Contact Lens Close-upThe August issue of Review of Optometry is our 47th annual contact lens report, where we help you use new and old techniques to improve your fitting skills. |
A successful initial contact lens fitting is not the experience of many patients. In fact, a recent study that evaluated the incidence of contact lens discontinuation and associated factors in neophyte wearers found that nearly half of patients who stopped wearing their newly fitted lenses did so within the first two months.1 The most common reasons reported by participants included poor vision (42%), handling problems (15%) and discomfort (14%). Importantly, most patients in this study (71%) were not offered any alternative lens or management strategy, which also contributes to early lens dropout.1
What can we do as clinicians to reduce neophyte dropout? There is a host of factors to consider when selecting the most appropriate contact lens for a patient including vision goals and expectations, type and severity of refractive error, ocular surface health, age and lifestyle, to name a few. In this article, we discuss how to get ahead of the common causes of early lens discontinuation and stack the odds in your favor even for your more challenging patients.
1. Vision Concerns
Let’s begin by discussing the primary reason why patients discontinue contact lens wear: quality of vision.2 There are numerous circumstances that could cause a patient to be unsatisfied with the vision provided by their new lenses, including unmet (or undiscussed) vision goals and expectations, misleading in-clinic vs. real-world visual experience and fitting challenges specific to certain types of refractive errors.
Below, we discuss the potential culprits of poor vision to look out for in various types of contact lens wearers.
Goals and Expectations
One of the most important responsibilities that influences first-fit success is the need to ensure reasonable expectations of vision performance are set before selecting a contact lens. It is essential to ask the patient about their visual goals, a discussion that will invariably include the patient’s type of work, hobbies and recreational activities that may influence the successful use of contact lenses.
Besides obtaining sharp vision at all distances, visual goals may include the reduction of glare, UV protection, reduction of spectacle-related distortion and cosmesis and avoidance of fogging of spectacle lenses (as became an important concern following the mask mandates that began during the COVID-19 pandemic).3 In addition, a discussion on the steps involved in the fitting process may help patients understand what to expect.4
Once a contact lens is selected, a brief review of the level of vision the patient should anticipate may help set realistic expectations. It’s also helpful to communicate to patients that they should schedule a follow-up or call the clinic if expectations aren’t being met for an opportunity to troubleshoot or try an alternative lens.
In-clinic vs. Real-world
The in-clinic visual experience with diagnostic lenses should mimic actual wear as much as possible. Researchers studying patient acceptance of multifocal vs. monovision contact lenses emphasized this when it became clear from the study that patients’ in-clinic experience was better with monovision contact lenses, but their real-world experience was better with multifocal contact lenses.5 Be aware that conditions (such as lighting, working distance and availability of expert advice) in the clinic are usually skewed to provide a good experience, but that testing the lenses in the “real world” may change the patient’s experience of the trial lenses.5
Astigmatism
Neophyte contact lens wearers with astigmatism are significantly more likely to discontinue wearing their new toric contact lenses compared with those requiring spherical correction.6,7 However, patients with low amounts of astigmatism (1D and lower) should be offered the benefit of a toric contact lens, as objective, subjective, high-contrast and low-contrast visual acuity have all been shown to be superior to correction with spherical lenses in these cases.8,9 It has also been shown that driving performance—a task that demands good distance correction—is better when low amounts of astigmatism are corrected with contact lenses.10 Thinking that high-modulus lenses or aspheric lenses will mask small amounts of astigmatism was shown to be a myth and should not be used as an alternative to correcting low amounts of astigmatism.11
What about higher amounts of astigmatism? It’s important to have trial lenses on the eye and determine rotation after the lenses have settled. The higher the astigmatic correction, the more rotation of the lenses will degrade visual acuity with every 10° of rotation of a 1.75D astigmatic lens causing an additional 0.75D of residual astigmatism.12 LARS adjustment of the axis of the new trial lens can be a solution. This only applies if the lens is truly stable on the eye, and changing to another lens with a different toric stabilization design may be a better option (Figure 1).
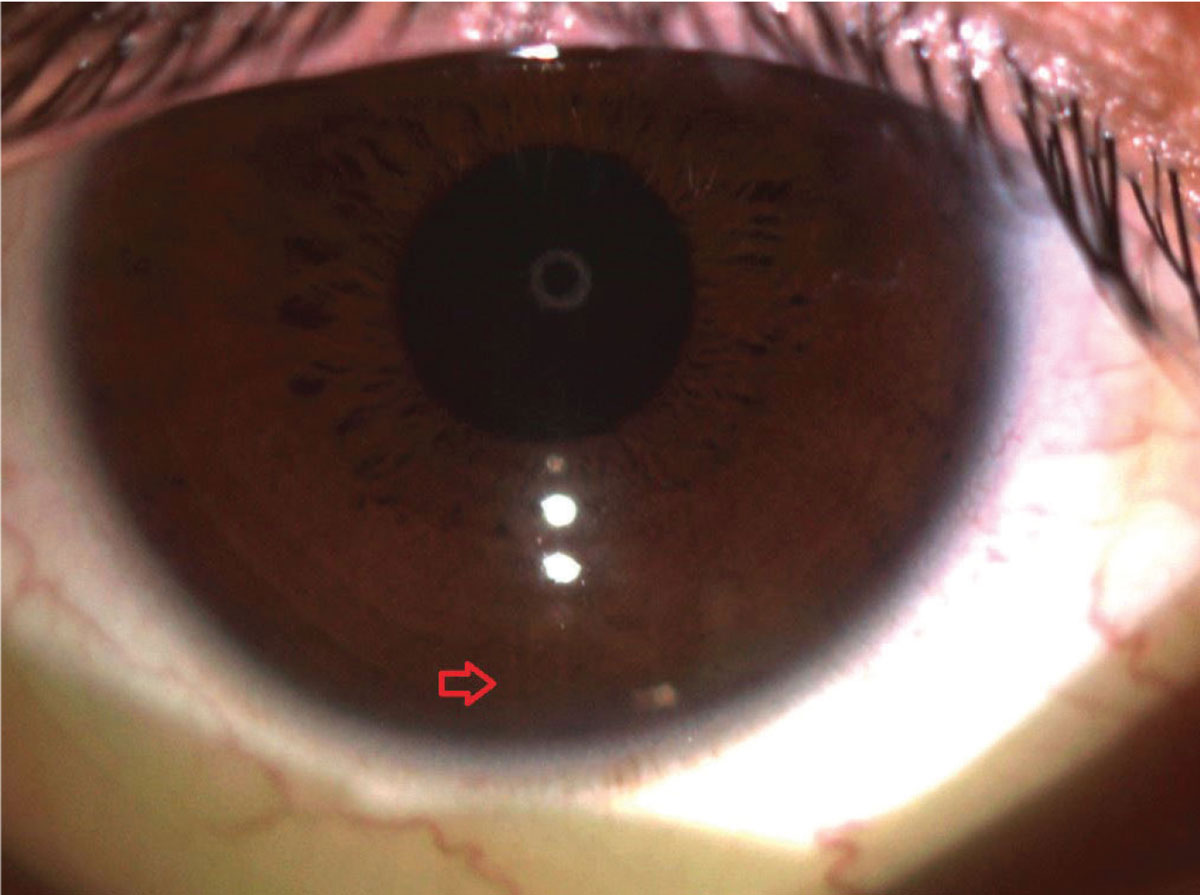 |
|
Fig. 1. Determining the appropriate cylinder axis is essential to ensure the best quality of vision. Pictured here is a soft toric lens aligned at six o’clock. Photo: Vivian P. Shibayama, OD. Click image to enlarge. |
Presbyopia
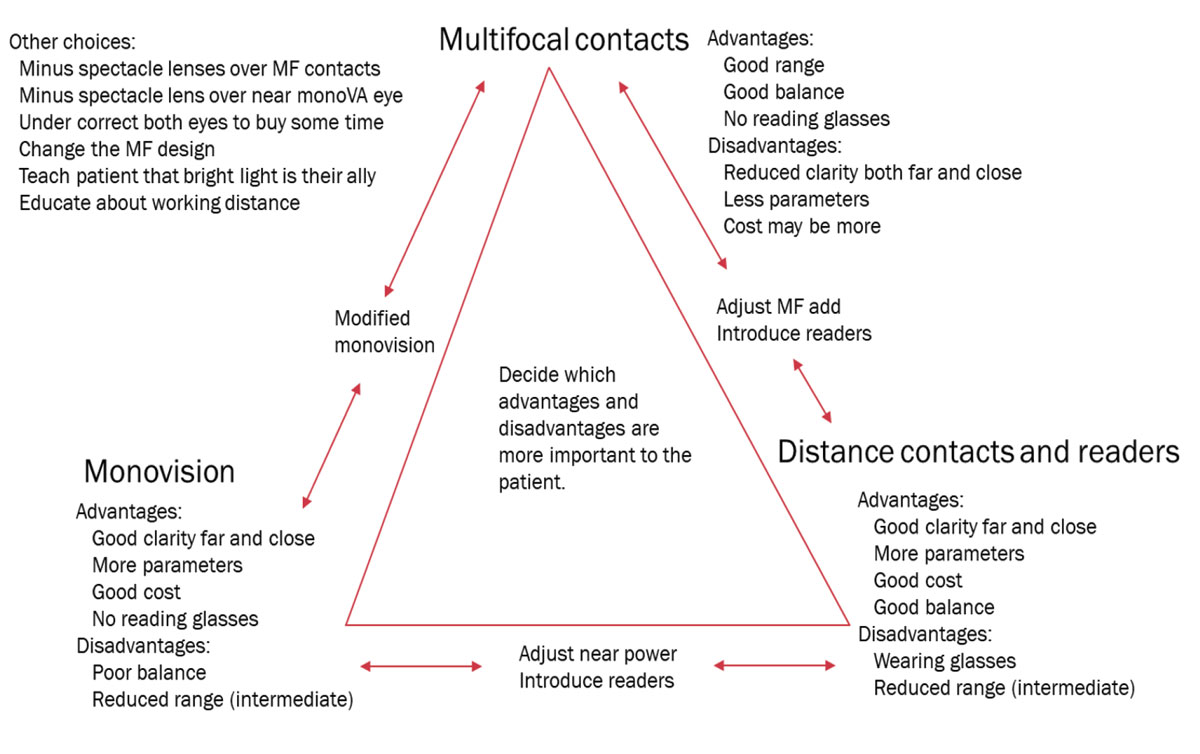
Providing a comprehensive approach to lens fitting for presbyopia can be an invaluable practice builder. An approach tailored to the needs of the patient is most successful, which starts by recognizing the multiple options available that include multifocal, monovision and distance-vision contact lenses with reading glasses (Figure 2). The OD needs to keep in mind that neophyte dropout is highest for multifocal contact lens wearers when compared with toric and spherical lens wearers.1
All these options should be considered and discussed briefly; however, one option should be presented to the patient as the top choice based on the individual’s characteristics and vision goals and needs. The following factors should be taken into account when choosing the most ideal lens for each patient:13
- Range of vision
- Binocular balance between eyes
- Dependence on reading glasses
- Clarity of vision
- Available range of contact lens parameters
- Impact of cost
Also consider and remind patients that an adaptation period of up to 15 days may be required to acclimate to multifocal lenses.14 When one option is deemed less than optimal by the patient, adjustments can be made as shown in the “presbyopia triangle” in Figure 2.
Other tips to increase the chance of success are to keep patients mildly undercorrected in both eyes—as long as distance acuity stays 20/20—or to prescribe a spectacle option to enhance distance acuity that can be worn over undercorrected, multifocal or monovision contact lenses. Patients should understand the impact the distance of their reading material has on acuity, as well as the trade-off between distance vision clarity and the increasing presbyopic add power.15
Those patients who regularly experience mild near blur or strain in single vision contact lenses may benefit from the introduction of a low multifocal add so that future incremental changes can be made more easily as presbyopia progresses.
 |
|
Fig. 2. Dr. Stokkermans created this “presbyopia triangle,” which he uses to teach his optometry students about the different options available for presbyopes interested in contact lenses. (Note: “MF” refers to “multifocal). Photo: Thomas Stokkermans, OD. Click image to enlarge. |
Practitioner preference has certainly changed in the past decade with fitting multifocal lenses becoming increasingly popular (80% in 2021 vs. 63% in 2020) and a drop-off in monovision fits (14% in 2021 vs. 28% in 2020) and spectacles combined with contact lenses (6% in 2021 vs. 9% in 2020).16
Evaluating presbyopic patients for first-time success with contact lenses is what makes the practice of prescribing these lenses both art and science.
Other Refractive Errors
There are generally good options available in our trial lens sets when the spherical power is between -12D and +8D, cyl power is below 2.75D and the bifocal add is no more than 2.50D. When the refractive error surpasses these cutoffs or if oblique astigmatism is present, an empirical diagnostic lens order may be necessary. In these cases, patients should be made aware that the optimal on-eye experience will be delayed and an overrefraction and slit-lamp exam at the initial evaluation may necessitate another lens order.
To avoid vertex adjustment errors when a spherical trial lens order is based on the refraction, place the closest available power contact lens on the eye and perform a careful sphero-cylindrical overrefraction. If the overrefraction is under 4D, a vertex adjustment is not necessary. Otherwise, measure the vertex distance of the overrefraction, making sure that each meridian is individually vertex-adjusted to ensure greatest accuracy. Similarly, for cylindrical powers that must be empirically ordered, the closest cylinder power with the same axis as the one that will be ordered should be placed on the eye to assess fit and rotation. This overrefraction can avoid additional orders and time by maximizing the likelihood that the new trial lens is the correct prescription. If the lens is unstable on initial evaluation with the lower power, then a different toric lens design or manufacture should be considered.17
Enough Options?
Many patients—particularly those with little or no knowledge or experience with contact lenses—won’t know which options are available unless we educate or, better yet, show them. This is why it’s crucial to have a wide and comprehensive stock of diagnostic contact lenses on-hand in your practice. Allowing patients to try multiple types of lenses in-clinic will provide them with more options to choose from to help find the one best suited for their unique needs and desired level of vision.
Introducing both an entry level and a premium lens option or even a “good, better, best” approach and dispensing trial lenses can greatly help patients gauge their level of satisfaction for each. The same holds true for providing different presbyopia options (e.g., a low multifocal add in both eyes along with a high multifocal add as a second option for the nondominant eye).18
Careful consideration should be given to the potential downsides of this approach, as it may devalue the contact lens practitioner’s perceived expertise. Additionally, self-selected choices may cause confusion for those with no prior contact lens experience, or the patient may lose track of which lens they are wearing.
2. Handling Problems
An inability or unwillingness to properly handle contact lenses contributes to nearly one in six cases of lens dropout within the first two months.1 A practical way to prevent or reduce this issue is by increasing in-clinic patient education. A successful application and removal (A&R) training class to ensure patients are comfortable with handling their lenses is essential to avoid rejection at the initial fit or subsequent contact lens dropout.
In older adult first-time wearers, decreased dexterity and sensitivity may be associated with an inability to adequately apply and remove lenses. Even following A&R training, patients may not be ideal candidates for full-time contact lens wear if they are unable to handle them safely and properly. Comorbid ocular disease may also influence success and increase discomfort upon insertion and removal. Careful management of underlying risk factors should be discussed upfront to ensure future expectations of contact lens wear and upkeep will be met.19
While young children may need more training and practice to comfortably insert and remove their lenses, one study found that patients as young as eight are able to successfully handle soft contact lenses with only 5% requiring an additional training class and only 2% unable to wear the lenses due to inability of handling.20
A&R training on the day of the fit allows you to make immediate changes in lens parameters to account for the patient’s ability to handle the lenses. For example, noticing during training that a patient quickly rips a lens may prompt a switch to a material with a different lens modulus. A patient who cannot remove a lens because it feels too slippery may benefit from one with lower lubricity and modulus or a different edge design.21 This is another reason why ensuring you have a wide assortment of diagnostic contact lenses in your practice is essential for first-fit success.
Follow-up visits will allow for adjustment of the trial lenses and to address concerns that may have arisen during the trial wear period. These visits have been on the decline due to practitioner perception that newer-generation lenses are safer with less complications, as well as the temporary reduction in access to eye care throughout the COVID-19 pandemic.22
The fact that 71% of patients who dropped out of contact lens wear were never offered an alternative lens—according to the study cited in this article’s introduction—drives home the need for clinicians to make a greater effort to find solutions to the problems leading to patient dissatisfaction.1
3. Discomfort
The third leading cause of neophyte dropout in contact lens wearers is ocular discomfort. It’s a two-way street: contact lenses can impact the ocular surface, and the ocular surface can impact the success of first-fit contact lenses.23 Both the type of lens prescribed and the presence of diagnosed or undiagnosed ocular disease can affect the initial and long-term comfort of contact lenses. A thorough evaluation and history can uncover ocular and general health conditions that will need to be addressed to achieve initial-fit success. Depending on the condition’s severity and the patient’s desire to wear contact lenses, the ocular and systemic conditions may need to be managed prior to introducing the first contact lens.
 |
|
Fig. 3. Different ocular conditions affecting the ability to wear contact lenses will have to be treated prior to the intial fitting and will require a specific fitting approach (left to right: keratoconus with Fleisher ring, giant papillary conjunctivitis and meibomian gland dysfunction). Photos left to right: Elyse L. Chaglasian, OD, Tammy Than, MS, OD, Melissa Barnett, OD and Doan Huynh Kwak, OD. Click image to enlarge. |
Type of Lens
In 2021, 43% of all contact lens wearers were prescribed daily disposables in the United States, a percentage that has been creeping up especially in recent years.24 Subjective comfort is generally better for daily disposable lenses compared with reusable ones.25 However, other attributes of daily disposable lenses such as parameters, diameter and material need to be considered when deciding to fit a daily disposable lens to provide the best comfort.
Lens material can affect comfort of wear, though the evidence is not definitive due to confounding factors. In 2022, the majority (58%) of all fits were with silicone hydrogel (SiHy) lenses, which have been reported to improve comfort and extend the number of hours the lenses can comfortably be worn.26,27 However, a meta-analysis of multiple studies revealed that SiHy lenses do not necessarily provide superior comfort, but rather, similar to daily disposable lenses, other parameters all play an important role, such as lens design and material, replacement regimen and the type of lens cleaner.28
Dry Eye and Blepharitis
While the treatment and management of dry eye and blepharitis is beyond the scope of this article, these conditions that affect the ocular surface should be carefully evaluated and treated before or concurrently when prescribing any contact lens (Figure 4). A decreased tear break-up time and increased tear evaporation have been associated with dry eye symptoms during contact lens wear.29
Many studies suggest that patients with existing dry eye disease and blepharitis achieve the best comfort when fit with daily disposable contact lenses as long as the dry eye management is implemented concurrently.30
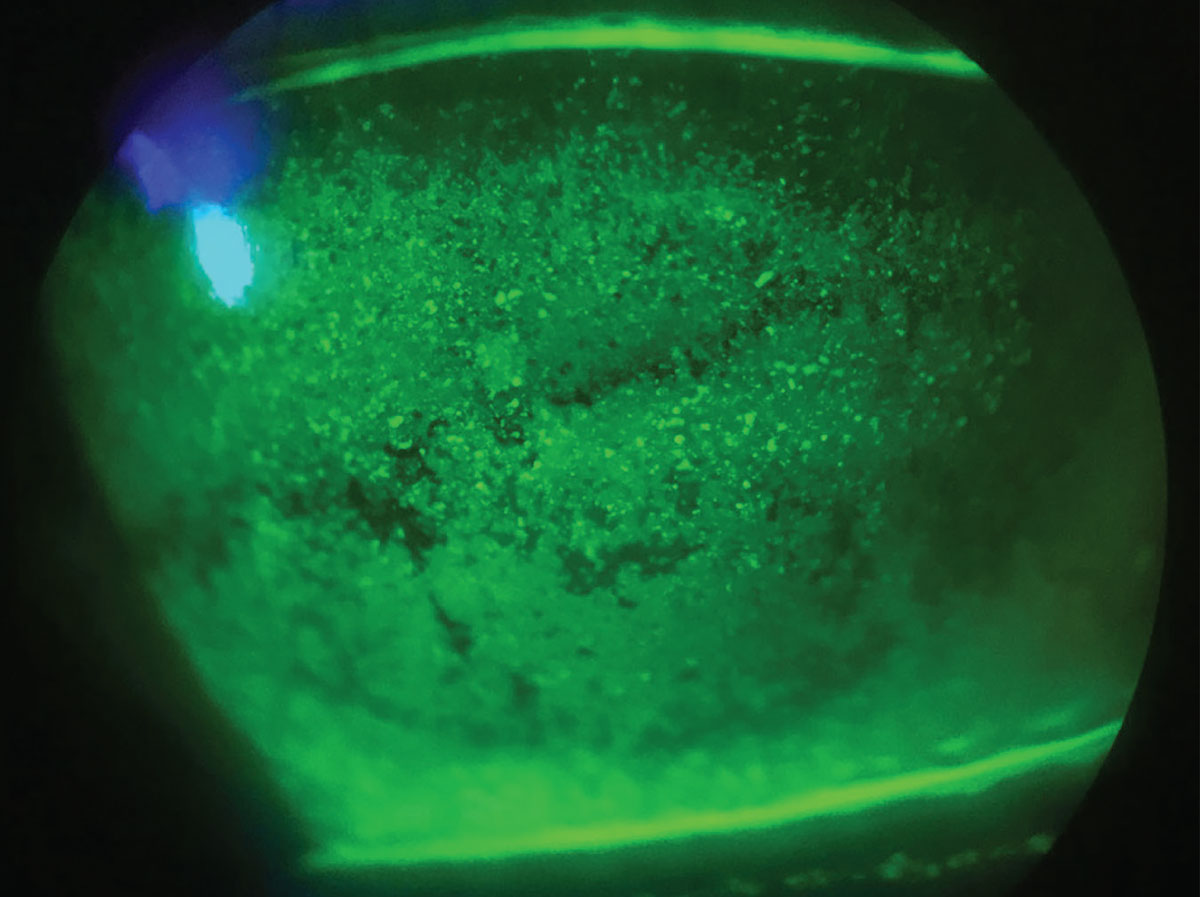 |
|
Fig. 4. Patients with signs and/or symptoms of dry eye may need to be evaluated and treated prior to contact lens selection and fitting. Photo: Alexandra Wiechmann, OD. Click image to enlarge. |
Allergies and Giant Papillary Conjunctivitis
The best way to avoid causing allergic conjunctivitis and giant papillary conjunctivitis (GPC) with newly fit contact lenses is for the practitioner to take a good medical history. An evaluation of ocular redness, conjunctival chemosis and the presence of papillae—including GPC—is central. While many practitioners do not routinely evert the eyelid, it is indicated in those patients with an allergic/atopic profile. The lower tarsal conjunctiva should be routinely evaluated for signs of allergies.
Patients with multiple allergies and those with atopic disease are best candidates for daily disposable lenses that are low in modulus and have consistent high lubricity. Some SiHy lenses—especially early generation ones that were not designed for a daily disposable modality—have a high modulus. These lenses may cause “localized” GPC with large papillae in the central upper tarsal conjunctiva.31 SiHy lenses may also attract lipid deposits that reduce lubricity.32
While lens cleaning with a peroxide-based solution is a hypoallergenic option, patients need to follow the instructions carefully. This cleaning system is not conducive to intermittent use of contact lenses. However, it does provide longer, more comfortable wear time for patients wearing SiHy lenses.33
Treatment with allergy medications is certainly an option, but try to avoid systemic antihistamines whenever possible, as these may exacerbate dry eye symptoms. Most allergy drops are taken once or twice daily, and it’s important to remind patients that these should be administered without the contact lenses in the eyes.
Takeaways
To maximize the success of the neophyte contact lens wearer, a special emphasis must be placed on factors affecting visual performance, comfort and lens handling.34 With the many advanced technologies and extensive selection of contact lenses practitioners have in their armamentarium, there are many ways to improve the experience of new contact lens patients.
Besides technology, we should not underestimate that in the end, our most effective tools are our abilities to set realistic expectations, educate the patient on the fitting process, provide opportunities for the patient to explain what needs to be improved and include them in the process of deciding which options are available.
Dr. Stokkermans is an associate professor at the Case Western Reserve School of Medicine, director of optometric services at University Hospitals Cleveland Medical Center and an adjunct faculty member of five optometry schools in the US. He is a fellow of the American Academy of Optometry, the chief editor of Advanced Medical Care at www.statpearls.com and a medical writer and reviewer at www.allaboutvision.com. He has participated in over 30 contact lens trials. He discloses financial relationships with Biotissue and Tarsus.
Dr. Louie is a professor of ophthalmology at the Casey Eye Institute at Oregon Health & Science University, where he is the director of the Medical Contact Lens Service, Optometric Services and the Medical Contact Lens Fellowship Program. He is also a fellow of the AAO.
1. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye. 2017;40(1):15-24. 2. Pucker AD, Tichenor AA. A review of contact lens dropout. Clin Optom (Auckl). 2020;12:85-94. 3. Malik SS. A simple method to prevent spectacle lenses misting up on wearing a face mask. Ann R Coll Surg Engl. 2011;93(2):168. 4. Gustafson B. Set expectations for contact lens fits. Optometric Management. October 1, 2019. 5. Richdale K, Mitchell GLM, Zadnik K. Comparison of multifocal monovision soft contact lens corrections in patients with low-astigmatic presbyopia. Optom Vis Sci. 2006;83(5):266-73. 6. Sulley A, Young G, Hunt C, et al. Retention rates in new contact lens wearers. Eye Contact Lens. 2018;44 Suppl 1:S273-S282. 7. Young G, Veys J, Pritchard N, Coleman S. A multi-centre study of lapsed contact lens wearers. Ophthalmic Physiol Opt. 2002;22(6):516-27. 8. Cho P, Cheung SW, Charm J. Visual outcome of Soflens Daily Disposable and Soflens Daily Disposable for Astigmatism in subjects with low astigmatism. Clin Exp Optom. 2012;95:43-7. 9. Morgan PB, Efron SE, Efron N, et al. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optom Vis Sci. 2005;82:823-8. 10. Cox DJ, Banton T, Record S, et al. Does correcting astigmatism with toric lenses improve driving performance? Optom Vis Sci. 2015;92:404-11. 11. Bernstein P, Gundel R, Rosen J. Masking corneal toricity with hydrogels: does it work? Int Contact Lens Clin. 1991;18:67-70. 12. Jackson JM. Back to basics: soft lenses for astigmatism. Contact Lens Spectrum. June 1, 2012. 13. Michaud L. Seven steps to success in multifocal fitting. Review of Optometry. August 15, 2022. 14. Fernandes PR, Neves HI, Lopes-Ferreira DP, Jorge JM, González-Meijome JM. Adaptation to multifocal and monovision contact lens correction. Optom Vis Sci. 2013;90(3):228-35. 15. Bennett ES, Quinn TG. Multifocal lens decision-making 101. Contact Lens Spectrum. April 1, 2014. 16. Nichols JJ, Starcher L. Contact lenses 2021. Contact Lens Spectrum. January 1, 2022. 17. Kading D, Fischer A. Turn up your toric lens fitting, astigmatism-correcting designs are available in soft, GP, and scleral lens options. Contact Lens Spectrum. June 1, 2020. 18. Sha J, Tilia D, Kho D, et al. Visual performance of daily-disposable multifocal soft contact lenses: a randomized, double-blind clinical trial. Optom Vis Sci. 2018;95(12):1096-104. 19. Zadnik K. Contact lenses in the geriatric patient. J Am Optom Assoc. 1994;65(3):193-7. 20. Paquette L, Jones DA, Sears M, Nandakumar K, Woods CA. Contact lens fitting and training in a child and youth population. Cont Lens Anterior Eye. 2015;38(6):419-23. 21. Efron N, Morgan PB, Nichols JJ, et al. All soft contact lenses are not created equal. Cont Lens Anterior Eye. 2022;45(2):101515. 22. Brujic M, Miller J. Contact lens follow-ups. Optometry Times. July 1, 2014. 23. Jones L, Efron N, Bandamwar K, et al. TFOS Lifestyle: impact of contact lenses on the ocular surface. Ocul Surf. 2023;29:175-219. 24. Morgan P, Woods C, Tranoudis I, Helland M, Efron N. International contact lens prescribing in 2021. Contact Lens Spectrum. 2022;37. 25. Lazon de la Jara P, Papas E, Diec J, et al. Effect of lens care systems on the clinical performance of a contact lens. Optom Vis Sci. 2013;90(4):344-50. 26. Nichols JJ, Starcher L. Contact lenses 2022. Contact Lens Spectrum. January 1, 2023. 27. Riley C, Young G, Chalmers R. Prevalence of ocular surface symptoms, signs, and uncomfortable hours of wear in contact lens wearers: the effect of refitting with daily-wear silicone hydrogel lenses (senofilcon A). Eye Contact Lens. 2006;32:281-6. 28. Guillon M. Are silicone hydrogel contact lenses more comfortable than hydrogel contact lenses? Eye Contact Lens. 2013;39(1):86-92. 29. Craig JP, Willcox MD, Argüeso P, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS123-TFOS156. 30. Pucker AD, Jones-Jordan LA, Marx S, et al. Clinical factors associated with contact lens dropout. Cont Lens Anterior Eye. 2019;42(3):318-24. 31. Dumbleton K. Adverse events with silicone hydrogel continuous wear. Cont Lens Anterior Eye. 2002;25:137-46. 32. Sulley A, Dumbleton K. Silicone hydrogel daily disposable benefits: the evidence. Cont Lens Anterior Eye. 2020;43(3):298-307. 33. Keir N, Woods CA, et al. Clinical performance of different care systems with silicone hydrogel contact lenses. Cont Lens Anterior Eye. 2010;33(4):189-95. 34. Harthan JS, Man MK. Which factors matter in contact lens selection? Review of Optometry. August 15, 2022. |

