 |
The pursuit of a more youthful appearance has led to innovative treatments that extend beyond skincare products that rarely deliver the results people seek. Surgical procedures have a role but there is downtime and risk involved. Neurotoxin injections have emerged over the last twenty years and are a powerful tool for enhancing the aesthetics of the eyes. This minimally invasive method offers a highly effective solution. If you have given a patient a new prescription for spectacles or contact lenses, you have witnessed the transformation that people experience when they enhance the way the look with a fabulous frame or when they gain spectacle freedom.
Why should we stop there? Let’s explore the transformative potential neurotoxin injections have in eye care and shed light on the mechanism, the safety and the impact on the overall appearance of the eyes.
 |
|
Injection sites for glabella into procerus and corrugators. All photos: Adobe. Click image to enlarge. |
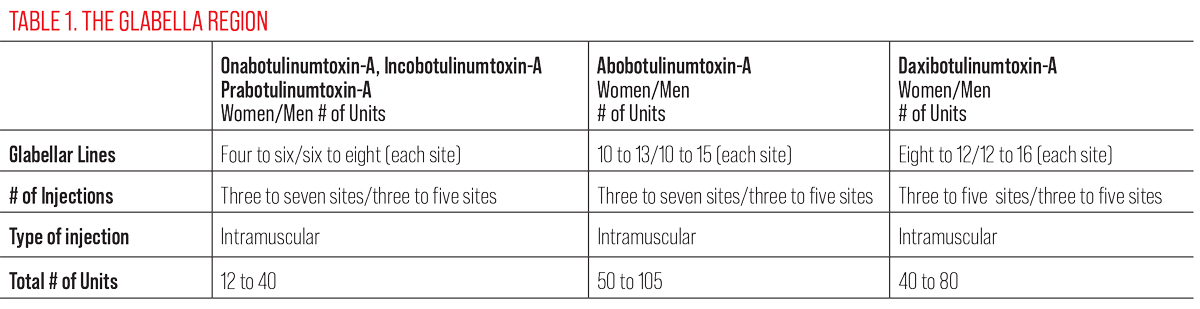 |
| Click table to enlarge. |
Background
Neurotoxin is the number one minimally invasive procedure performed in the US according to the American Society of Plastic Surgeons. These treatments involve the use of purified botulinum toxin, which is a potent neurotoxin produced by the bacterium Clostridium botulinum. These injections have gained immense popularity for their ability to reduce the appearance of wrinkles and fine lines. The intramuscular injection of botulinum toxin inhibits the release of acetylcholine from the presynaptic motor neurons which cause muscle paralysis temporarily.1
 |
|
Injecting 4.0 units of neurotoxin into the procerus muscle. Click image to enlarge. |
When properly reconstituted and effectively administered in a trained provider’s hands, the relaxation of the muscle and the diminishment of wrinkles and fine lines can give very pleasing aesthetic results.2 In our context, there are a lot of muscles that can be intentionally manipulated around the eyes. Remember, neurotoxin works well on dynamic wrinkles because it prevents the muscle from working during movement. Frowning, squinting, smiling, raising eyebrows, all common facial expressions, result from muscle movement. These in turn can cause frown lines or “11s”, crow’s feet aka lateral canthal rhytids and forehead lines. These repeated muscle movements result in wrinkles. Selectively targeting the muscles involved in each of these movements, injecting the appropriate dose and location, allows for the skin to smooth out and offer a rejuvenated look.3
One of the advantages of neurotoxin injections is their precise, targeted placement, which can create beautiful results. However, one challenge is that you don’t see the full effects of placement for two full weeks. This means that patience, attention to detail and practice will be paramount in successful injections.
 |
|
Injecting 4.0 units of neurotoxin into the corrugator muscle. Click image to enlarge. |
One Size Does Not Fit All
The biggest mistake I see is new injectors taking a cookie cutter approach to each patient, treating them all the same. Ultimately, a tailored approach will result in meeting patients’ needs and exceeding their expectations, and this precise delivery ensures natural looking results. I want my patients to look well rested and more youthful, not overdone and obvious. Patients should still have some movement and be able to show emotion. I do not want to rob people of their unique facial characteristics or the ability to emote.
This balance between preserving facial expressions and wrinkle reduction is the hallmark of a great injector. It’s also why this procedure is such a popular choice for those seeking subtle, yet highly impactful, improvements in their appearance-and it starts with their eyes. Notably, when patients have dry eye disease, then there are no injections in the orbicularis oculi as this can dampen the blink and exacerbate their disease. Another reason why eyecare providers are primed to perform this procedure!
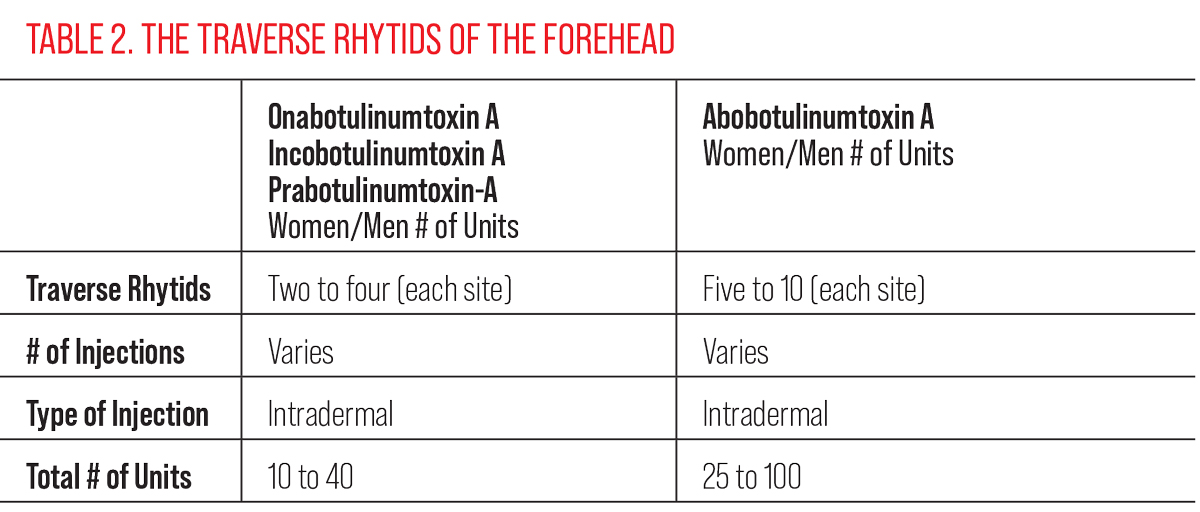 |
| Click table to enlarge. |
To enhance the periorbital region, first understand the muscles and their actions (Figure 5). Remember the skin around the eyes is thinnest on the body and therefore shows aging more quickly. If we want to paralyze a muscle temporarily with neurotoxin, we must understand its opposing result. If we paralyze a depressor, we create elevation. If we paralyze an elevator, we create depression.
 |
|
Injection sites (top) and post-injection and lack of movement (bottom). The Xs depict where I would inject this patient. Click image to enlarge. |
The Procedure Process
Neurotoxin injections are renowned for their safety profile and minimal downtime. The procedure done in the right patient is generally well-tolerated and has few side effects. The most common are headache and redness. Swelling and bruising can also be common at the injection site. Patients usually return to their normal activities after treatment as long as there is no hat or pressure placed on the injection sites for the first few hours after treatment that would diffuse the medication causing it to migrate to a muscle that you don’t want to paralyze. Our understanding of the periorbital muscles makes eyecare providers the perfect injectors, if that is something you desire.
To reconstitute the drug, use the manufacturer’s and FDA’s recommended dilution rates. For onabotulinumtoxin-A, incobotulinumtoxin-A and prabotulinumtoxin-A, the dilution rates are 2.5mL into a 100-unit vial with 0.9% sodium chloride which results in 4.0 units per 0.1mL dose. For daxibotulinumtoxin-A, the dilution rates for a 100-unit vial are double that of onabotulinumtoxin-A, so 8.0 units per 0.1mL dose. These dilution rates give you 4.0 or 8.0 (for daxibotulinumtoxin-A) units respectively per 0.1mL dose, which has migration at about the size of a nickel. Having 2.0 or 4.0 (for daxibotulinumtoxin-A) units will have migration of approximately the size of a dime. Abobotulinumtoxin-A is diluted according to the manufacturer’s guidelines for a 100-unit bottle at 3.0mL of 0.9% sodium chloride diluent added results in 10.0 units per 0.1mL dose.
See Tables 1, 2 and 3 for the typical number of injection sites, units, and type of injection for each facial area.
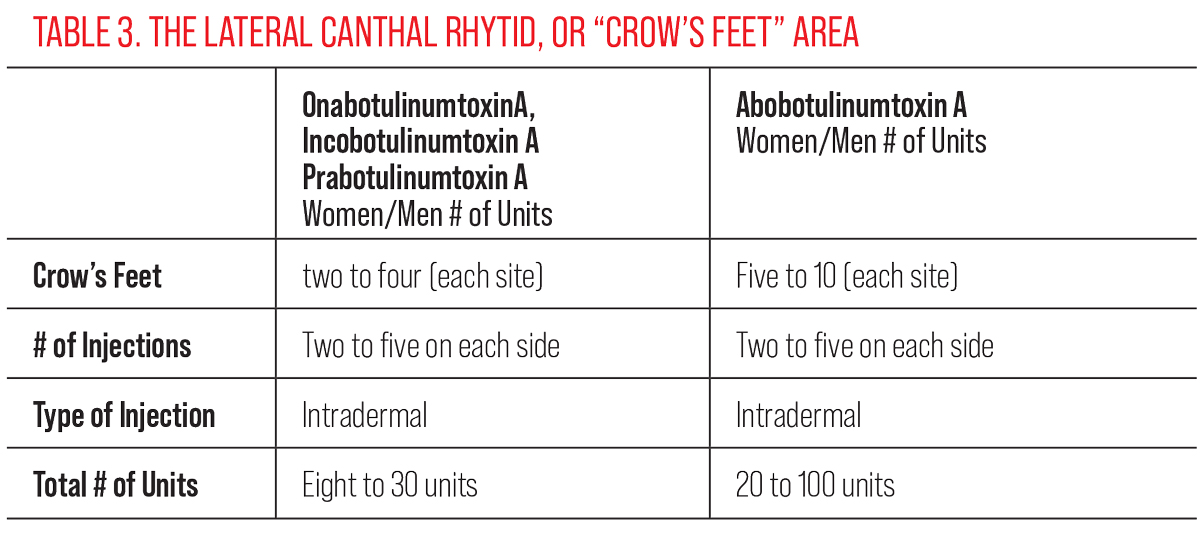 |
| Click table to enlarge. |
Store reconstituted medication in refrigerator between 2º to 8º C. Best practices are to use it within seven hours of dilution, but there was a consensus paper that showed it can be stored for up to four weeks, with 87% potency using preserved or bacteriostatic saline preferably.4 The stored medication should be clear, colorless and free of particulate matter before being administered.
 |
Injecting 2.0 units of neurotoxin into the frontalis muscle. Click image to enlarge. |
Neurotoxin injections for aesthetics provide results that can last anywhere from three to six months. Individual experiences with how long it lasts depend on that person, their metabolism rates and how much they use the muscle. I have patients return to my clinic in two weeks to fully assess their result and see if they need a touch up if I’m injecting them for the first time. This allows me to learn their specific anatomy and correct any muscle that may need an adjustment. After that, patients are scheduled every 90 days to receive their injections. I do often combine neurotoxin alongside energy-based devices that address redness and pigment as well as also build collagen. I always wait at least two weeks before performing an energy-based treatment like intense pulsed light, radiofrequency or laser resurfacing.
Takeaways
The power of neurotoxin injections in eye care is in our ability to deliver precise, safe and impressive results to our patients. They value our relationship that is built on trust and the optometrist’s proficiency in other procedures. I have many patients who have had prior injectors that have given me great confidence by saying, “This is the best I’ve ever looked, it’s so natural and I’m thrilled with the results. I’m never having anyone else inject me.”
 |
| Injecting 2.0 units of neurotoxin into the orbicularis oculi. Click image to enlarge. |
These injections offer a minimally invasive solution to address periorbital concerns that come with aging. Helping patients with rejuvenation can be a transformative experience for both your patient and you. So, go out there and enhance beauty in whatever way you can.
Dr. McGee is founder and owner of BeSpoke Vision, a boutique private practice that offers patients a wide range of optometric care. She is also an adjunct assistant professor at the Northeastern State University College of Optometry and on faculty at the Oklahoma Medical Research Foundation at its Sjögren’s clinic. She is a fellow of the American Academy of Optometry, a diplomate of the American Board of Optometry and is past president of the Oklahoma Association of Optometric Physicians. Dr. McGee consults for Allergan, Kala Pharmaceuticals and Novartis Pharmaceuticals.
Dr. Lighthizer is the associate dean, director of continuing education and chief of specialty care clinics at the NSU Oklahoma College of Optometry. He is a founding member and immediate past president of the Intrepid Eye Society. Dr. Lighthizer’s full disclosure list can be found here.
1. Carruthers J, Carruthers A. The use of botulinum toxin type A in the brow and periorbital rhytides. Semin Cutan Med Surg. 2007;26(2):66-70. 2. Kane MA, Lorenc ZP. Botulinum toxin and the brow: evolution of a technique. Plast Reconstr Surg. 2013;132(3S):7S-15S. 3. Lorenc ZP, Smith S. Chemical brow lift with botulinum toxin. Aesthetic Plast Surg. 2017;41(5):1060-6. 4. Carruthers J, Fagien S, Matarasso SL; Botox Consensus Group. Consensus recommendations on the use of botulinum toxin type a in facial aesthetics. Plast Reconstr Surg. 2004;114(6 Suppl):1S-22S |

