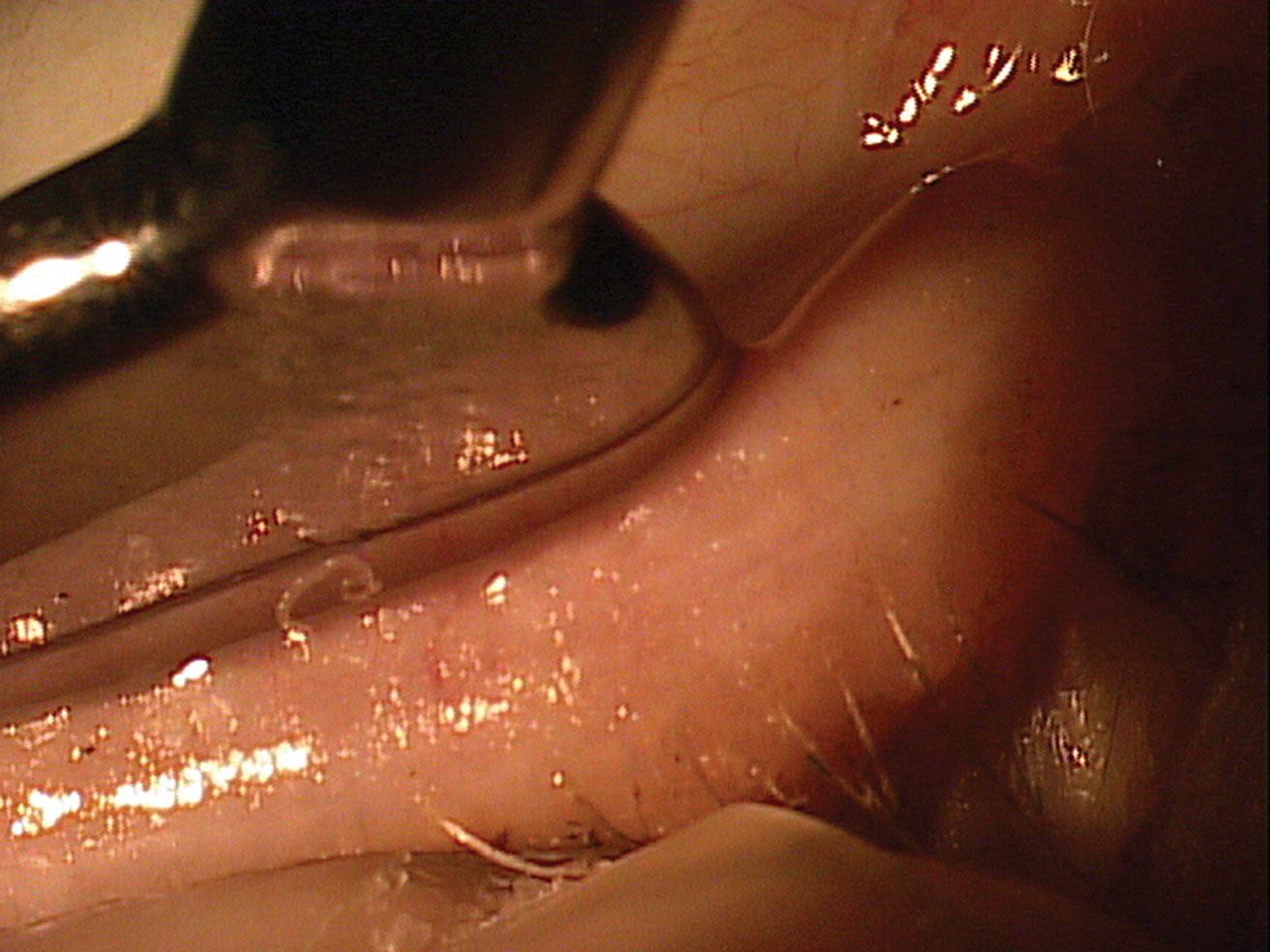 |
| Paste-like meibomian expression in a patient with MGD. Click image to enlarge. |
Two Therapies in One
Combined light therapy involves the application of both IPL and LLLT.5 LLLT is a different kind of photobiomodulation that also had its beginnings in dermatology and is now demonstrating efficacy in MGD, specifically in terms of improved tear break-up time.5,6
While IPL treatment offers thermal-based effects, LLLT is athermal, and researchers believe it has additive effects on the lids and periorbital area.5 The presumed mechanism is photoactivation.5,7 The ability to apply LLLT to the upper lid, where it is generally considered unsafe to apply IPL, may further contribute to its MGD therapy success.5
A recent study of 460 eyes evaluated the effects of combined light therapy on patients who were unresponsive to previous medical management.5 The combined treatment consisted of intense short pulses of light on the area of the face around the eye followed by longer exposure to low-level red light on the cheek and over the closed lids.5
The researchers found that mean Ocular Surface Disease Index (OSDI) scores were significantly lower after combined treatment.5 Pre-treatment, 70.4% of patients had OSDI scores indicative of dry eye; after, only 29.1% did.5 The researchers also observed a one-step or greater reduction in MGD grading in 70% of eyes, with 28% of eyes having a two-step or greater reduction.5 Tear break-up time was ≤6 seconds in 86.7% of eyes pre-treatment, which dropped to 33.9% of eyes after treatment.5 There were no ocular or facial adverse events or side effects related to treatment.5
IPL Procedure BasicsAlthough there is some variation in protocol, a standard IPL procedure begins by placing protective IPL shields over the eyes. All IPL devices, with the exception of the Eye-Light, require applying ultrasound gel to the skin to keep the treatment area cool.4 Clinicians should only treat the skin inferior and lateral to the lower eyelid margin, as there is risk of light penetration through the eyelid and absorption within the intraocular structures with upper eyelid treatment.4 For systems that require coupling gel, clinicians should remove the ultrasound gel after two passes on each side and apply a hot compress along the eyelids for two to three minutes.4 Research also shows expressing the meibomian glands following IPL treatment can be beneficial.8,9 In fact, meibum expressibility improvement might be a good therapeutic target of IPL treatment in patients with MGD and dry eye and could be an indicator of ocular surface inflammation during IPL treatment.10 In a recent study of 30 patients who underwent three IPL sessions, patients with low meibum expressibility and tear film instability experienced greater improvement in symptoms after IPL treatment.10 The improvement in meibum expressibility was also associated with a decrease in tear inflammatory cytokine levels.10 Finally, a topical steroid may be prescribed for two to three days following the procedure.4 |
Beyond efficacy and safety, practical benefits may also inspire use of combined light therapy. Specifically, the therapy adjusts energy levels for optimum effects based on the patient’s level of MGD and their Fitzpatrick skin scale score.5
Furthermore, the currently available device used for this combination therapy, Eye-Light (Topcon), requires no gel thanks to a built-in cooling system of forced air that maintains the temperature of the crystal at a non-traumatic level for the patient’s skin type.5 This may allow treatment of any patient, regardless of their Fitzpatrick skin type.
Time will tell how treatment will change with the approval of this new form of light therapy, but one thing is certain: With so many tools at our disposal, we are well equipped to treat both the signs and symptoms of dry eye and MGD with greater ease and efficacy than ever before.
Note: Dr. Karpecki consults for companies with products and services relevant to this topic.
1. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg. 2015;33(1):41-46. 2. Viso E, Rodríguez-Ares MD, Oubiña B, Gude F. Prevalence of asymptomatic and symptomatic meibomian gland dysfunction in the general population of Spain. Invest Ophthalmol Vis Sci. 2012;53(6):2601-06. 3. Dell SJ. Intense pulsed light for evaporative dry eye disease. Clin Ophthalmol. 2017 June;11:1167-73. 4. Vora G, Gupta P. Intense pulsed light therapy for the treatment of evaporative dry eye disease. Curr Opin Ophthalmol. 2015;26(4):314–18. 5. Stonecipher K, Abell TG, Chotiner B, et al. Combined low level light therapy and intense pulsed light therapy for the treatment of meibomian gland dysfunction. Clin Ophthalmol. 2019 June;13:993-99. 6. Toyos R, Briscoe D, Toyos M. The effects of red light technology on dry eye disease due to meibomian gland dysfunction. JOJ Ophthalmol. 2017;3(5):555624. 7. Kim WS, Calderhead RG. Is light-emitting diode phototherapy (LED-LLLT) really effective?. Laser Ther. 2011;20(3):205-15. 8. Arita R, Mizoguchi T, Fukuoka S, et al. Multicenter study of intense pulsed light therapy for patients with refractory meibomian gland dysfunction. Cornea. 2018;37(12):1566-71. 9. Vegunta S, Patel D, Shen J. Combination therapy of intense pulsed light therapy and meibomian gland expression (IPL/MGX) can improve dry eye symptoms and meibomian gland function in patients with refractory dry eye: a retrospective analysis. Cornea. 2016;35(3):318–22. 10. Choi M, Han SJ, Ji YW, et al. Meibum expressibility improvement as a therapeutic target of intense pulsed light treatment in meibomian gland dysfunction and its association with tear inflammatory cytokines. Sci Rep. 2019;9(1):7648. |

