 |
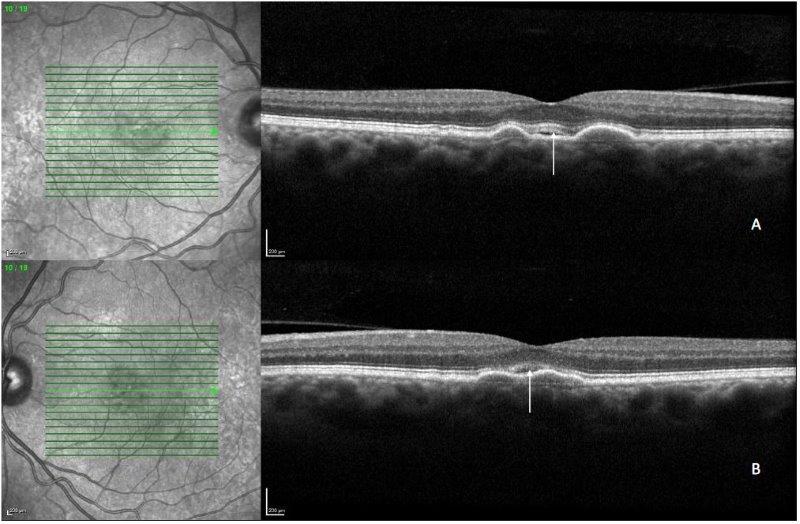
| A definitive diagnosis of this new AMD variant is key. Experts recommend a complete evaluation with multimodal imaging to rule out other causes. Differentials include conventional types of MNV, retinal vascular abnormalities such as diabetic macular edema and retinal occlusive vascular diseases, and other conditions such as intraretinal degenerative pseudocysts, ePVAC and MacTel 2. Photo: Jessica Haynes, OD. Click image to enlarge. |
In patients with age-related macular degeneration (AMD), macular neovascular (MNV) lesions are usually responsible for the presence of intraretinal fluid (IRF), but in some reports this fluid occurs in the absence of MNV lesions. To describe this new AMD variant, researchers conducted a retrospective study of patients with IRF and intermediate AMD. Their results, published in Retina, show that non-exudative IRF is a novel and distinct finding in intermediate AMD.
The study included 10 eyes of 10 patients (aged 68 to 60; mean BCVA 20/40) who demonstrated IRF in intermediate AMD. No macular neovascularization was seen on multimodal imaging, and optical coherence tomography-angiography didn’t detect any abnormal flow signal associated with IRF.
The researchers described two distinct phenotypes of patients in which IRF occurred: (1) those with serous/drusenoid pigment epithelium detachment (PED) and (2) those with an area of nascent geographic atrophy (nGA). They explained in their Retina paper that when seen on structural OCT, the “IRF associated with PED was usually found at the apex of the PED, that was surrounded by hyperreflective deposits,” while “in eyes with nGA, IRF appeared as hyporeflective cystoid spaces that follow the course of Henle’s fiber layer.”
Proposed causes and/or mechanisms for non-exudative IRF in intermediate AMD include:
- PED lesions “with considerable height,” causing mechanical stress and hydrostatic pressure;
- concomitant Muller cell loss and outer segment cell impairment, ultimately leading to cystoid IRF accumulation;
- blood retinal barrier breakdown and protein deposit accumulation between the choriocapillaris and ELM, leading to increased osmotic pressure and hyperosmolar stress;
- local hypoxia resulting from increased distance between retinal pigment epithelium (RPE) and choriocapillaris; or
- outer retinal injury leading to RPE migration to the inner retinal layers.
“These findings are of paramount relevance in the clinical setting, highlighting that we need to discern between the presence of IRF due to MNV and that due to non-MNV causes,” the researchers emphasized in their paper. They concluded that larger cohorts are needed along with multimodal approaches to “improve the understanding of the mechanism at play causing the IRF” in intermediate AMD and to improvement the management of patients in this subgroup.
Servillo A, Kesim C, Sacconi R, et al. Non-exudative intraretinal fluid in intermediate age-related macular degeneration. Retina 2024. [Epub ahead of print]. |

