 |
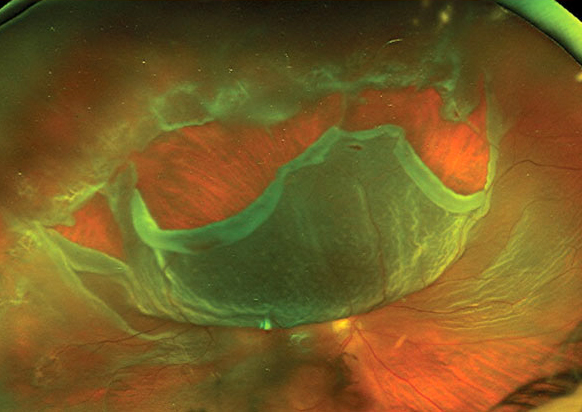
Quite a few demographic disparities in ED visits for retinal detachment were found in this recent study, including issues with access to care and cost of procedures and services. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
There are inequities in access and outcomes throughout healthcare, especially in cases when patients have to go to the emergency department (ED), but the epidemiologic and economic burden of visits involving sight-threatening diseases such as rhegmatogenous retinal detachment (RRD) haven’t been reported. In this study, researchers analyzed the demographic and hospital billing amount and cost of service disparities in RRD visits to EDs nationwide and found several, including Whites having a higher likelihood for same-day treatment compared with other racial groups and the cost of service higher in self-paying patients compared to those with insurance.
A retrospective, cross-sectional, population-based study using CPT codes in the 2016 to 2019 Nationwide Emergency Department Sample databases to identify RRD visits was conducted. The analysis included demographics, hospital billing amount and cost of service of RRD ED management.
A total of 12,492 RRD encounters were identified with the prominent age group being 50 to 64 years (49.3%). Most patients (90%) were managed in metropolitan teaching hospitals, mostly in the southern U.S. region. Private insurance covered 45% of patients.
Hispanics had the highest RRD ED incidence and Native Americans had the lowest. Similar to previous studies, African Americans and Asians had lower incidences of RRD ED visits than Whites. While no sex bias was found, Whites are more likely to receive same-day ED repair compared with these racial groups. Several factors could contribute to this, the authors noted, including better access to care, socioeconomic differences and differences in health-seeking behavior.
“It is important to further investigate these potential factors to address disparities in RRD treatment and ensure equitable care for all patients, regardless of their race,” the authors explained in their paper for the Retina journal. “This finding should be interpreted with caution because it could be influenced by factors such as the availability of ophthalmology staffing and surgical capabilities at the EDs visited by patients of different races.”
It should be noted that patients with RRD who went to the ED during November and December were more likely to have RRD repair during the same visits.
“We postulate that limited patient access to subspecialty surgeons during the holiday seasons may explain the need for same visit ED-based surgical interventions,” the authors wrote. “One study using a claims-based cohort of primary RRD surgery in the United States demonstrated that management of RRD varied according to the day or the week; pneumatic retinopexy was disproportionally likely to be selected over the weekends, when there is less operating room availability.”
ED mean billing amount and cost of service were higher in self-paying patients compared with those with any form of insurance, highlighting health disparities directly in RRD repair, the authors suggested. The cost of service varied by the procedure performed was around $610 to $4,501, with a mean of $3,372. The overall inflation-adjusted hospital billing amount associated with RRD visits rose over the study period, although the cost of service did not change.
“Although the procedure type could account for a difference in the total billing amount and cost of service across the years, our data did not show a difference in the increased rate across the procedure types based on CPT codes,” the authors concluded. “Although the present data on cost of service reflect the economic impact of repairing an RRD, they underrepresent the cost of service associated with RRD because they do not include indirect expenses such as lost work time and transportation, visual aids required for daily activities and comorbidities in patients with impaired vision.”
Shaheen AR, Ashkenazy N, Iyer PG, et al. Nationwide demographic disparities in United States emergency department visits in patients with rhegmatogenous retinal detachment. Retina. 2023;43:1936-44. |

