 |
|
Topical steroids increased IOP in DME patients after eight and 12 weeks of treatment, while those treated with an NSAID demonstrated stable levels. Photo: Anna Bedwell, OD. Click image to enlarge. |
While anti-VEGF injections are an effective treatment for many patients with diabetic macular edema (DME), this method of drug delivery has several drawbacks. The treatment is invasive, requires multiple injections, can increase intraocular pressure (IOP) and is less effective in patients with mild disease.
Topical therapy is an alternative noninvasive treatment for DME that has become a more desirable option for patients in recent years, though the efficacy of these ophthalmic solutions is still under investigation. A new study compared the performance of the NSAID bromfenac with that of an ophthalmic steroid, betamethasone. The data showed that DME patients treated with the NSAID experienced no increase in IOP over 12 weeks, while those who received the topical steroid showed a significant increase at eight and 12 weeks of treatment.
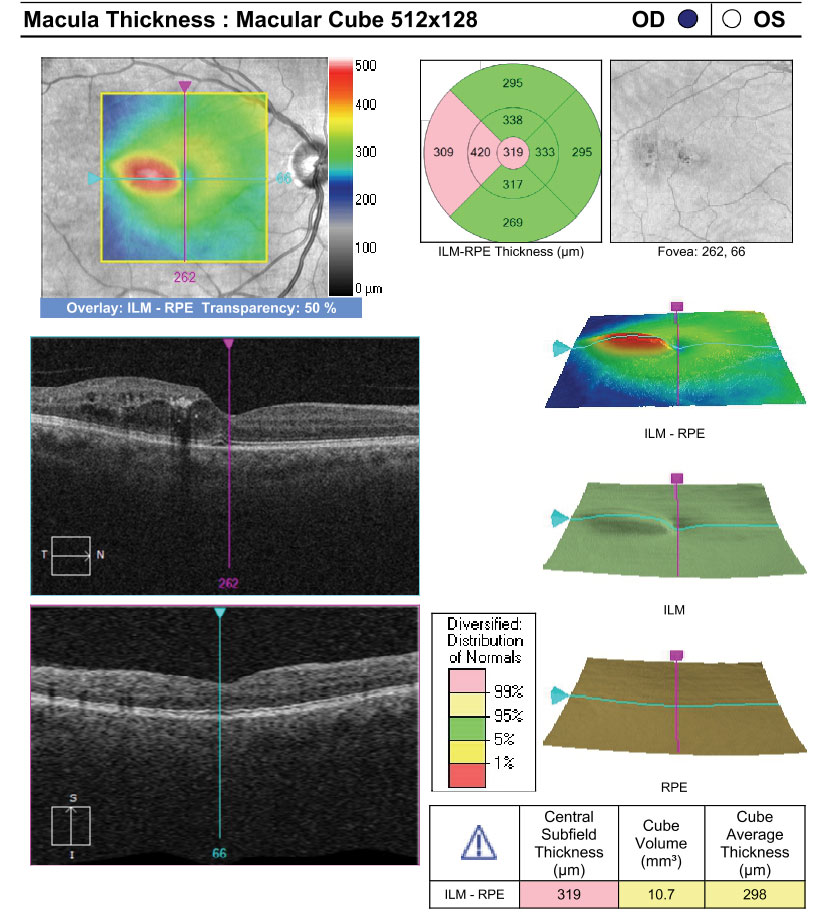
The small prospective trial involved 19 patients (mean age: 67) with DME, an HbA1c level below 10%, a mean retinal thickness within a 1mm diameter from the fovea and a central subfield thickness (CST) of 250mm to 500mm. Ten patients were randomly chosen to receive the NSAID, while nine received the steroid. The drops were instilled two times a day in the NSAID group and four times a day in the steroid group. The clinicians measured the following at four, eight and 12 weeks of treatment: CST, BCVA and IOP.
CST and BCVA in patients treated with either the NSAID or the steroid did not differ significantly at any point between baseline and the end of the study period. The researchers did find that in patients with an HbA1c of 6.7% treated with the NSAID, the average CST improved from 309µm to 289µm.
The two groups had similar baseline IOPs. In the steroid group, the mean IOP increased by nearly 2mm Hg at eight weeks and 3mm Hg at 12 weeks.
Along with the benefit of a more stable IOP, the study authors also pointed out the advantage of twice-daily instillation required by NSAID therapy. “It is believed that, compared with bromfenac, which requires instillation four times daily, it is easier to continue the administration of betamethasone due to safety and patient adherence to long-term instillation,” they wrote.
The study reported three total adverse events, including subretinal fluid (NSAID group), vitreous hemorrhage (NSAID group) and elevated IOP (steroid group). However, the authors wrote, “All were non-serious events and disappeared/recovered or improved after discontinuation of drug administration.”
The data from this trial shows that, compared with topical steroids, treatment with ophthalmic NSAIDs may offer more stable IOP levels and potentially reduce CST in DME patients with good glycemic control.
Tobimatsu Y, Ogihara R, Endo N, et al. Comparison of the effect of bromfenac versus betamethasone ophthalmic solutions in patients with diabetic macular edema. Current Eye Research. November 4, 2022. [Epub ahead of print]. |

