A Closer Look at EyelidsThe eyelids are the first structure examined under the slit lamp microscope and are often quickly evaluated. Yet accurate assessments of common eyelid conditions and appropriate medical management can improve patients' quality of life. The October issue of Review of Optometry gives readers a rundown on best practices regarding eyelid health. |
The profession is evolving, and more optometric physicians are becoming confident with minor surgical procedures, including the management of eyelid lumps and bumps. Beginning with Oklahoma in 1998, about 17 states now privilege optometrists to perform minor surgical procedures.1 Incorporating these procedures into practice once a state grants surgical procedures is up to the individual doctor. However, we should all have the foundational knowledge to appropriately diagnose and manage, whether that means in-house removal or referral.
Know Your Way Around
A good grasp of eyelid and adnexa anatomy is essential in the management of eyelid lesions. Though eyelid skin is the thinnest anywhere on the human body, it contains an array of structures including epithelium, muscle, fat, tarsus, conjunctiva as well as dermal adnexal structures such as eyelash hair follicles, sweat and sebaceous glands, nerve fibers and associated blood and lymphatic vessels.2 Eyelid neoplasms can derive from any of these structures.3-5
Most eyelid lesions encountered in clinical practice are benign. However, there is some variability in their clinical presentations. This can lead to overlap of characteristics even between benign and malignant lesions.6 Think keratoacanthoma vs. basal cell carcinoma. Interestingly, it has been reported that 2% to 4.6% of lesions diagnosed as benign clinically were found to be malignant on histological examination.7,8 Bearing this in mind, we try to not be too cavalier even when we are confident making a tentative clinical diagnosis. In our office, we send a sample of all excised masses to the pathology department for confirmation.
Histologic terms such as hyperkeratosis, acanthosis and dyskeratosis are useful to pathologists. However, we find it more clinically advantageous to describe neoplasms on the basis of physical characteristics such as size, attachment (sessile vs. pedunculated), ulceration, variation in color, borders, changes to surrounding adnexal structures and whether loosely or firmly attached to underlying tissue.
 |
|
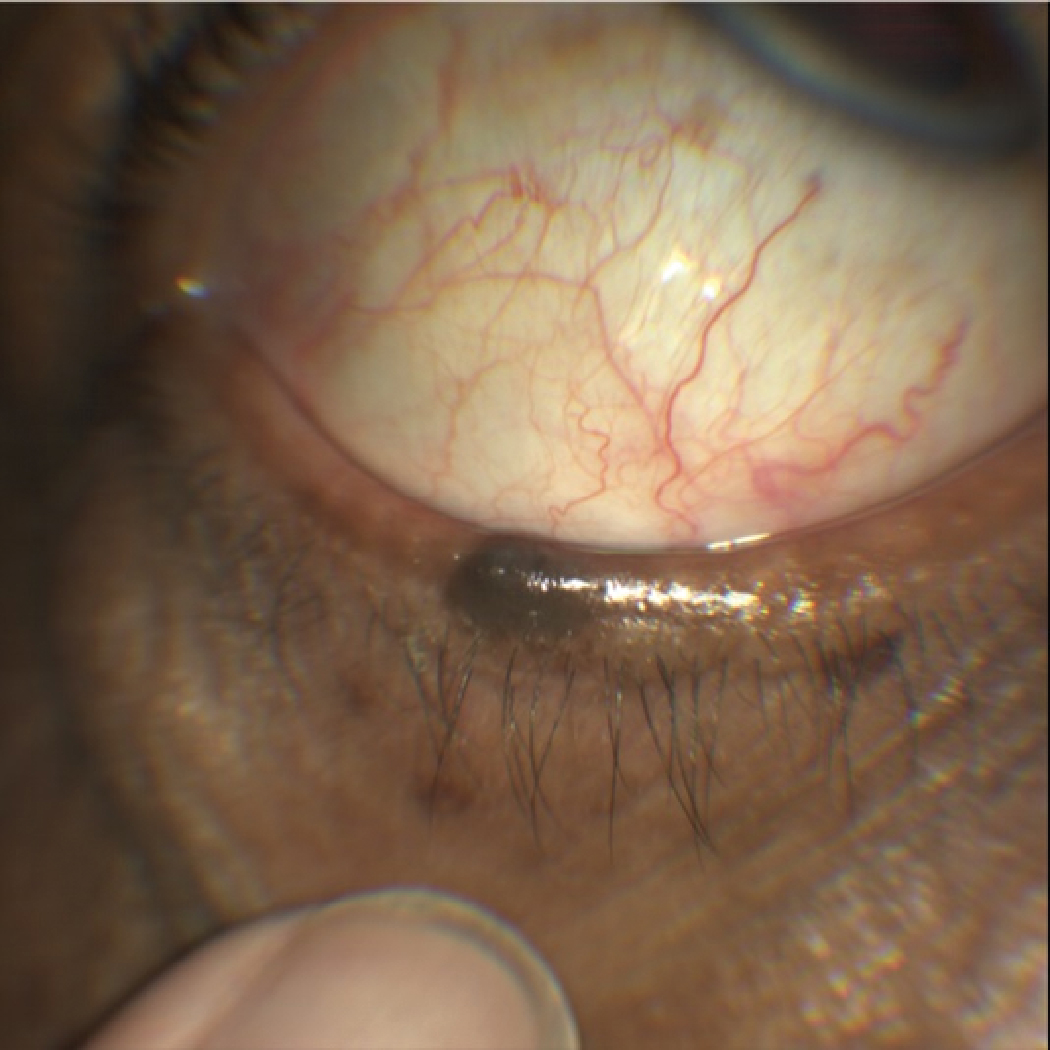
A sebaceous cyst of Zeis. Click image to enlarge. |
In a world where our profession is driven to see more and more patients with ever more complex health conditions, it can be tempting to cut corners. It is, however, incumbent upon the clinician to take a few moments to grossly observe the patient prior to moving on with the eye exam. Much can be gleaned by looking at basic symmetry or the condition of exposed skin of other parts of the body during a face-to-face history.
If you find a lesion of interest, take a pertinent history. Onset, evolution (changes to the lesion over time such as rapid growth, bleeding, crusting, loss of lashes) and changes or variations in color should be assessed. Bear in mind fair complexion, history of excessive sun exposure, prior radiation treatment and especially a personal history of skin cancer would increase suspicion of malignancy.3
A closer look with a slit lamp biomicroscope can enhance your ability to evaluate lesion characteristics. Pay close attention to the overall appearance as well as the surrounding skin and adnexal structures. Normal eyelid structure loss such as madarosis (loss of lashes), poliosis (absence of pigment within the lashes), tylosis (thickened eyelid margins) or deformation of lid position should raise suspicion of malignancy.9 Palpate the lesion and area immediately surrounding to determine whether the lesion is moveable or attached firmly to underlying tissue, and also assess regional lymph nodes for possible involvement. This step is often overlooked, but some malignancies such as squamous cell carcinoma can metastasize to nearby organs via lymph nodes with associated lymphadenopathy. Gauge symmetry to the corresponding node on the opposite side of the head. Photo-documentation is invaluable for monitoring progression.
LESION TERMINOLOGY2Bulla. A large (more than 0.5cm) serous fluid-filled lesion. Crust. Solidified serous or purulent exudate. Cyst. A nodule consisting of an epithelial-lined cavity filled with fluid or semisolid material. Macule. Localized area of color change without infiltration, depression or elevation, less than 1cm in diameter. Neoplasia. Abnormal tissue growth, either benign (localized, non-invasive and non-spreading) or malignant (progressive growth with the potential for distant spread). Nodule. A palpable solid area measuring more than 1cm. Papilloma. A benign neoplastic tag or wart-like projection of the skin or mucous membrane. Papule. A solid elevation less than 1cm in diameter. Plaque. A solid elevation of the skin, greater than 1cm in diameter. Pustule. A pus-filled elevation less than 1cm in diameter. Scale. Readily detached fragments of shed keratin layer. Tumor strictly refers only to a swelling, though is commonly used to denote a neoplasm. Ulcer. A circumscribed area of epithelial loss. In skin an ulcer extends through the epidermis into the dermis. Vesicle. Circumscribed lesion containing serous fluid (less than 0.5cm across). |
Benign Epithelial Neoplasms
These kinds of eyelid lesions are six- to eight-times more common than malignant.11 Due to the variety of tissue types contained within the eyelids, there are a multitude of possibilities. For the sake of brevity, we will discuss only some of the most common types seen in clinical practice.
Squamous papillomas, commonly referred to as “skin tags,” are flesh-colored growths consisting of squamous hyperplasia within the epithelium. They may be sessile (broad-based attachment) or pedunculated (on a stalk). Removal by simple excision may be performed for cosmesis or effects on vision. 2,5
 |
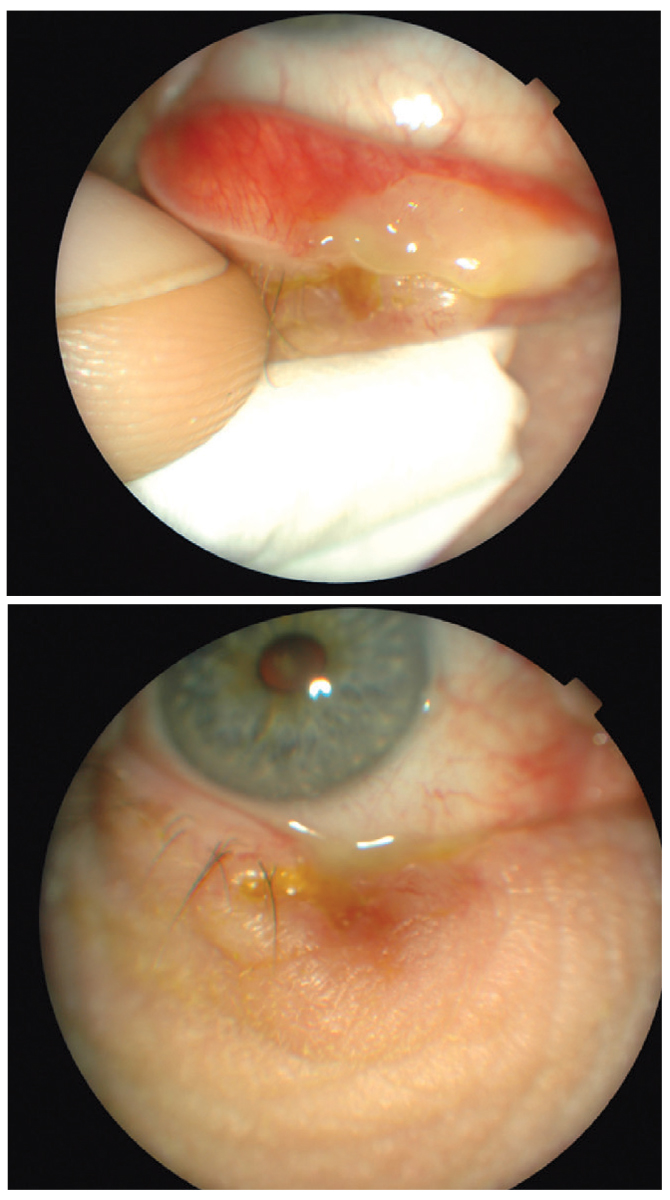
|
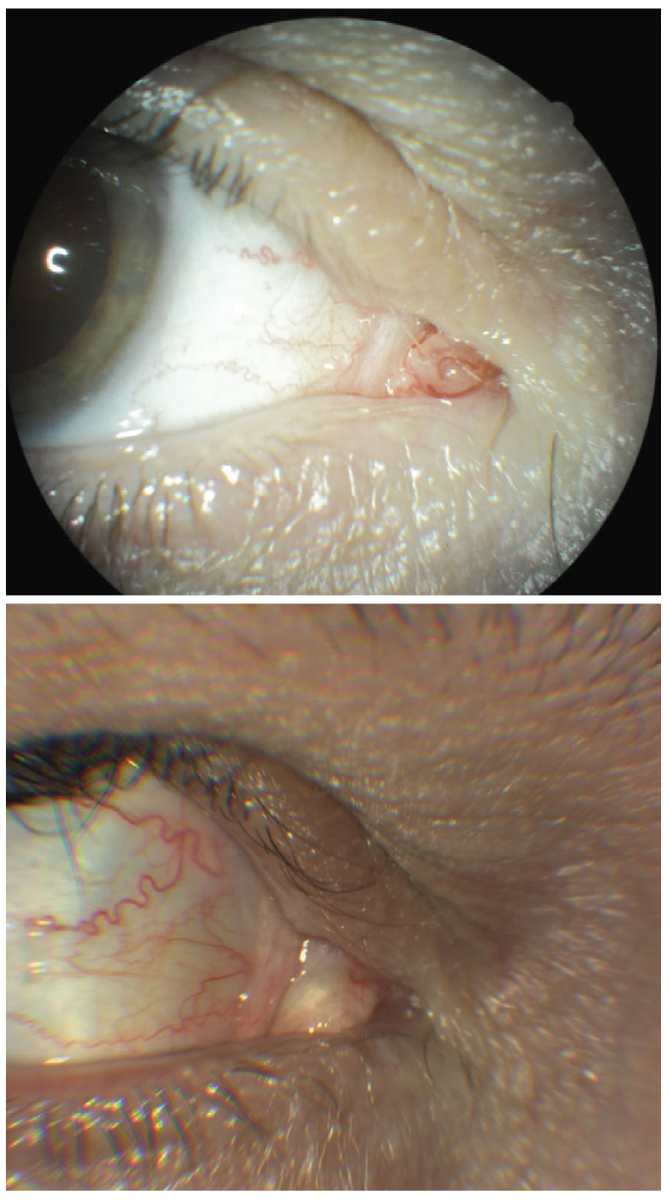
At top, mass in the caruncle right eye. Lesion was biopsied with histologic report of squamous papilloma. At bottom, 18 months post-op. Note the scar tissue. Click image to enlarge. |
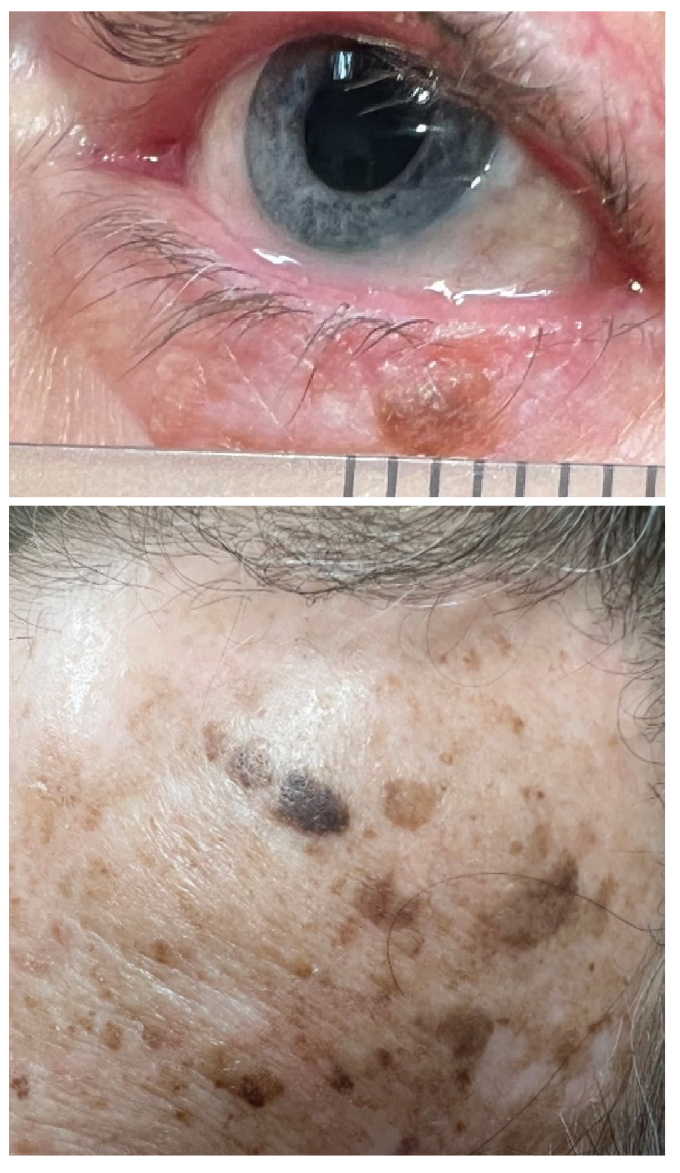
Seborrheic keratosis (SK) typically affects older individuals. These appear as elevated, pigmented, crusty, greasy, stuck-on plaques. While benign, a sudden increase in number or size could indicate a systemic malignancy. They develop from intradermal proliferation of basal cells within the epidermis. Treatment is complete excision.2, 5
Epidermal inclusion cysts are slowly enlarging keratin filled cysts. They can be removed by excision and curettage.3
Verruca vulgaris, also known as viral wart, is an epidermal growth caused by the human papilloma virus. There are two forms of verruca: ones that project in a finger-like nature from their base called filiform or digitate, and plana, which are flat in appearance. Beginning as small papules slightly lighter than the surrounding skin, they tend to darken and become hyperkeratotic with time. While benign, eyelid margin warts can cause punctate keratitis or even corneal pannus. Observation is often adequate, as these lesions tend to eventually outgrow their blood supply and spontaneously involute. Otherwise, they may be removed by excision, cryotherapy or chemical cautery if eye irritation ensues or for cosmetic reasons.12
A chalazion, which is typically secondary to an internal hordeolum, is a sterile, chronic eyelid lipogranuloma that forms after an infected meibomian gland ruptures and releases sebum into the surrounding tarsal tissue. They are associated with chronic blepharitis, meibomian gland dysfunction, seborrhea, acne rosacea and Demodex infestation of the sebaceous gland.13
Molluscum contagiosum, associated with the DNA poxvirus, is characterized by small, typically 1mm to 2mm, flesh-colored papules often with an umbilicated center. More common in the very young and in immunocompromised patients, these marginal eyelid lesions can cause follicular conjunctivitis and are spread by skin-to-skin contact. Normally they eventually regress spontaneously, except in the immunocompromised, where they can develop into disfiguring lesions. In healthy individuals, the prognosis is good, and the risk of transmission is low.13
Pyogenic granuloma presents in the form of a pinkish or red, vascularized mass that protrudes from the conjunctiva. These rapidly growing, delicate lesions are typically a response to local trauma and are composed of blood vessels and fibroblasts and readily bleed with minor insult.6
THE ABCs OF CUTANEOUS NEOPLASMSA: Asymmetry. Draw a line through the lesion. Are both sides symmetric? B: Regular borders suggest benign lesions, whereas malignant lesions tend to have irregular borders. C: Uniform color is associated with benign lesions. Color variations in a neoplasm suggest malignancy. D: Lesions larger than 6mm in diameter should raise suspicion of malignancy. E: Evolution. Changes such as rapid growth, bleeding, crusting and local tissue changes such as loss of lashes warrant biopsy. Size and depth are the two most important prognostic indicators for malignancy.10 |
Ephelides, more commonly known as freckles, are small 1mm to 3mm tan or brown macules present in sun-exposed areas of the skin. They tend to occur more frequently in individuals with light skin pigmentation and worsen with sun exposure. No treatment is necessary, but if there is a cosmetic concern, sun protection can minimize their appearance.6
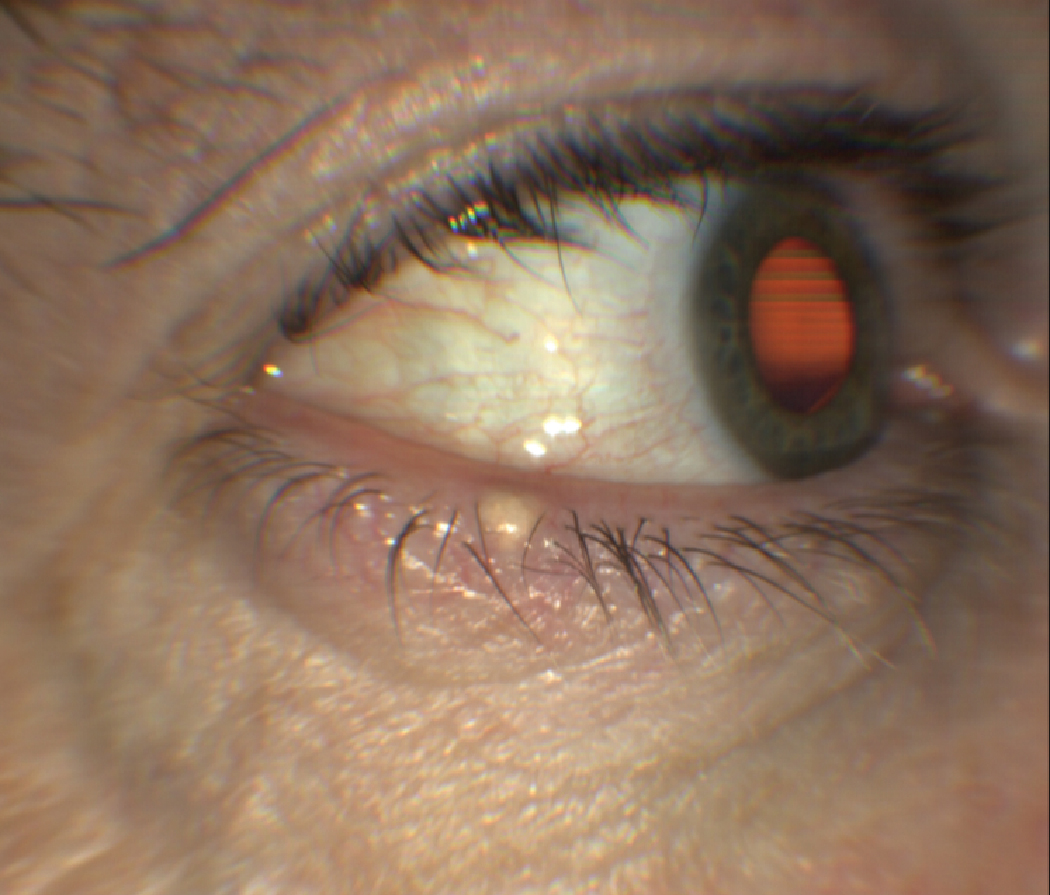
Sebaceous or pilar cysts are caused by blocked pilosebaceous follicles containing sebum. They may arise from glands of Zeis within the eyelashes, from meibomian glands or from sebaceous glands associated with hair follicles.2
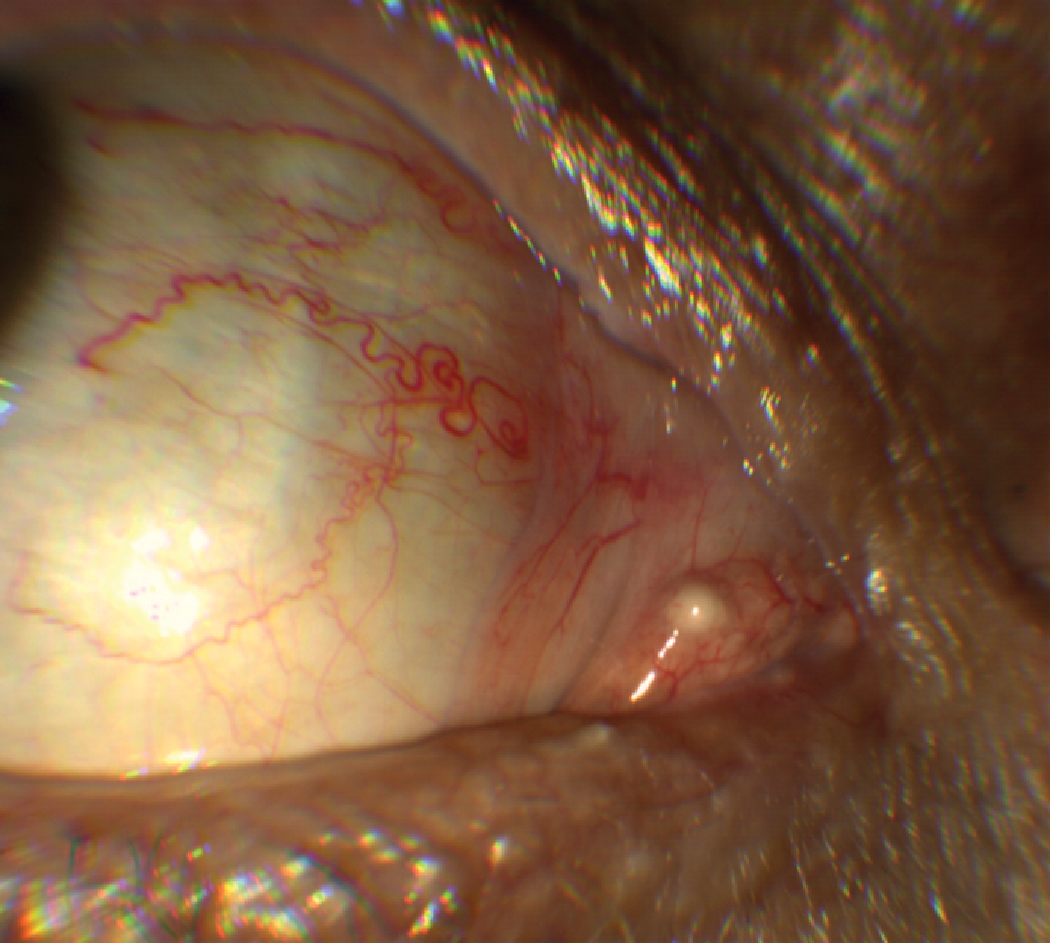
Eccrine hidrocystomas/sudoriferous cysts are small, smooth and translucent nodules on the lid skin, not involving the margin. Associated with sweat glands, these cysts often increase in size during hot and humid weather. They can be lanced and drained, but often recur unless they are excised. A similar lesion, apocrine hidrocystoma, is a translucent, milky cyst on the eyelid margin. These do not typically enlarge during hot, humid weather.2
 |
|
This lesion could be mistaken for a junctional nevus, demonstrating overlap in clinical characteristics. However, it was confirmed histologically to be an SK. At the bottom is an image of numerous SKs on the forehead of the same patient. Click image to enlarge. |
 |
|
A case of a sebaceous cyst on the right caruncle of this 67-year-old Caucasian male. Although rare, they may occasionally occur on the inner canthus including the caruncle and within thin (vellus) eyebrow hairs over the periocular skin.2 Click image to enlarge. |
Premalignant Epithelial Neoplasms
These are precancerous lesions according to histologic findings.
Actinic keratosis (AK), also known as solar keratosis, is a pink or red, scaly lesion common on sun-exposed areas of the skin such as the face, scalp, and hands. It can sometimes occur on the eyelid.3 Some 25% of cases develop into squamous cell carcinoma.9
Keratoacanthomas appear as rapidly growing papules with a central keratin-filled core in elderly or immunocompromised individuals. They can resolve over several months. Complete excision is recommended due to an approximately 12% risk of conversion to squamous cell carcinoma.3
Lentigos are caused by a proliferation of melanocytes (as opposed to ephelides, which are caused by an increase in melanin production by a stable number of melanocytes). Lentigo maligna, a precancerous lesion, should be differentiated from solar lentigo, in that the former has more irregular borders, variations of color and notching. Excisional biopsy of lesions suspicious for maligna should be performed by an oculoplastics specialist and include 5mm wide margins as frozen sections, as 10% of melanomas of the eyelids originate from maligna.3,6
Melanocytic nevi arises in childhood from a proliferation of nevocytes within the epidermis at the junction of the epidermal-dermal border (junctional nevus). Interestingly, nevocytes are capable of producing melanin, like melanocytes. Over time, these cells migrate partially into the dermis (compound nevus) and finally reside fully within the dermis (intradermal nevus).6
 |
|
Eccrine cyst drainage. Definitive treatment is complete excision. However, we have found simple incision and drainage more tolerable for patients and also note that, though they can, they don’t often recur. If they do, a repeat drainage seems to reduce recurrence, presumably from development of scar tissue within the sac. Click image to enlarge. |
 |
|
Solar lentigos and areas of actinic keratoses. These evenly hyperpigmented macules should be differentiated from the precancerous maligna, which has variable pigmentation and even more irregular borders.6 Click image to enlarge. |
Malignant Epithelial Lesions
Although benign lesions of the lids are six- to eight-times more common than malignant ones, some 5% to 10% of all skin malignancies occur on the eyelids. This may be because the eyelid is quite thin and also one of the most sun-exposed areas of the body.15
The most common type of eyelid skin cancer—about 90% of malignancies—is basal cell carcinoma (BCC). These originate in the basal layer of the epidermis and usually affect older, fair-skinned individuals with a history of chronic sun exposure. BCC demonstrates an affinity for the lower eyelid (50% to 60%) and medial canthus (25% to 30%) and manifests a low likelihood of systemic spread (less than 1% incidence of metastasis). However, local invasion can occur, and those located near the medial canthus can spread via anatomic fissures into the orbit and sinuses, making management more difficult.
 |
|
This pigmented lesion was reportedly unchanged since childhood. Note the functioning meibomian glands, normal lashes and general lack of dysplasia. We opted to photograph and monitor this and the associated small ephelides on this patient’s lower eyelid. Click image to enlarge. |
Forms include nodular, nodulo-ulcerative and sclerosing. Despite these varying appearances, BCC typically presents in its classic form as a firm, pearl papule with superficial telangiectasia at the early stage. In later stages, it may present with central ulceration and necrosis. Complete excision is recommended, with clear sections, in order to prevent recurrence, which is often aggressive.2,9
Squamous cell carcinoma (SCC) is less common, accounting for 5% to 10% of malignant eyelid neoplasms. However, it tends to be more aggressive, with spread to local lymph nodes in approximately 20% of cases. SCC can also spread along nerves into the orbit and even intracranially. It is a malignancy of the stratus spinosum layer of the epidermis and rarely contains superficial telangiectasia. Like BCC, SCC occurs in older individuals with a history of chronic sun exposure. Types include nodular, ulcerating and cutaneous horn. SCC classically presents as a rough, scaly and/or ulcerated erythematous plaque. It may be flat or elevated and is most commonly located on the lower eyelid margin.2,9
Sebaceous gland carcinoma (SGC) is a rare and slow-growing tumor with a predilection for the upper eyelid. It typically affects elderly females, and may also be associated with previous radiation therapy. Originating from meibomian glands or glands of Zeis, the classic presentation is a yellow, firm mass in the upper eyelid, often with associated madarosis and tylosis. These tumors can be mistaken for internal hordeola in their early stages, thus recalcitrant or recurrent cases should rouse suspicion. As mentioned previously, SGC are associated with poor prognosis with an overall mortality rate of 5% to 10%, but lesions greater than 2cm are associated with a 60% mortality rate. Symptomatic lesions present for longer than six months are associated with a 38% mortality rate.2,9
 |
|
This patient presented for an eye infection. Reportedly the mass had been growing for over a year, but he and his family had not addressed it due to his poor health. The patient was commencing hospice for a terminal condition (not cancer related) and the patient, wife and their daughter refused any services specific to the tumor, requesting only antibiotics for the associated blepharoconjunctivitis. Click image to enlarge. |
Melanomas are rare, accounting for only 1% of eyelid malignancies, yet are highly aggressive and potentially lethal. Despite their relative paucity, cutaneous melanoma accounts for two-thirds of all skin cancer-related deaths.6 They develop secondary to dysplasia of melanocytes in the epidermis.9 Though an image of a pigmented lesion comes to mind when thinking of these lesions, about 50% are initially non-pigmented. By the time the patient presents to clinic, they usually have irregular borders, uneven pigmentation and a history of rapid growth. Wide-margin excision, with inclusion of regional lymph nodes, is effective in localized forms. For those with significant metastasis, survival rates are poor.2
Excisional Biopsy Protocols
Lesions with a high degree of symmetry, regular borders, even pigmentation, no disruption in normal lid anatomy and lack of ulceration, are more likely benign and can be considered for in-office excision. We recommend that a representative sample of all lesions excised be sent to the lab for pathological confirmation.
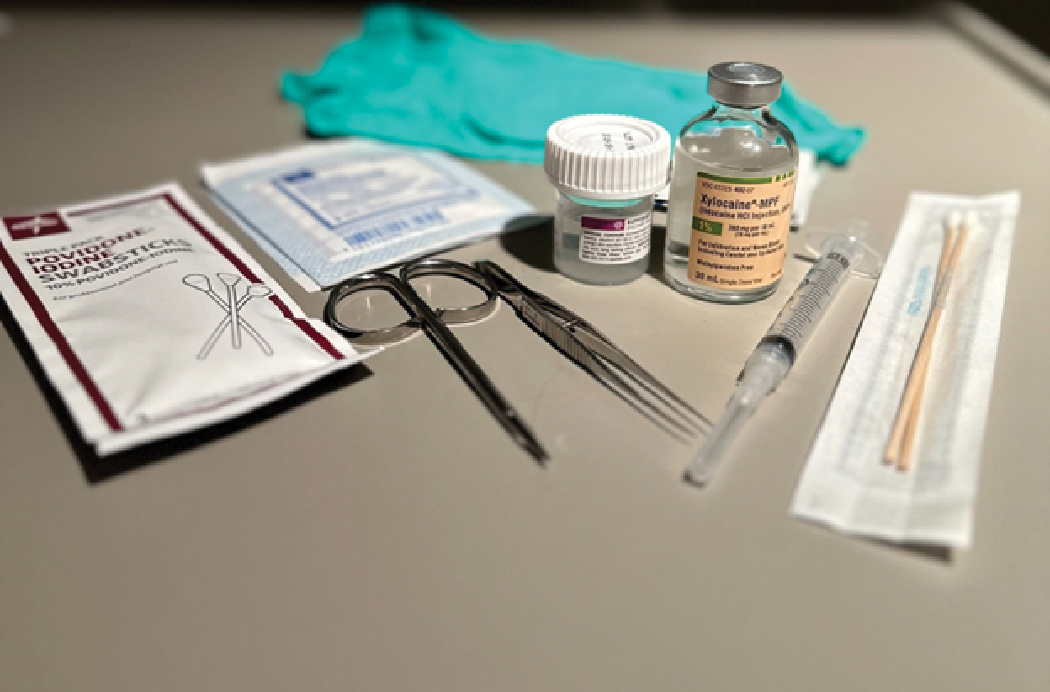
Before performing any surgical procedure, be sure to review drug allergies, discuss the risks, benefits and alternatives with the patient, and obtain informed consent with appropriate signature(s). If infiltrative anesthesia is required, inform the patient of a brief pinching sensation followed by mild burning associated with the injection. For appropriate infection control, wear sterile latex or nitrile gloves and proper eye protection. Position the patient comfortably for the procedure. You may need to recline the patient to a secure supine position to allow for easy access to the lesion. In a case such as this, where the procedure is not performed behind the slit lamp, magnifying loops can be helpful.
TREATMENT FOR EYELID LESIONS
|
 |
|
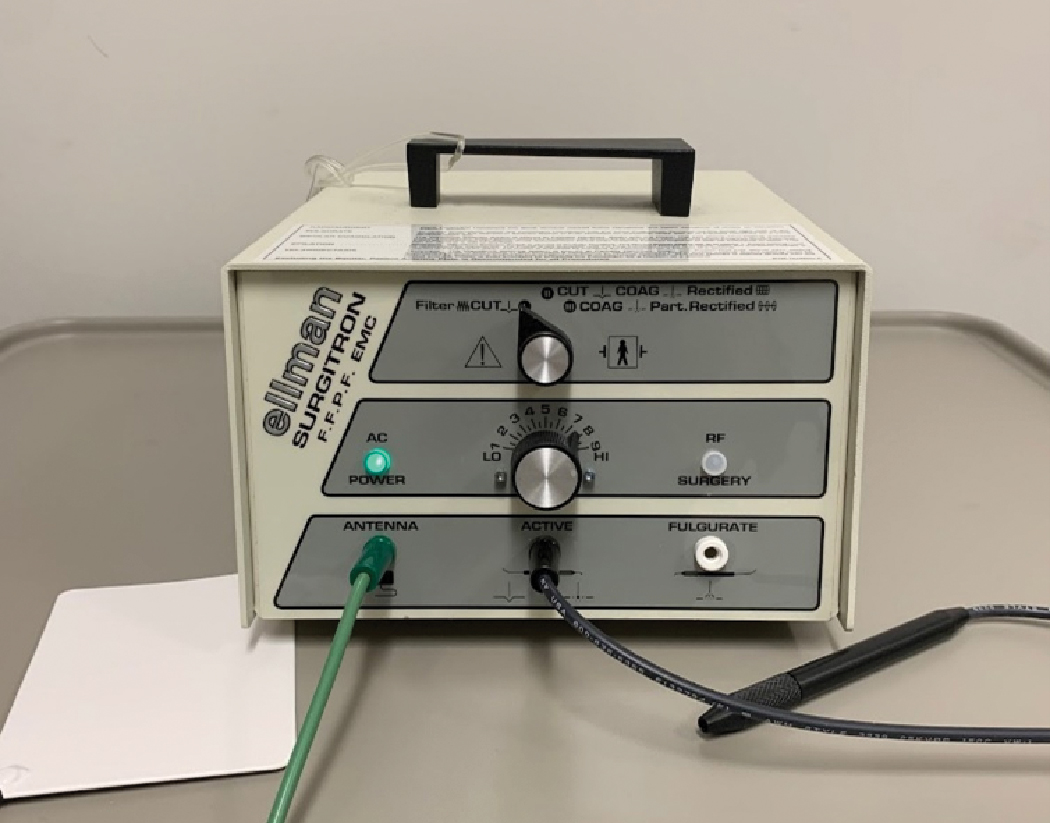
Example of a radiofrequency device in our office. Click image to enlarge. |
Consideration of the lesion base with underlying skin will determine the type of excisional technique you should use. Pedunculated lesions with smaller diameter stalks (usually 1mm to 2mm) or slightly larger can simply be removed by simple excision, often without the use of anesthetic. Larger diameter or flat-based lesions tend to require anesthesia for pain control. First, prep the area with ophthalmic Betadine. Next, inject 1% to 2% lidocaine with epinephrine 1:100,000 subcutaneously using a 27- or 30-gauge, 1/2- to 5/8-inch needle attached to a 3mL syringe. Remember to check blood pressure and pulse prior to injecting any preparation containing epinephrine. We tend to use a “bevel-down” technique for eyelid anesthesia to avoid penetrating too deeply. To ensure you’ve adequately infiltrated the tissue, you may need to retract the needle partially while still within the lesion, then orient in a different direction to inject additional anesthetic, noting slight elevation of the tissue all around the base of the lesion. Always remember when performing injections that you should pull back on the plunger before pushing it down to ensure you don’t get a flash of blood, suggestive that you’ve entered a blood vessel.
 |
|
The above lesion remained after antibiotic treatment for blepharitis. The report from an oculoplastics ophthalmologist describes an inflamed SK and treated by kenalog injection. Click image to enlarge. |
Check that the area is numb by pinching the base of the mass with your toothed forceps. Pull the lesion slightly upward away from the base placing tension on the base of the lesion and underlying skin. Position the curved-tipped scissors parallel to the skin surface, tips away from the patient, straddle the base of the stalk and snip the lesion at the junction of the base and skin surface. If minor bleeding occurs, apply firm and direct pressure with a sterile gauze pad or cotton-tipped applicator.
For significant or persistent bleeding, consider using thermal cautery. Place the excised lesion in the formalin container suitable for transport to the laboratory for histologic evaluation. Prior to releasing the patient, apply a broad-spectrum ophthalmic antibiotic ointment to the epithelial defect. Advise the patient to keep the area clean and dry and instruct the patient to apply the ointment three times daily for a few days post-procedure. We recommend non-aspirin oral analgesics for patients with any residual discomfort or irritation.
We prefer to refer lesions with malignant characteristics or those involving the lid margin to an oculoplastics ophthalmologist for evaluation, biopsy and reconstruction if needed. Alternatives to excision include epidermal curettage, chemical removal with dichloroacetic acid, chemotherapy, radiation or photodynamic therapy, as well as cryogenic therapy such as Mohs micrographic surgery.12
 |
|
Some examples of surgical equipment useful for in-office lesion removals. Click image to enlarge. |
Case #1
A 67-year-old Caucasian male farmer was referred for a recurrent stye of the right eye. He had received a prescription from his primary care physician for a topical antibiotic cream twice in the past two years for the same lesion, which he reported as a scab which eventually fell off and left a “raw” spot on his eyelid that never resolved.
We noted a lesion with raised borders, central ulceration and telangiectatic vessels. When we everted the lower lid, there was apparent dysplasia of the palpebral conjunctiva. Notably, he had a personal history of two skin cancer removals and carcinoma in situ of the anus. The patient was tentatively diagnosed with malignant neoplasm of the right lower lid and referred to a local oculoplastics ophthalmologist for biopsy.
 |
|
Case 1, recurrent hordeolum removal. Click image to enlarge. |
The patient underwent excisional biopsy with Mohs procedure and was diagnosed with infiltrative basal cell carcinoma, which involved much of the lower right eyelid and punctum. He underwent reconstruction using a rotational flap from the upper right lid and reconstruction of his lower punctum and canaliculus using a silicone tube. At follow-up, the patient verbalized that he was quite pleased with the outcome. We continued to follow the patient until his death in 2021, with no evidence of recurrence.
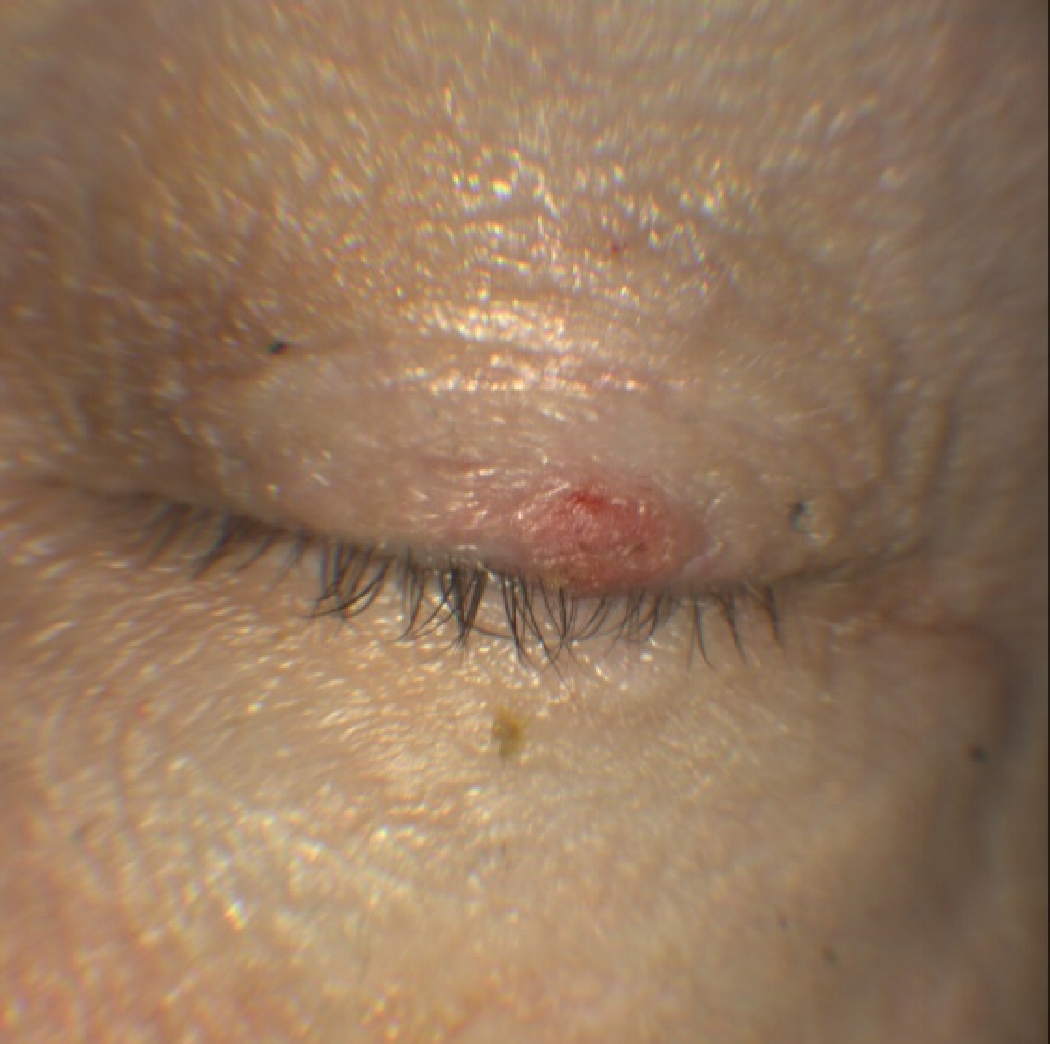
Case #2
A 70-year-old healthy white male presented with a recurrent mass on his left upper eyelid, which he had removed himself using toenail clippers over a decade prior. The lesion had since slowly regrown, absent bleeding, pain, or change in color. After obtaining informed consent, the base of the lesion was anesthetized, and the lesion was removed by simple excision. The histologic pathology report diagnosed verruca vulgaris. Four-week follow-up reveals healing scar tissue at the site of the lesion.
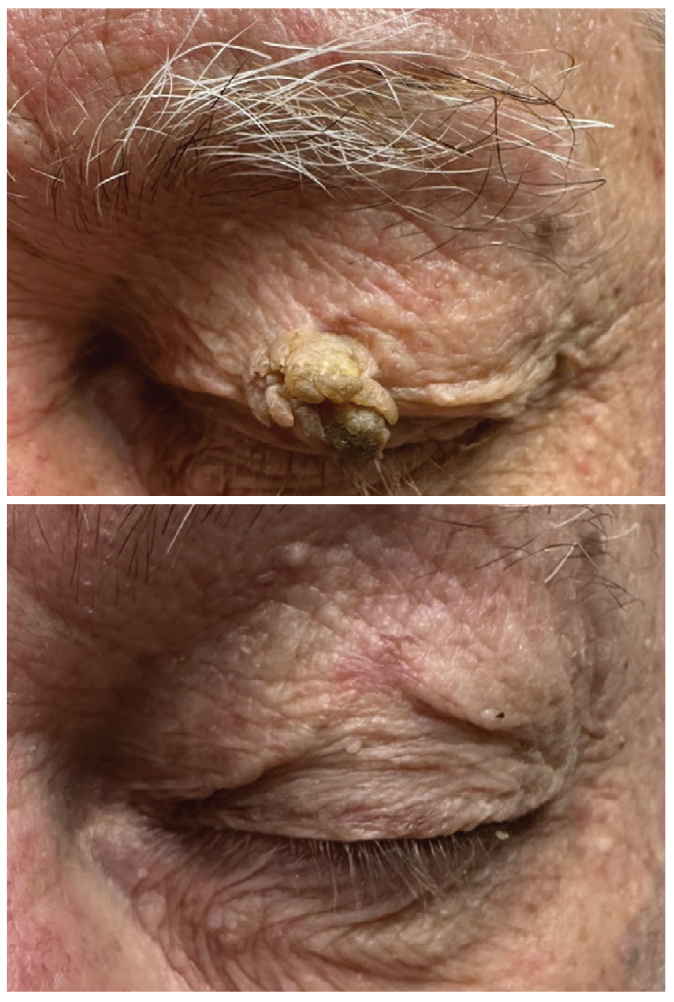 |
|
Case 2, recurrent verruca. Click image to enlarge. |
Case #3
A 76-year-old Caucasian male presented with a complaint of a cyst of the lower left eyelid, reporting it had been stable for several years. This eccrine cyst was drained in-office with a sterile 32-gauge needle and cotton-tip applicator behind the slit lamp.
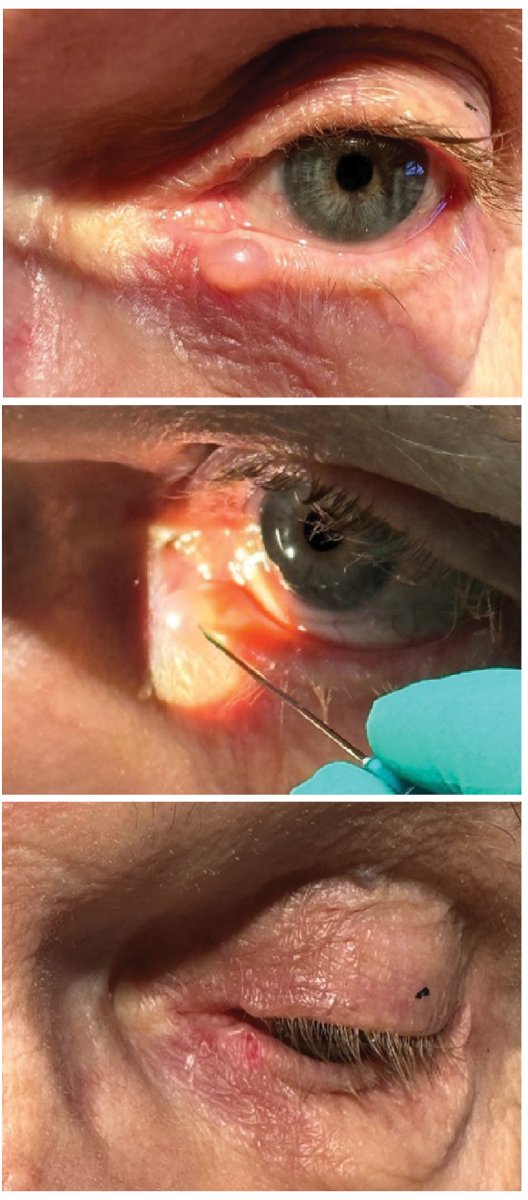 |
|
Case 3, eccrine cyst drainage.Click image to enlarge. |
Case #4
A 78-year-old Caucasian male presented for a general exam with a secondary complaint of a small “bump” under his left eye. It had been stable for one to two years, no rapid growth, bleeding, changes in color or pain. Inspection in the slit lamp revealed a small lesion with mildly elevated rim tissue and an umbilicated center. The veteran requested to have it removed.
We were able to efficiently express the entire contents. In this case, we did not send the expressed material to the lab for confirmation, but for a recurrent case, we would. We ensured complete resolution had occurred at a follow-up two weeks later.
 |
|
Case 4, mildly elevated lesion. Click image to enlarge. |
What about when you just aren’t sure? We’ve all been there: a patient presents with lackluster history skills and a lesion about which you are on the fence. Is it infectious, inflammatory, benign or malignant?
In cases such as this, when the patient can’t give a clear answer as to onset, associated symptoms, duration or evolution, we often opt to photograph, treat with the appropriate antibiotic and have the patient back in a number of weeks to determine if any changes have taken place. Note, it is best to use a ruler to document size.
Takeaways
On any given day, the optometrist will encounter a variety of eyelid lumps and bumps. While most of these are benign and carry only a cosmetic concern, some will present with malignant characteristics. Whether you intend to include surgical procedures in your repertoire, mastering the diagnosis and management of eyelid lesions is one way to achieve the superior level of care our patients expect and deserve.
Dr. Bendure is a staff optometrist and externship coordinator at Ernest Childers VA Outpatient Clinic in Tulsa, OK. He is a fellow of the American Academy of Optometry. Dr. Mai is a staff optometrist and residency supervisor at Ernest Childers VA Outpatient Clinic in Tulsa, OK. He completed his ocular disease residency at Jack C. Montgomery VA Medical Center in Muskogee, OK, and is a fellow of the American Academy of Optometry. They serve as adjunct faculty at Northeastern State University Oklahoma College of Optometry, Arizona College of Optometry and Chicago College of Optometry. They have no financial disclosures.
1. Schneider J, Scheibling C. Optometry’s essential and expanding role in health care: assured quality and greater access for healthier communities. Avalon Health Economics. www.aoa.org/AOA/Documents/Advocacy/state/Optometry%27s%20Essential%20and%20Expanding%20Role%20in%20Health%20Care-Final%20Report%20%28002%29.pdf. June 12, 2019. Accessed July 23, 2023. 2. Salmon JF. Kanski’s Clinical Ophthalmology: A Systematic Approach. 9th ed. Edinburgh: Elsevier; 2020. 3. Onofrey BE, Skorin L, Holdeman NR. Ocular Therapeutics Handbook a clinical manual. Wolters Kluwer; 2020. 4. Remington LA. Clinical Anatomy and Physiology of the Visual System. St. Louis, Missouri Butterworth-Heinemann; 2012. 5. Gawkrodger DJ, Ardern-Jones MR. Dermatology: An Illustrated Color Text. 7th ed. Elsevier; 2021. 6. Yanoff M, Duker JS. Ophthalmology. 6th ed. Elsevier; 2022. 7. Kersten RC, Ewing-Chow D, Kulwin DR, Gallon M. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology. 1997;104(3):479-84. 8. Margo CE. Eyelid tumors: accuracy of clinical diagnosis. Am J Ophthalmol. 1999;128(5):635-6. 9. Friedman NJ, Kaiser PK, Pineda R. The Massachusetts Eye and Ear Infirmary. 4th ed. Elsevier; 2014. 10. Fitzpatrick TB, Johnson R, Wolff K, Suurmond R. Color Atlas and Synopsis of Clinical Dermatology. 4th ed. McGraw-Hill, St. Louis, 2001. 11. Deprez M, Uffer S. Clinicopathological features of eyelid skin tumors. a retrospective study of 5,504 cases and review of literature. Am J Dermatopathol. 2009;31(3):256-62. 12. Casser L, Fingeret M, Woodcome H, et al. Atlas of Primary Eyecare Procedures. 2nd ed. Appleton & Lange; 1997. 13. Penne R. Oculoplastics. 2nd ed. Wolters Kluwer Health/Lippincott Williams & Wilkins Health; 2012. 14. Bolognia JL, Shaffer JV, Duncan KO, Ko CJ. Dermatology Essentials. Elsevier, 2022. 15. Cook BE Jr, Bartley GB. Epidemiologic characteristics and clinical course of patients with malignant eyelid tumors in an incidence cohort in Olmsted County, Minnesota. Ophthalmology. 1999;106(4):746-50. 16. Landow, SM, Oh DH, Weinstock MA. Teledermatology within the Veterans Health Administration, 2002-2014. Telemed J E Health. 2015 ;21(10):769-73. |

