 |
A 22-year-old Caucasian female was referred for ophthalmic evaluation following discharge from a hospital where she was admitted for workup due to four days of a right-sided headache, horizontal double vision, ringing in her ears and transient visual obscurations. She was taking an oral contraceptive and was allergic to heparin. Prior to this episode, her past medical, ocular and family histories were all unremarkable.
Visual acuity was 20/25 OD and 20/30 OS. There was -1 abduction OD and -4 abduction OS. Confrontation visual field testing was full to finger counting OU, pupils were equal in size and reactivity without relative APD. IOP was 12mm Hg OD and 15mm Hg OS, and Ishihara color plates were full OU.
Take the Retina Quiz
1. According to the Frisén classification of optic nerve edema, how would you grade the optic nerves seen in Figures 1 and 2?
a. Grade 2.
b. Grade 3.
c. Grade 4.
d. Grade 5.
2. Which of the following is NOT a risk factor for bilateral optic nerve edema?
a. Blood dyscrasias.
b. Brain tumor.
c. Systemic hypertension.
d. Overhydration.
3. Which of the following is NOT indicated in the workup for this patient?
a. Measuring blood pressure.
b. MRI of the brain and orbits with and without contrast.
c. MRV of the brain without contrast.
d. All of the above are indicated.
4. According to the Idiopathic Intracranial Hypertension Treatment Trial, what is the maximum recommended dose of oral acetazolamide that is considered safe?
a. 250mg PO BID.
b. 500mg PO BID.
c. 1,000mg PO BID.
d. 2,000mg PO BID.
5. Which of the following is required to make a diagnosis of idiopathic intracranial hypertension (IIH)?
a. Absence of spontaneous venous pulsation.
b. Negative MRI brain and orbits, and MRV brain.
c. Lumbar puncture opening pressure <20cm H2O.
d. Transverse sinus thrombosis.
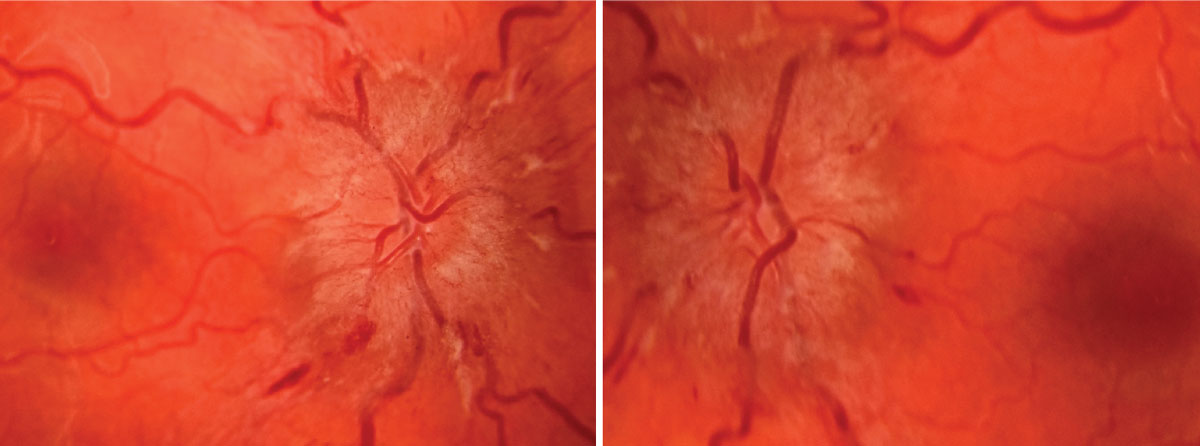 |
Topcon fundus photo of optic nerve OD at presentation (left). Topcon fundus photo of optic nerve OS at presentation (right). Click image to enlarge. |
Diagnosis
While in the hospital, the patient underwent neuroimaging that identified cerebral venous thromboses (CVT) present on magnetic resonance venogram (MRV) in the upper right internal jugular vein, as well as the right superior sagittal, transverse and sigmoid sinuses. Serologies to investigate for blood dyscrasias uncovered a previously undiagnosed Factor V Leiden heterozygous mutation and elevated Factor VIII (antihemophilic factor A) activity of 238% (reference range 60% to 150%).
It was felt that the Factor V Leiden positivity in the setting of oral contraceptive use put her at an increased risk for developing the CVTs and secondary intracranial hypertension. She was treated acutely with tissue plasminogen activator and systemic anticoagulation, and her birth control pill was discontinued. She was discharged on warfarin 5mg PO BID and acetazolamide 250mg PO BID.
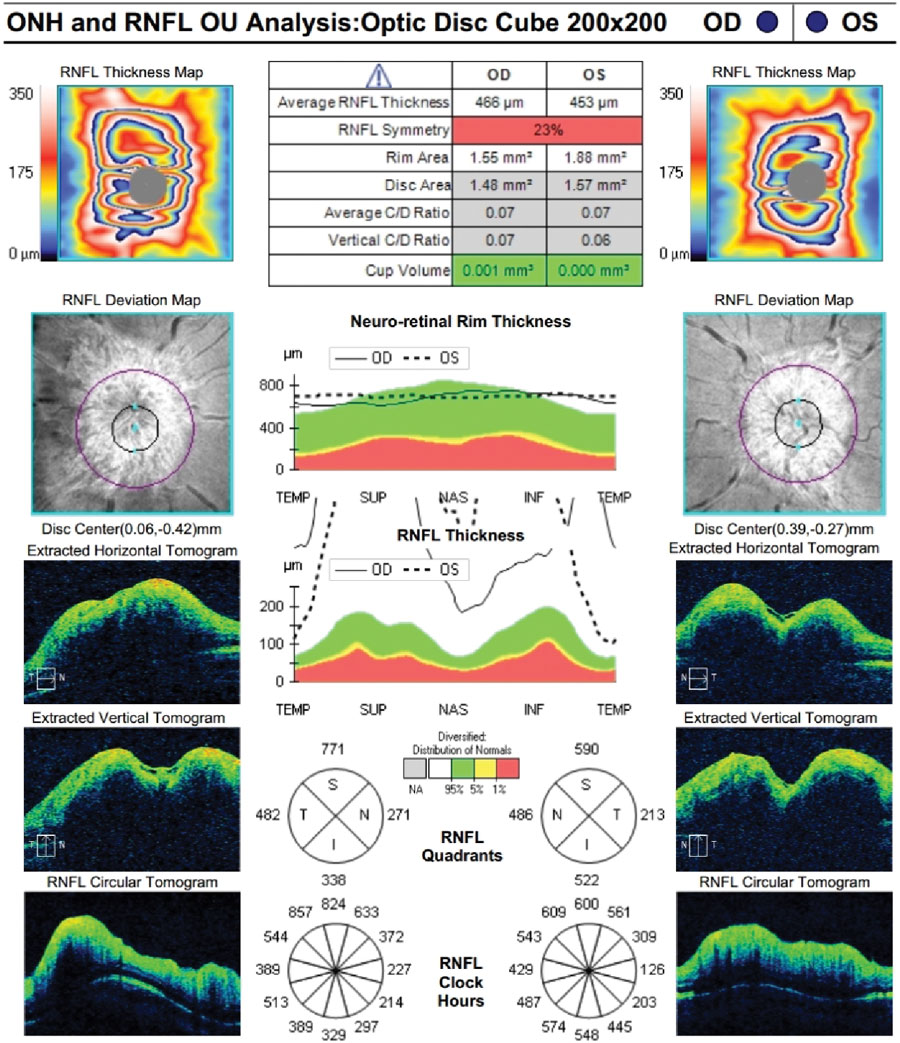
Upon presentation to our institute, she was found to have bilateral (left >> right) cranial nerve VI palsies and grade 4 optic disc edema OU. Her headache improved, but she still had pulsatile tinnitus, horizontal diplopia worse in left gaze and transient visual obscurations varying with positional changes.
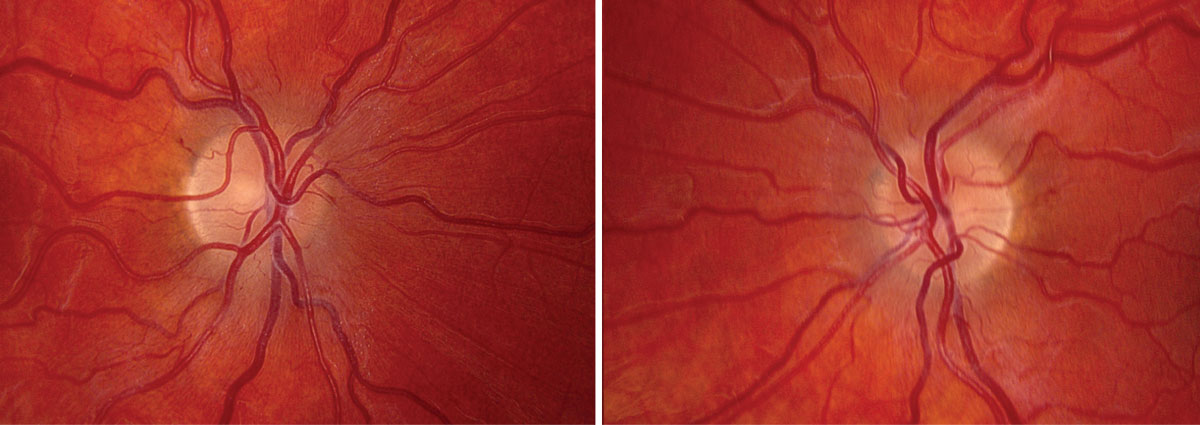 |
Topcon fundus photo of optic nerve OD at presentation (left). Topcon fundus photo of optic nerve OS at presentation (right). Click image to enlarge. |
Discussion
Papilledema is defined as optic nerve edema in the setting of intracranial hypertension (e.g., space-occupying lesion, infection, malignant hypertension, idiopathic).1,2 When there is no elevated intracranial pressure (ICP) as the underlying etiology, the term optic nerve edema is more appropriate, defined as swelling of the optic nerve head secondary to local or systemic etiologies (e.g., optic neuritis, ischemic optic neuropathy, uveitis, retinal vein occlusion, radiation, medication use).1
The pathophysiology underlying optic nerve edema is based on stasis or obstruction of axoplasmic transport and secondary accumulation of fluid within the retinal nerve fiber layer (RNFL).1 Such edema appears opaque and can blur the appearance of the optic nerve and its vasculature.1
Papilledema is graded on the Frisén scale from 0 to 5, with grade 0 being a normal optic nerve without edema.1,3 Grade 1 is defined as a “c-shaped” halo of blurring along the nasal border of the optic nerve, and grade 2 is characterized by a circumferential halo of optic nerve obscuration.1,3 Grades 3 to 5 are determined by degree of blood vessel obscuration; grades 3 and 4 are defined by partial obscuration of a major blood vessel leaving and on the disc, respectively, and grade 5 is characterized by obscuration of all vessels leaving and on the disc with obliteration of the cup.1,3
While the absence of spontaneous venous pulsations is an early and subtle indicator of elevated ICP, it may be absent in up to 10% of normal patients.4
 |
|
Zeiss Cirrus RNFL OU at presentation. Click image to enlarge. |
Workup
A thorough and careful history is required to elicit symptoms of blurry vision, pulsatile tinnitus, intermittent or constant horizontal binocular diplopia, transient visual obscurations, neck stiffness, headache, nausea and altered states of consciousness. Pertinent medication history includes hormone-containing contraception, tetracycline antibiotics, vitamin A, lithium and systemic steroid use—all of which can elevate intracranial pressure or are risk factors for venous thrombosis.1
Additional history should include smoking status, presence of metabolic syndrome (measuring blood pressure and BMI calculation) and recent weight gain.1
Idiopathic intracranial hypertension is a diagnosis of exclusion that requires a completely negative work-up to rule out primary etiologies for elevated ICP, including MRI and MRV of brain and orbits with/without contrast.1 Once space-occupying lesions have been ruled out, lumbar puncture can be diagnostic to measure the opening pressure and confirm elevated ICP; typical opening pressure in an adult is <20cm H2O.5 Positive neuroimaging findings warrant consultation with appropriate subspecialties and further investigative studies as indicated.
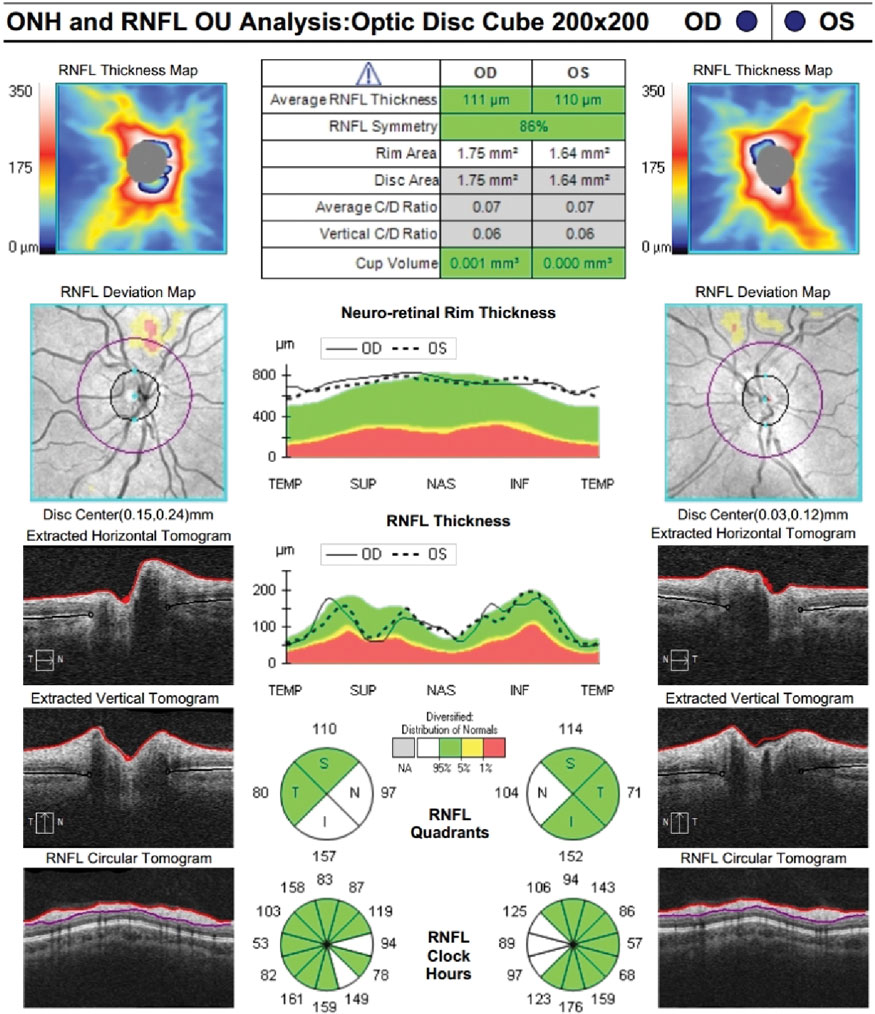 |
Zeiss Cirrus RNFL OU at follow-up. Click image to enlarge. |
Management
Primary etiologies for papilledema, when present, must be addressed directly. IIH may be treated with weight loss and oral acetazolamide.6 The Idiopathic Intracranial Hypertension Treatment Trial demonstrated safety, tolerability and efficacy of oral acetazolamide titrated to a maximum daily dose of 4g (divided into two doses).6
Our patient’s CVTs were addressed with acute and long-term systemic anticoagulation, cessation of her oral contraceptive and initiation of acetazolamide. Acetazolamide was titrated to 3g daily (1,500mg PO BID) and she achieved complete resolution of her cranial nerve VI palsies and optic nerve edema within three and nine months, respectively, with a final visual acuity of 20/20 OU. The patient was ultimately tapered off acetazolamide and maintained systemic anticoagulation with warfarin 5mg PO QD indefinitely.
CVTs are a rare but life-threatening cause of optic nerve edema. This case underscores the significance of including MRV in the work-up of all patients presenting with bilateral optic nerve edema. Furthermore, even when there are known risk factors for hypercoagulability such as oral contraceptive use, blood dyscrasias must be ruled out with thorough serological studies.
Retina Quiz Answers
1: c, 2: d, 3: d, 4: d, 5: b
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. Neither has any financial disclosures.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Yanoff M, Duker JS, Ausburger JJ, et al. Ophthalmology, 5th ed. Philadelphia: Elsevier Saunders, 2019. 2. Ryan SJ, Davis JL, Flynn HW, et al. Retina, 5th ed. London; New York: Saunders/Elsevier, 2013. 3. Frisén L. Swelling of the optic nerve head: a staging scheme. J Neurol Neurosurg Psychiatry. 1982;45(1):13-8. 4. Jacks AS, Miller NR. Spontaneous retinal venous pulsation: aetiology and significance. J Neurol Neurosurg Psychiatry. 2003;74(1):7-9. 5. Bowling B, Kanski JJ. Kanski’s clinical ophthalmology a systematic approach. [Erscheinungsort nicht ermittelbar: Elsevier, 2016. 6. Smith SV, Friedman DI. The Idiopathic Intracranial Hypertension Treatment Trial: a review of the outcomes. Headache 2017;57(8):1303-10. |

