 |
Eliminating the anxiety of having to go “under the knife” goes a long way for most patients. Lid-everting sutures, also referred to as Quickert sutures, are simple to use, low cost and can drastically help. Being able to provide a functional change that greatly impacts your patient’s quality of life is enough of an incentive to add this to your office-based procedure arsenal.
Background
Characterized as the inward turning of the eyelid margin, entropion occurs in up to 2.4% of people over 60 years of age.1 The inward turning of the eyelid margin causes the eyelashes to come into contact with the corneal and conjunctival surfaces, resulting in irritation (Figure 1). This resulting secondary trichiasis, if left untreated, can lead to chronic ocular surface disease and subsequent keratinization of the cornea.
 |
|
Fig. 1. Involution entropion in the right eye. Click image to enlarge. |
Entropion pathogenesis is multifactorial and consists of overriding of the preseptal orbicularis muscle, disinsertion of the lower eyelid retractors, increased horizontal laxity of the tarsus and canthal tendons, scarring from prior surgeries, radiation and trauma.1
Entropion can be classified as involutional, spastic, congenital or cicatricial. Of these, only involutional and spastic apply to this article. Conservative treatment consists of lid taping, bandage contact lenses and artificial tears. However, these treatments do not address the underlying cause of the condition. Thus, the majority of cases will require some sort of corrective surgical measure, and therefore having the capability to offer one in-office is very advantageous.
 |
|
Fig. 2. Subcutaneous injection of Lidocaine 2% with epinephrine done to provide proper local anesthesia. Click image to enlarge. |
First described in 1971, double-armed Vicryl absorbable sutures are safe, minimally invasive, effective, low cost and can be used in the office to address involutional and spastic entropions.2 By inducing scar formation between the tarsal plate and low lid retractor, lid eversion is achieved to a more neutral/natural position. Additionally, this scarring between the orbicularis oculi and the lower lid retractors prevents the overriding of the preseptal orbicularis oculi muscle.3
Patient selection and expectation is an important aspect to consider. For this procedure, only involutional and spastic entropion cases, where horizontal lid laxity is not the main contributor, are candidates. This is due to the fact that its method of action is tightening of the lower lid retractors, and therefore it does not address any horizontal lid laxity. Evaluating dehiscence of the lower lid retractors can be achieved by having the patient look downward and measuring the descent of the lower lid. The lower lid should descend 3mm to 4mm; if this is diminished, it is an indicator of dehiscence or disinsertion of the retractors.4 Horizontal lid laxity can be evaluated by pulling the lower lid laterally while the patient is looking straight ahead and measuring the displacement from the medial canthus or puncta, then repeated medially measuring lateral canthus displacement. Normal displacement is from 0mm to 2mm.5 Moreover, patients who do not wish to pursue or who do not qualify for traditional lid surgery are good candidates. Additionally, blood thinners do not have to be stopped prior to the procedure.
 |
|
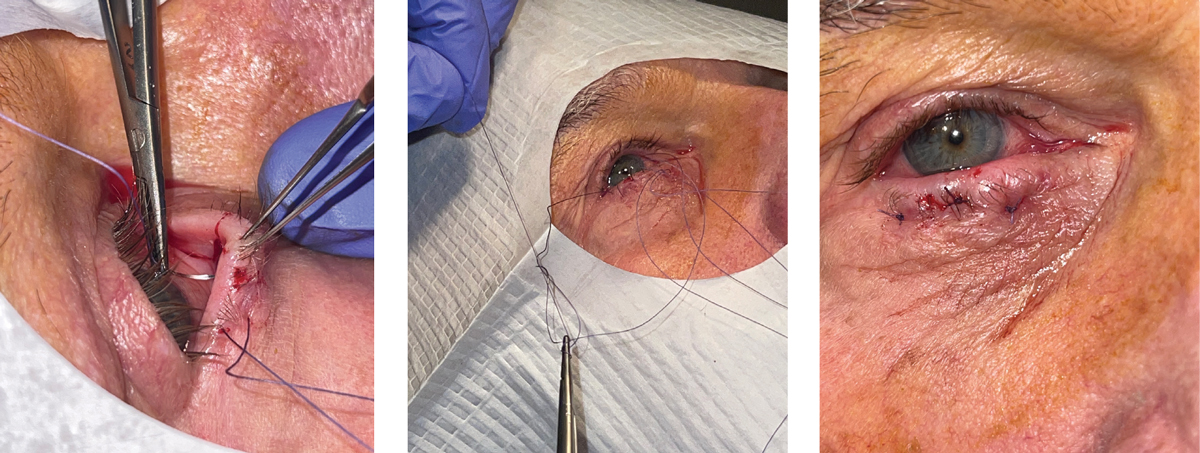
Figs. 3-5. The first arm of the second suture being thrown in the central third of the eyelid (left). Tying of the knots (middle). Immediate post-op appearance (right). Notice the slight ectropion immediately following the procedure, which is the clinical endpoint to shoot for. Click image to enlarge. |
Procedural Technique
The procedure consists of three horizontal mattress sutures placed medially, centrally and laterally in the entropic lid. All sutures enter from the inferior conjunctival fornix and exit on the external side of the lid just inferiorly to the lash line. The everting sutures transfer the pull of the attenuated lid retractors to the anterior surface of the tarsal plate. Moreover, a horizontal barrier above the preseptal orbicularis is created to prevent further upward migration.6 The main prognostic factor for permanence of the procedure depends on the extent of the fibrosis created.7 The fibrotic response has been reportedly demonstrated as early as two weeks.6
The equipment required for the procedure is shown in Table 1. Sterilize the operative lid with a betadine or iodine swab, making sure to sterilize both the upper and lower lids extending downward to the cheek. Divide the lower lid into thirds, paying close attention to the puncta to ensure it does not get everted. The use of a surgical marker is highly suggested for the first few cases.
Anesthetize the palpebral conjunctiva by use of a topical anesthetic, for example proparacaine 0.5%. This is followed by the lower lid being injected with 1mL to 2mL of 2% lidocaine HCl with 1:100,000 epinephrine into the subciliary skin and palpebral conjunctiva (Figure 2). It is advised to test the anesthesia by palpating the target tissue with sterile forceps. Once proper anesthesia is achieved, decide on which side of the lid to begin.
Table 1. Recommended Instruments and Supplies
|
For simplicity’s sake, this article will begin with the lateral third of the lower lid first. A 5.0 double-armed polyglactin absorbable Vicryl suture on an S-14 needle is recommended and is held using a needle driver in the dominant hand. The first arm of the suture is placed deep in the inferior fornix through the lower palpebral conjunctiva. To ensure it pierces through and engages the lower lid retractors, roll the wrist upward as you pass the needle through the capsulopalpebral fascia. This will also allow for the proper passing of the needle to exit the external side of the lid.
Holding the forceps in the non-dominant hand, pull the protruding needle through. It should be exiting the external side of the lid 2mm below the lash line. A greater everting effect is achieved by having the sutures deeper in the fornix and closer to the lash line.8 Once the needle and suture have been pulled through and sufficient slack is left, the second arm of the suture is then ready to be placed. The second arm is placed 2mm to 3mm medial to and at the same level of the first arm.
Using the same technique described previously, the second arm should be exiting 2mm below the lash line. Again, being adjacent to and at the same level of the first arm. Once the second arm exits externally, use forceps to pull the slack evenly on both sides. The second suture is placed at the central third of the lower lid in the exact same manner as the first (Figure 3). Again, ensuring both arms are exiting at the same level, 2mm below the lash line. The third and final suture is placed at the medial third of the lower eyelid. It is imperative to stay lateral to the lower puncta. Doing so will avoid punctal eversion, which occurs when the sutures are placed too proximal to the puncta.
Tying the sutures can be done immediately after passing both arms of the needle through the lower lid or after all three sutures have been placed (Figure 4). To mitigate tangling, cutting off the needles on the sutures is recommended prior to tying them. When tying the suture, it is recommended to use at least a three-throw technique to ensure proper eversion. When pulling taut, ensure that no tissue strangulation occurs from over-tightening. The clinical endpoint immediately after the procedure should result in a slight ectropion (Figure 5). Once all three sutures have been successfully tied, a topical antibiotic ointment, such as erythromycin, is placed over the sutures and along the palpebral side of the lid.
It is advised to prescribe a topical antibiotic ointment with good gram-positive coverage for a course of at least two weeks. It is recommended to follow-up with the patient in 10 to 14 days.
 |
|
Fig. 6. The 10-day post-op visit. Note the perfect position of the eyelid margin. Click image to enlarge. |
Follow-up
The patient is instructed to apply the topical antibiotic ointment bid to the sutures for one week then Qhs for one week. Furthermore, the patient should be instructed not to get the sutures wet, as well as no prolonged bending or heavy lifting for the two weeks following surgery. By the
two-week point, lower lid retractor fibrosis is achieved.6 The sutures can be left to absorb on their own, and the knots can be trimmed at the follow-up (Figure 6). A final follow-up can be set at the six-week point to ensure proper healing.
The recurrence rate is variable according to multiple sources. At the two-year mark, it has been reported to be as low as 15% and as high as 42.9%.6,9 The key factor to mitigating recurrence lies in patient selection. As stated earlier, this procedure does not address entropions with significant horizontal lid laxity. Another appealing feature of the procedure is that it is repeatable, with even lower rates of recurrence.10 This quick in-office procedure is cost-effective with good medical reimbursement for those medical optometrists practicing in states with broadened scope.
Dr. Daniel specializes in ocular disease and refractive surgery at Edmond Regional Eye Associates in Edmond, Oklahoma, having received advanced clinical training in the diagnosis and management of ocular disease and is certified in laser vision correction, anterior segment laser procedures and other minor surgical procedures . Dr. Daniel is a fellow of the American Academy of Optometry, as well as a diplomate of the American Board of Optometry He has no financial disclosures.
1. Weber AC, Del Monte MA, Goel S, et al. Entropion. EyeWiki. eyewiki.aao.org/entropion. Last updated September 24, 2022. Accessed January 27, 2023. 2. Quickert MH, Rathbun E. Suture repair of entropion. Arch Ophthalmol. 1971;85(3):304-5. 3. Lubis RR, Sari ND, Hutasoit H. Quickert procedure for involutional lower eyelid entropion: a multi-centre study. Bali Med J. 2020;9(3):636-9. 4. Shorr NM, Douglas RMP, Goldberg RAM, Schwarcz RMM. (2004). Three-suture technique addresses involutional entropion in the office. Healio. www.healio.com/news/ophthalmology/20120331/three-suture-technique-addresses-involutional-entropion-in-the-office. February 15, 2004. Accessed January 27, 2023. 5. Labib AM, Patel BC, Milroy C. Lower eyelid laxity examination. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Last updated October 19, 2022. Accessed January 27, 2023. 6. Wright M, Bell D, Scott C, Leatherbarrow B. Everting suture correction of lower lid involutional entropion. Br J Ophthalmol. 1999;83(9):1060-3. 7. Seiff SR, Kim M, Howes EL Jr. Histopathological evaluation of rotation sutures for involutional entropion. Br J Ophthalmol. 1989;73(8):628-32. 8. Chen CY, Lai CH, Chu YC, Liao YL, Wang JJ, Chen WD, Tsai YJ. Using A modified quickert procedure combined with prolapsed fat and preseptal orbicularis muscle removal to correct involutional lower eyelid entropion in Asians. Biomed J. June 23, 2022. [Epub ahead of print]. 9. Nakos EA, Boboridis KG, Kakavouti-Doudou AA, Almaliotis DD, Sioulis CE, Karampatakis VE. Randomized Controlled Trial Comparing Everting Sutures with a Lateral Tarsal Strip for Involutional Lower Eyelid Entropion. Ophthalmol Ther. 2019;8(3):397-406. 10. Mohammed BR, Ford R. Success rate of nurse-led everting sutures for involutional lower lid entropion. Eye (Lond). 2017;31(5):732-5. |

