 |
Q:
A 29-year-old male with a history of systemic lupus erythematosus (SLE) presented with a red eye with mild tenderness and light sensitivity for six days. His doctor put him on a generic topical steroid Q3H for three days without improvement. What are the next steps?
A:
"Whenever there is localized (sectoral) injection, we should consider superficial causes such as conjunctival abrasion, Staph. marginal keratitis or infiltrates and episcleritis,” says Anthony DeWilde, OD, of the Kansas City VA Medical Center in Missouri. "Phenylephrine 2.5% can aid in the diagnosis, and in this case, lessened the injection somewhat but not completely.”
Distinguish Simple from Severe
Episcleritis commonly appears as sectoral injection involving both the episcleral tissues and overlying conjunctiva, usually concentrated in either the nasal or temporal quadrant.
Most cases are unilateral, but they may occur bilaterally in cases of toxic exposure or underlying systemic disease. There may be symptoms of pain or burning, but patients are always alarmed by the redness. Most cases of episcleritis are self-limiting, resolving spontaneously within two to three weeks even without treatment.
Take care to distinguish episcleritis from the more severe scleritis, which may appear similar. Ocular injection is typically deeper with scleritis, and the eye will not blanch with 2.5% phenylephrine as it would in episcleritis.
Scleritis can be anterior or posterior based on its relative location to the recti muscle insertion. Anterior scleritis, the most common form, can be subdivided into diffuse, nodular or necrotizing forms, with diffuse being the most common and causing widespread inflammation,” says Dr. DeWilde.
Nodular scleritis tends to have more localized injection with a raised nodule. Necrotizing scleritis is associated with collagen vascular disorders and causes destruction of the sclera. Posterior scleritis occurs far more often than previously thought and can lead to rapid and permanent visual loss.! Fundus examination is critical and may reveal optic nerve edema, exudative retinal detachment or choroidal effusions.
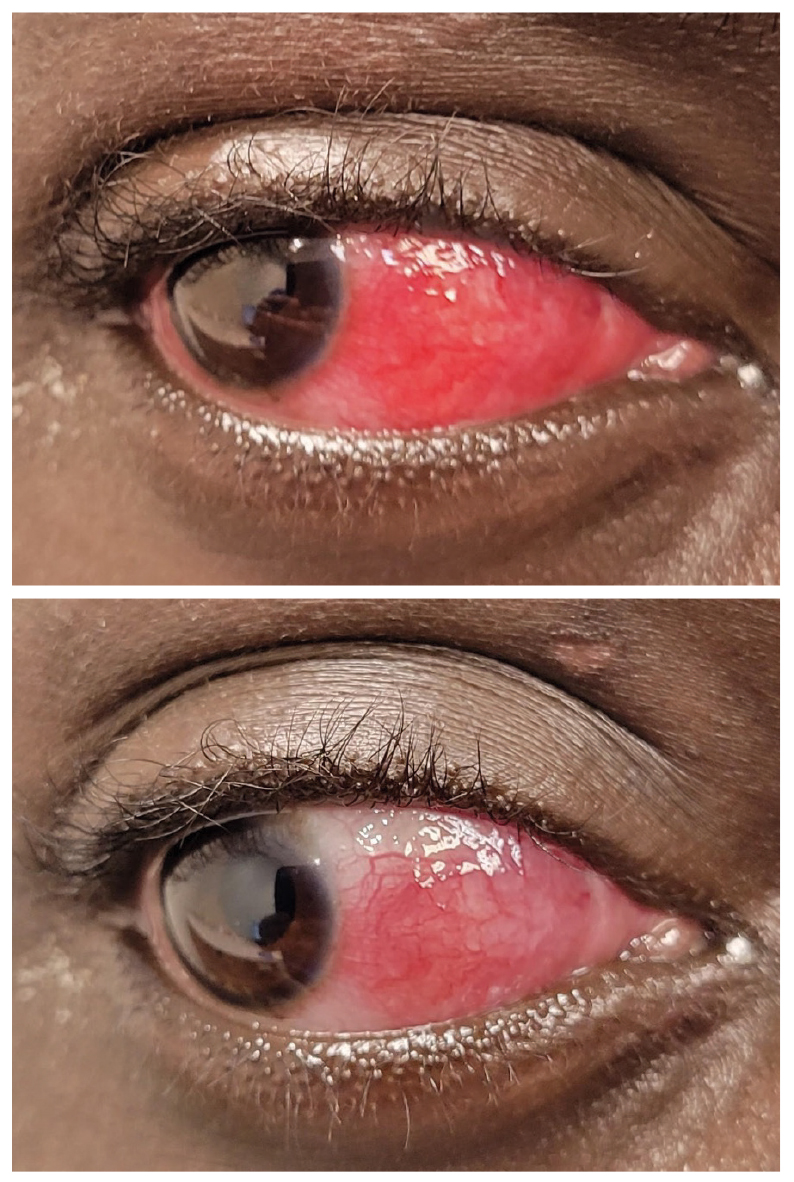 |
| Most cases of scleritis will only blanch partially with topical 2.5% phenylephrine. Click image to enlarge. |
Treatment and Follow-up
In this patient, there was no improvement with three days of topical treatment. “While Durezol (difluprednate 0.05%, Novartis) could be more effective than Pred Forte (prednisolone acetate 0.1%, Allergan), our patient was suspected to have scleritis, which requires oral NSAIDs and/or oral corticosteroids (1mg/kg),” Dr. DeWilde says.
In this case, NSAIDs were not used due to a contraindication with the patient’s chronic stage 1 kidney disease. He was treated with oral methylprednisolone 30mg PO daily. He was advised to continue the Cellcept (mycophenolate mofetil, Genentech) and Plaquenil (hydroxychloroquine, Sanofi) that he still takes for SLE. The patient’s symptoms were resolved after four days of oral corticosteroids, with a significant improvement in redness.
Due to the pre-existing autoimmune disease, the decision was made to not pursue more laboratory tests. If patients are diagnosed with scleritis, there is about a 50% chance they have an associated autoimmune condition. “Most commonly these are rheumatoid arthritis, SLE and polyarteritis nodosa,” Dr. DeWilde says. “To evaluate for associated conditions in scleritis, a referral to rheumatology would be warranted.”
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International and is vice president of the Georgia State Board of Optometry. He has no financial interests to disclose.
1. McCluskey PJ, Watson PG, Lightman S, et al. Posterior scleritis: clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology. 1999;106(12):2380-6. |

