
A 52-year-old aphakic patient has experienced repeated retinal detachments and re-pairs. The patient now has silicone oil in the posterior chamber and corneal decompensation with a very low IOP (5mm Hg). Several corneal specialists have recommended an attempt at full-thickness grafting, but one suggested going right to a keratoprosthesis (artificial cornea) given the low IOP and therefore high risk for graft failure. Fortunately, the patient still has 20/30 acuity in the fellow eye. What is the best course of action for this patient?
Youll need four additional pieces of information about this patient before recommending him for either procedure, namely:
The patients current visual acuity and predicted visual outcome. Refer this patient back to his retinal specialist so this practitioner can determine what his predicted visual outcome will be as the result of such surgeries, says ophthalmologist Robert Abel Jr., of Wilmington, Del. There is no point in referring this patient for either procedure if he is not going to gain any vision.
Sadeer Hannush, M.D., a corneal surgeon at Wills Eye Hospital, in Philadelphia, agrees. If this patients vision is light perception or hand motions, and the cornea is not deemed to be the major contributor to the visual deficit, then the prognosis is very guarded, and it may not be a good idea to refer him for either surgery, he says.
The health of the retina. If there is visual potential, ask the retinal specialist if the retina is healthy enough to remove the silicone oil. If the silicone oil has to stay in place, referring this patient for a full-thickness graft may not be a good idea because he does not have an intraocular lens to prevent the oil from burping out and contaminating the new cornea, Dr. Abel says.
The status of the patients ocular surface. If this patient has severe dry eye, that could influence the long-term survival of a corneal transplant. A keratoprosthesis, however, does not have to be wet to the degree that a corneal transplant does. A corneal transplant needs to maintain healthy epithelium, and it needs to nourish the surface of the eye, specifically the cornea, says ophthalmologist Stephen E. Pascucci, of Bonita Springs, Fla. A keratoprosthesis does not require that type of nourishment.
The cause of the low IOP. Determine if this patients low intraocular pressure is due to complete ciliary body shutdown, which means the eye is not capable of maintaining pressure and therefore is prephthisical. It is sometimes difficult to obtain an accurate IOP. Usually, a low pressure is not consistent with graft survival, as it is not consistent with the cornea maintaining its clarity, Dr. Hanush says. Also, over time, the patient will develop corneal folds in Descemets membrane. A keratoprosthesis, however, is not affected by a low IOP.
This patients history warrants at least one initial attempt at corneal transplant, these practitioners say.
A corneal transplant should be done on this patient first because he has better visual acuity potential with human tissue than with a keratoprosthesis, Dr. Abel says. For this reason, the keratoprosthesis companies encourage corneal surgeons to make sure patients have a failed cornea transplant before inserting a keratoprosthesis.
Dr. Pascucci offers additional reasons for attempting a transplant before keratoprosthesis. First, while both procedures share certain risks, such as infection, bleeding and repeat retinal detachments, a keratoprosthesis comes with the added risks of extrusion of the device and chronic inflammation, such as an iritis or uveitis, he says. Second, inserting a keratoprosthesis causes much greater disruption to the ocular surface than a corneal graft does. Third, seeing the retina through a clear cornea transplant is easier than seeing it through a keratoprosthesis, which is important should this patient experience another retinal detachment. Finally, a corneal transplant does not exhibit as much visual disfigurement as a keratoprosthesis, so why make the patient self-conscious if you dont necessarily have to?
A keratoprosthesis should not be the first option unless you and the corneal surgeon feel a corneal transplant has no chance for survival, adds Dr. Hannush. For example, if this patient had four quadrants of neovascularization, then there is little chance for a graft to survive.
So, what keratoprosthetic devices are currently available if the corneal graft fails?
 |
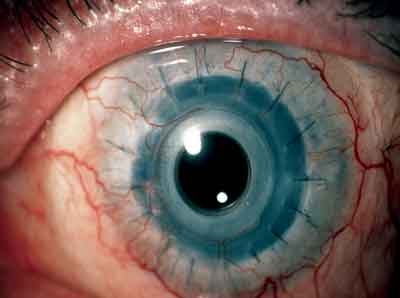 |
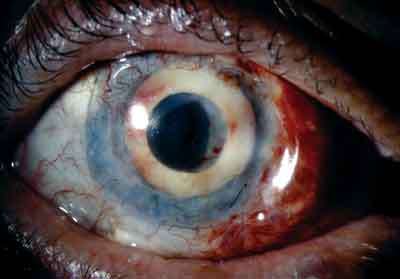
| The AlphaCor keratoprosthesis in a patient who sustained multiple failed corneal grafts (left). The Boston KP in a patient who experienced a graft failure (right). | |
There are two types of keratoprosthetic devices for this patient:
AlphaCor (CooperVision Surgical). This one-piece, artificial replacement cornea is indicated for a patient in whom a corneal graft is likely to fail or a patient who has experienced many failed corneal transplants. The keratoprosthesis replaces the patients diseased or scarred natural cornea. AlphaCor is available in two designs: phakic and aphakic.1
Boston KP (Massachusetts Eye and Ear Infirmary). This two-piece artificial replacement cornea is indicated for patients who have had two failed corneal grafts (in non-autoimmune diseases) with a poor prognosis for another graft. The candidate must have less than 20/400 vision in the affected eye, lower than optimal vision in the other eye and no retinal detachment or end-stage glaucoma.2
Confer with the corneal specialist about which device is best for your patient.
1. CooperVision Surgical. AlphaCor Artificial Cornea. www.coopervisionsurgical. com/coopervisionsurgical/cvs_alphacor.htm. (Accessed August 8, 2006)
2. Massachusetts Eye and Ear Infirmary. Artifical Cornea The Boston Keratoprosthesis. www.meei.harvard.edu/shared/ ophtho/cornea2.php. (Accessed August 8, 2006)
Vol. No: 143:10Issue:
10/15/2006

