 |
Q:
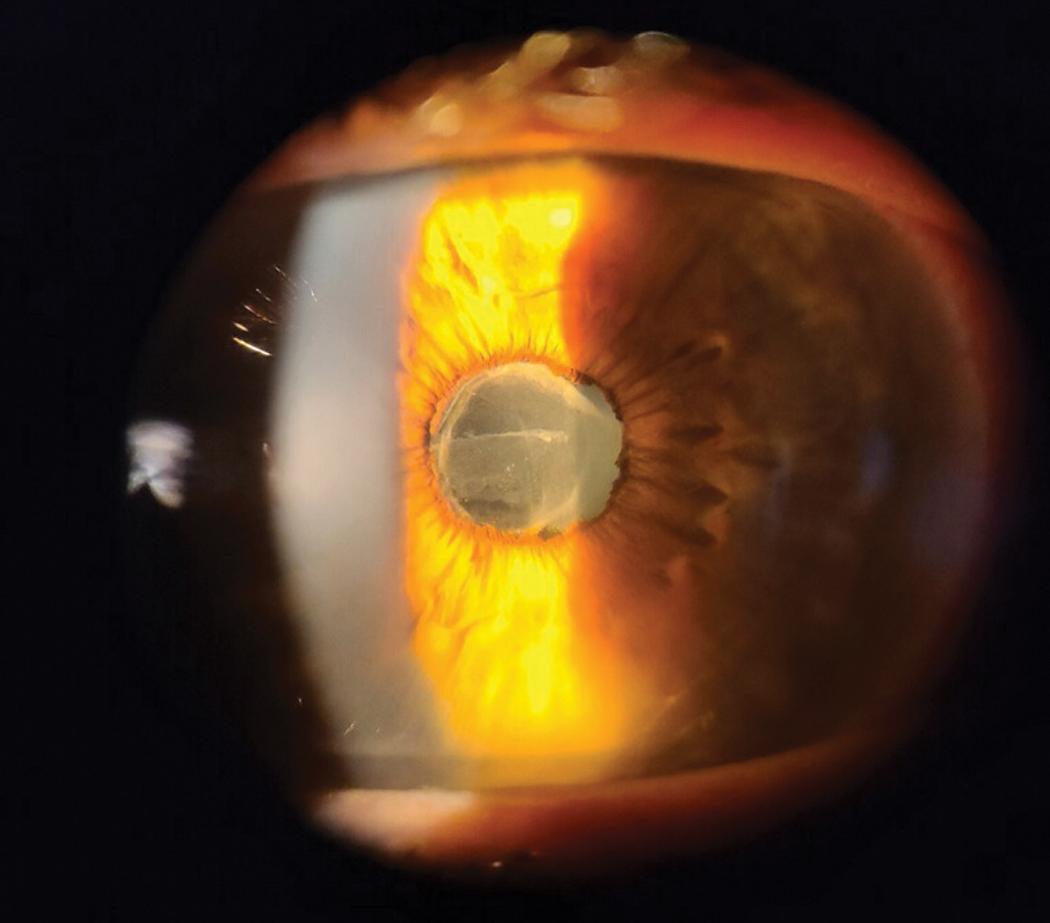
A 34-year-old Hispanic male presented with a two-week history of a painful, red left eye. Exam reveals 2+ cells and flare, mild posterior synechia and an early cyclitic membrane. He’s been using a topical antibiotic without improvement in symptoms. What’s the diagnosis, initial treatment and potential work-up indicated if the condition recurs?
A:
“The presence of anterior chamber cells and flare, combined with the posterior synechiae, indicates iris involvement (iritis), while the cyclitic membrane suggests ciliary body involvement as well (cyclitis),” says Chris Wroten, OD, of Bond-Wroten Eye Clinic in Louisiana. “Thus, we would classify this as an iridocyclitis and treat it more aggressively than we would with a run-of-the-mill iritis.”
“Don’t forget to rule out infectious and traumatic etiologies, including chlamydia and thyroid eye disease, as potential causes of recalcitrant, monocular conjunctivitis,” Dr. Wroten notes. This patient reported good systemic health while denying contact lens wear, previous eye surgery, known trauma or potential foreign bodies.
 |
|
Only when the cells and flare from uveitis resolve dramatically should ODs begin a slow taper of the steroid to prevent rebound. Click image to enlarge. |
Treatment
Dr. Wroten recommends prescribing Durezol (difluprednate 0.05%, Novartis) every one to two hours while awake, with atropine 1% twice daily and 10% phenylephrine in-office to break the synechia. Because pharmacies don’t stock these meds, have some on hand and send them home with them, to be used QID if the patient has no contraindications.
“Steroids need a couple of days to control inflammation, so don’t be tempted to believe treatment isn’t working,” he advises. Control any nasolacrimal drainage issues and prolong ocular contact at the same time by inserting collagen plugs in the affected eye(s). Add other medications such as topical or oral non-steroidal anti-inflammatories if the inflammation does not resolve quickly enough.
For complex noninfectious cases, consider either oral prednisone or sustained-release steroid implants, such as Dextenza (0.4mg dexamethasone ophthalmic insert, Ocular Therapeutics) and Ozurdex (dexamethasone intravitreal implant; Allergan).
One can consider subconjunctival, sub-Tenon’s or intravitreal steroid injections, but recognize that most chronic steroid therapies may cause elevated intraocular pressure, posterior subcapsular cataracts, opportunistic infections and delayed healing post-op.1,2
Lab Work and Follow-up
If the uveitis is bilateral, chronic, recurrent or recalcitrant, or additional clinical signs emerge, Dr. Wroten suggests starting with a complete blood count with differential to rule out infectious etiologies, in addition to tests for general systemic inflammation as well as other targeted labs based on the patient’s age and clinical history.
Uveitis occasionally precedes positive lab tests by months to even years. “If suspicion of systemic etiology persists, repeat labs at appropriate intervals even if a previous work-up was negative,” Dr. Wroten says.
If signs and symptoms are improving satisfactorily and the synechia are broken at the one-week follow-up, keep the patient on the aggressive steroid plan and gradually taper the dilating agents. Only when the cells and flare resolve dramatically should you begin a slow taper of the steroid over a number of weeks. Tapering too quickly will result in rebound, and the drops will need to be increased again for a longer period of time.
In cases where steroids are contraindicated or ineffective, consider systemic immunosuppressant medications such as methotrexate, mycophenolate mofetil and azathioprine.3
“Our goal is to restore a white, quiet eye with good vision and without long-term inflammatory sequela, so appropriate but aggressive therapy early on is my preference,” Dr. Wroten says. “If the condition is unresponsive to common therapies, consider a consult to a uveitis or retinal specialist for consideration of other therapies.”
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International. He has no financial interests to disclose.
1. Food and Drug Administration. Dextenza (dexamethasone ophthalmic insert) 0.4 mg,for intracanalicular use. www.accessdata.fda.gov/drugsatfda_docs/label/2019/208742s001lbl.pdf. Accessed August 17, 2021. 2. Food and Drug Administration. Ozurdex (dexamethasone intravitreal implant). www.accessdata.fda.gov/drugsatfda_docs/label/2014/022315s009lbl.pdf. Accessed August 17, 2021. 3. Bethke, W. The latest treatment approaches for uveitis: don’t hesitate to use immune-suppressing medications in severe patients, surgeons say. Rev Ophthalmol. 2017;24(8):35-9. |

