 |
|
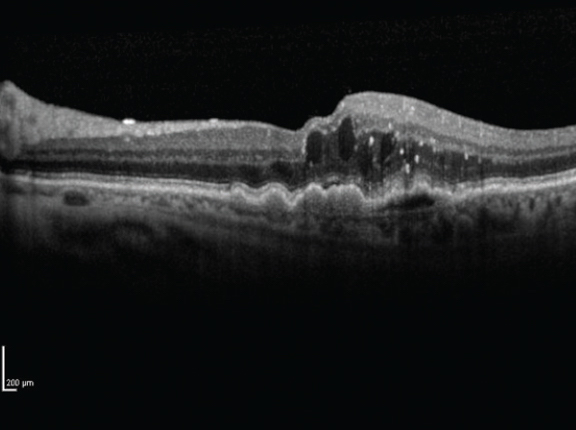
Home OCT devices—once they hit the market—may be an accurate way to remotely assess the progress of anti-VEGF treatment in nAMD patients, if such devices are shown comparable to the gold standard of an in-office scan (pictured). Click image to enlarge. |
The market for home-based OCT testing hasn’t even officially begun but the nascent field is already getting more competitive. A start-up company called OCT Health recently tested the performance of a prototype spectral-domain OCT home device for self-monitoring patients with neovascular age-related macular degeneration (nAMD). Farther along in the FDA clearance process is a similar device called the Notal OCT Analyzer from Notal Vision, which is expected to be released sooner. No head-to-head studies have been conducted and both devices seem promising.
The new prototype device, called RetinaCheck, was found to show excellent agreement to manual human grading. It uses a light source of 840nm and runs at a rate of 20,000 A-scans per second (20KHz). The developers explained in their paper on the study, recently published in Retina, “The two different scan patterns acquired were line and star scans centered at the fovea. The line scan involves five horizontal B-scans evenly separated over a 6mm x 3mm lateral field of view, and each B-scan comprises 700 A-scans of 3mm depth. A star scan comprises six radial B-scans evenly separated over a 6mm x 6mm.” No dilation is required for the scans.
Included in the prospective observational study were 136 OCT scans gathered from 70 patients using the home OCT device. All patients were undergoing anti-VEGF therapy for nAMD. Automated analysis software was used to perform fluid segmentation on images captured by the home OCT device, which was then compared with manual gradings across all retinal fluid types using ROC curves.
The developers reported that fluid detection per B-scan had an area under the ROC curve of 0.95 for intraretinal fluid (IRF), 0.97 for subretinal fluid (SRF) and 0.98 for subretinal pigment epithelium (sub-RPE) fluid. Values were slightly higher when assessed on a per-volume basis.
Segmentation accuracy was also assessed and the measurements represented excellent agreement to manual gradings, the developers explained in their paper.
In summary, the study authors observed that the results were comparable between automated analysis of the home OCT images and manual grading for retinal fluid detection and quantification. As home-based technology in eye care continues to be researched and fine-tuned in response to the growing demand, the developers concluded that their study helps by laying “an important foundation for future studies of the prototype home OCT device and highlights its potential to detect the need for anti-VEGF retreatment outside the clinic.”
Oakley JD, Verdooner S, Russakoff DB, et al. Quantitative assessment of automated optical coherence tomography image analysis using a home-based device for self-monitoring neovascular age-related macular degeneration. Retina. November 17, 2022. [Epub ahead of print]. |

