 |
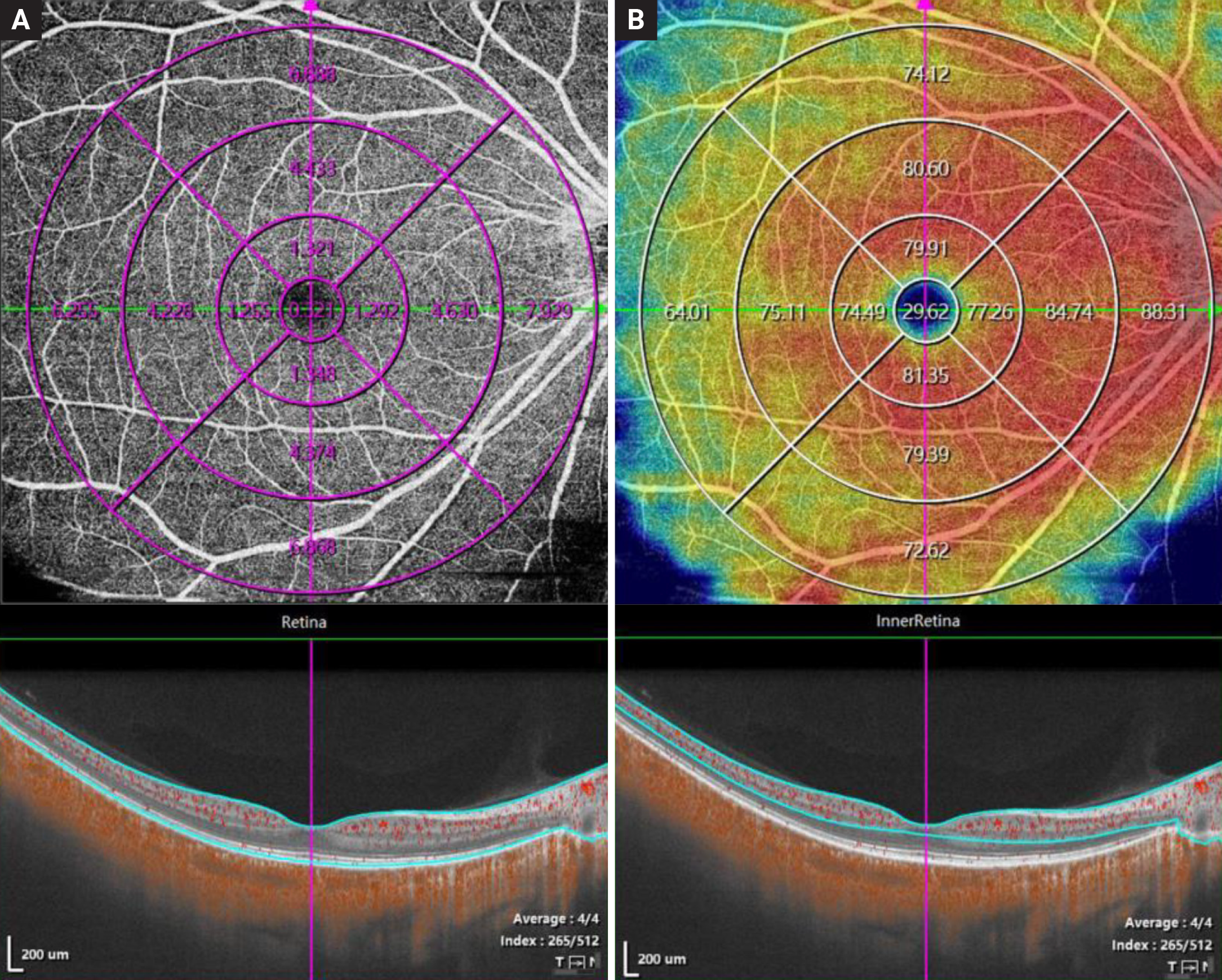
| This study was able to correlate changes in flow area (A) and vessel density (B) on OCT-A with fundus changes on ultra-widefield imaging in myopes with varying disease severities. Photo: Xu Y et al. Ophthalmic Res. Sept. 28, 2023. Click image to enlarge. |
When monitoring patients with myopia, especially those with higher refractive error, clinicians must always be on the lookout for signs of potential complications, which often manifest as vascular or fundus changes. With the advent of OCT angiography (OCT-A), optometrists with access to this device are now able to visualize the microvasculature of myopic patients without using intravascular dye. Ultra-widefield (UWF) imaging also has an evolving role in myopia management by simplifying the examination of the far periphery of the retina.
Researchers recently used these two devices in tandem to help paint a clearer picture of the role of microvasculature in myopic retinopathy pathogenesis. In their cross-sectional study, they found several associations between the vascular features of myopia on OCT-A and the fundus manifestations observed using UWF imaging.
The study enrolled 74 patients with myopia (30 with low to moderate disease and 44 with high myopia). All patients underwent ophthalmic examinations and imaging of the right eye using OCT-A and UWF fundus cameras. On OCT-A, the parameters of flow area, structure thickness and vessel density were obtained. On UWF imaging, the researchers measured tessellation and parapapillary atrophy.
The researchers observed a larger flow area in the outer retina and a thinner choroid in patients with high myopia. They elaborated in their paper on the study, published recently in Ophthalmic Research, “Thinning of the choroid is a striking feature in myopia, and a negative correlation has been reported between choroidal thickness and axial length. Choroidal thickness appeared to be the most important index among all OCT-A parameters, exhibiting apparent differences between the high myopia and low/moderate groups and revealing a stable correlation with axial length in all measured zones,” they wrote. The rate of choroidal thickness was also inversely related to axial growth speed, which the researchers suggest implies that “choroidal thickness has abundant clinical significances to explore and could serve as an ideal predictor of ocular elongation and myopia progression.”
A significant correlation was also found between axial length and retinal and choroidal flow area and thickness in the different zones. Additionally, a positive correlation was demonstrated between parapapillary atrophy area and flow area in the outer retina, while the former parameter was negatively correlated with choroidal thickness.
Another observation the team made was that “In the inner vascular retina, the vessel densities and flow area were reduced in eyes with higher grades of tessellation, as vessel density of inner retina, deep and superficial vascular complexes, as well as flow area of angio retina and inner retina all revealed a negative correlation with tessellation in two or more zones.”
The researchers conclude that the data from their combined analysis on OCT-A and UWF illustrated “the existence of higher flow area in the outer retina and smaller choroidal thickness in patients with high myopia, the negative correlation between choroidal vasculature and axial length and the connection between OCT-A parameters and common myopic fundus manifestations. Our findings may aid in understanding myopic retinopathy and its related vascular and structural fundal changes.”
Xu Y, Yang W, Niu L, Wang X, Zhou X, Li M. Myopic vascular changes revealed by optical tomography angiography and their association with myopic fundus manifestations. Ophthalmic Res. September 28, 2023. [Epub ahead of print]. |

