 |
Dr. Gurwood thanks Nick Karbach, OD, for his contributions to this case.
A 47-year-old female presented to the office emergently with a chief complaint of right-side facial pain of two weeks’ duration. She explained she was diagnosed with a sinus infection by her medical doctor and started on an oral antibiotic but was not improving. She had no previous medical or ocular history. She was taking only the oral antibiotic prescribed by the doctor and denied allergies of any kind.
Clinical Findings
Her best-corrected entering visual acuities were 20/20 OD and 20/20 OS at distance and near. Her extraocular motilities were normal and her confrontation fields were full OU. The pertinent external and pupillary observations are demonstrated in the photographs below.
There was no afferent defect present. Her biomicroscopic examination was normal and Goldmann applanation tonometry was measured at 17mm Hg in both eyes. Dilated fundus examination revealed no significant posterior pole or peripheral retina findings: the nerves were distinct with cup-to-disc ratios of 0.3/0.35 OD and OS.
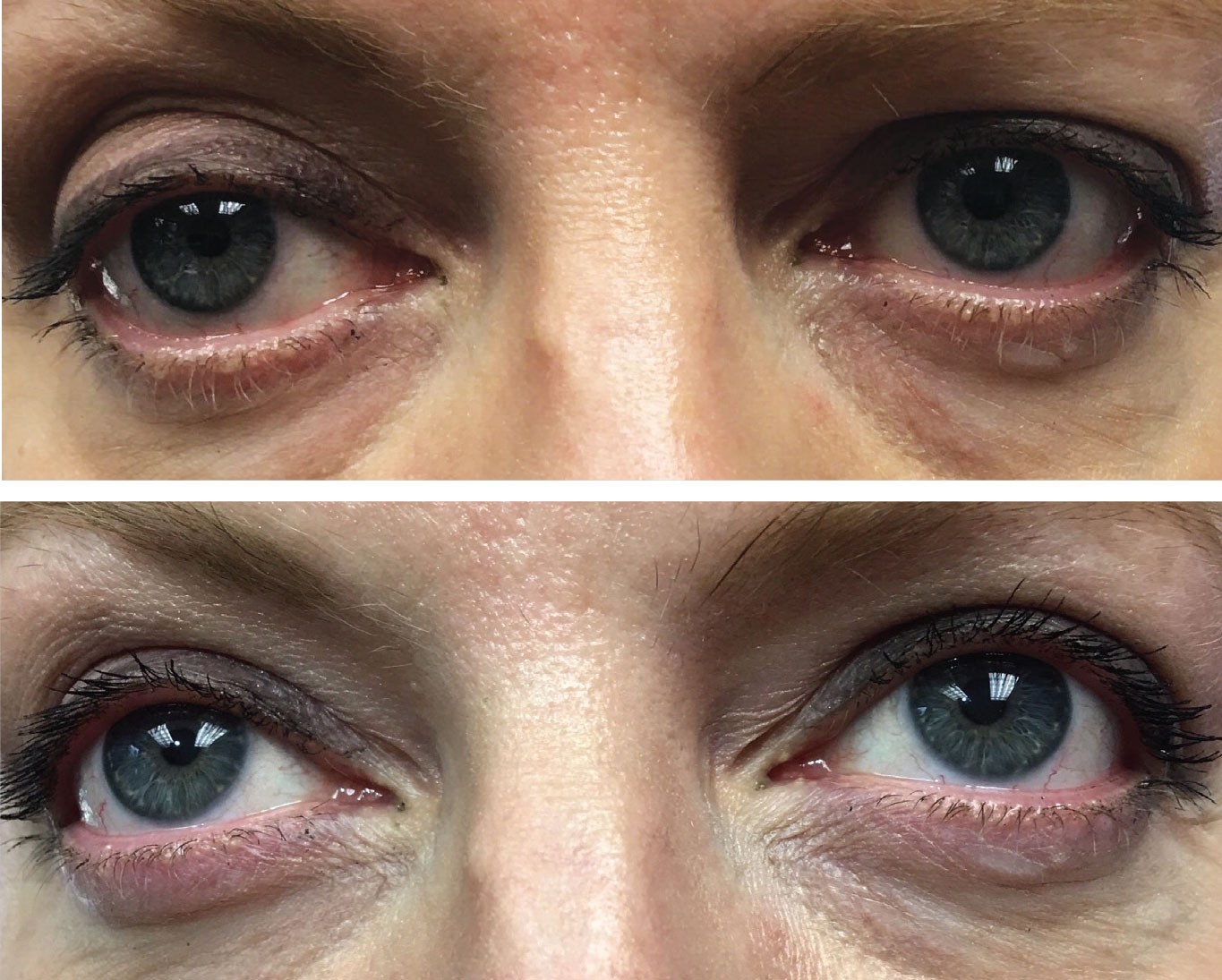 |
How might this presentation connect with the symptom of facial pain on the right side? Click image to enlarge. |
For More Information
Additional studies included measuring the pupils in both bright and dim illumination to confirm a pathologic anisocoria. Inspecting old photographs was completed to ensure that the ptotic eyelid position on the suspected side was new. A diluted topical adrenergic drop instillation test was completed to provoke suspected denervation hypersensitivity on the suspected side and observe its effect on the ptotic eyelid.
What would be your diagnosis in this case? What is the patient’s likely prognosis?
Tracing Neuro-Ophthalmic Pathways
The diagnosis in this issue is Horner’s syndrome due to acute carotid artery dissection. Horner’s syndrome is characterized by an interruption of the oculosympathetic nerve supply somewhere between its origin in the hypothalamus and the eye.1-9 The classic clinical findings associated with Horner’s are ptosis, pupillary miosis, facial anhidrosis, apparent enophthalmos, increased amplitude of accommodation, heterochromia of the irides (if before age two or congenital), paradoxical contralateral eyelid retraction, transient decrease in intraocular pressure and changes in tear viscosity.1-9
Horner’s syndrome has no predilection for age, race, gender or geographic location. When it’s of congenital origin, it presents around the age of two years with heterochromia and absence of a horizontal eyelid fold or crease in the ptotic eye.1-5,9 Iris pigmentation (which is under sympathetic control during development) is completed by the age of two, making heterochromia an uncommon finding in Horner’s syndrome acquired later in life.1-3 Old photographs can aide the clinician in distinguishing congenital Horner’s by documenting heterochromia present at birth.1-5
Sympathetic innervation to the eye consists of a three-neuron arc.1-9 The first originates in the dorsolateral hypothalamus. It descends through the reticular formation of the brainstem and travels to the ciliospinal center of Budge between the levels of the eighth cervical and fourth thoracic vertebrae (C8-T4) of the spinal cord. There, it synapses with second-order neurons whose preganglionic cell bodies give rise to axons, which exit the white rami communicants of the spinal cord via the anterior horn. These axons pass over the apex of the lung and enter the sympathetic chain in the neck, synapsing in the superior cervical ganglion.1-9 Here, cell bodies of third-order neurons give rise to postganglionic axons that course to the eye with the internal carotid artery via the cavernous sinus.1-9
Fibers from these axons form the long and short posterior ciliary nerves of the eye. These sympathetic nerve fibers course anteriorly through the uveal tract and join the fibers of long posterior ciliary nerves (branches of the fifth cranial nerve) to innervate the dilator of the iris. Postganglionic sympathetic fibers also innervate the muscle of Mueller, which is responsible for the initiation of eyelid retraction during eyelid opening. Postganglionic sympathetic fibers are also responsible for initiating facial sweating. They follow the external carotid artery to the sweat glands of the face.1-9 Interruption along this pathway, at any location (preganglionic or postganglionic), will induce an ipsilateral Horner’s syndrome.
Making the Call
The diagnosis and the localization of a Horner’s syndrome can be accomplished with pharmacological testing.5-9 Topically applied 10% cocaine works as an indirect acting sympathomimetic agent producing pupillary dilation in the normally innervated pupil by inhibiting the re-uptake of norepinephrine at the nerve ending in the synaptic cleft.4-9 A Horner’s pupil will dilate poorly compared to the normal eye because the interruption of the pathway has created a relative absence of norepinephrine at the nerve ending.4-9 The test should be evaluated 30 minutes after the instillation of the drops to ensure accuracy. The cocaine test is used to confirm or deny the presence of a Horner’s syndrome. A positive cocaine test does not localize the lesion.1-9 Another method used relies on denervation hypersensitivity; adrenergic receptors becoming hypersensitive to adrenergic neurotransmitter secondary to its absence. Here, dilute phenylephrine, apraclonidine or brimonidine may dilate a Horner’s pupil and effectively decrease a Horner’s ptosis.1-19
To localize the lesion as either preganglionic (neurons 1 or 2 before the synapse in the superior cervical ganglion) or postganglionic (after exiting the superior cervical ganglion), Paradrine (hydroxyamphetamine 1%) or Pholedrine (n-methyl derivative of hydroxyamphetamine 5%) can be instilled 48 hours later. Pholedrine and Paradrine act similarly by producing a forced release of endogenous norepinephrine from the presynaptic vesicles. If the third neuron is damaged, the pupil will not dilate, indicating a postganglionic lesion.1-9 There is currently no method of topical testing to differentiate a first-order preganglionic lesion from a second-order one.7
The common etiologies of acquired Horner’s syndrome include but are not limited to trauma, aortic dissection, carotid dissection, tuberculosis and Pancoast tumor.1-9
Aortic dissections often occur along the right lateral wall of the ascending aorta, where the hydraulic stress is the greatest.1-11 Compression of adjacent tissues (e.g., superior cervical ganglia, superior vena cava, bronchus, esophagus) by the expanding dissection, can result in Horner’s syndrome, superior vena cava syndrome, vocal cord paralysis, hoarseness, dysapnea, dysphagia, facial pain, ear pain and neck pain with up to 16% presenting with other associated cranial nerve palsies.11 Patients with long-standing systemic hypertension, Marfan’s syndrome and Ehlers Danlos syndrome are at increased risk.1–9 The issue is also a known complication of sports-related and ancillary traumas.12,13
In all cases the resultant hematoma in the arterial wall impacts adjacent tissues producing, among other things, oculosympathetic paresis.14 In cases where direct (a blow/blunt trauma) or indirect trauma (a deceleration injury) are absent the pathogenesis remains unknown.14 Predisposing factors seem to exist. Recognizing the signs and symptoms of Horner’s syndrome is important so that devastating neurological sequelae like embolic strokes, aneurysmal rupture and death can be avaoided.15 Frequently, physicians who fail to inspect the eyes or don’t identify the miotic pupil and ptotic lid misdiagnose temporal mandibular jaw (TMJ) dysfunction, otitis externa (swimmers ear), tooth cavity or sinusitis, prolonging the work up and testing necessary to make the correct diagnosis.1-15
Neck and facial pain (often misdiagnosed as sinusitis), headache, unilateral pulsatile tinnitus, amaurosis fugax and retinal infarction are all signs and symptoms that can accompany the partial oculosympathetic palsy.16,17 Timely neuroimaging is pivotal in making the right diagnosis. Clinical vigilance is of utmost importance as early diagnosis and prompt treatment favor a good long-term prognosis by arresting and preventing additional ischemic complications.16,17
Systemic Connections
Raeder first described Horner’s syndrome with ipsilateral head pain due to paratrigeminal organic disease.18 Today, Raeder’s syndrome is defined by facial pain with ipsilateral stenosis of the palpebral fissure, miosis and enophthalmos.19 It is divided into two groups. Group I includes cases with parasellar cranial nerve involvement and group II without parasellar cranial nerve involvement. Group II Raeder’s syndrome is difficult to distinguish from Horner's syndrome.19 In fact Raeder’s syndrome may be caused by any lesion affecting the post-ganglionic oculosympathetic fibers distal to the bifurcation of the common carotid artery. Serious lesions of the internal carotid artery (ICA) maybe responsible for this syndrome.19
Tuberculosis (TB) is a chronic infectious disease caused by the organism Mycobacterium tuberculosis.1-9 TB is an airborne disease that is transmitted from person to person by the inhalation of infected air droplets. TB may infect any organ in the body; however, the lungs are the most prevalent site of involvement.8,9 Tubercles (from which the name of the disease is derived) are granulomatous inflammations that invade the lung and induce tissue necrosis referred to as caseations.9 If the tubercle occupies a position at the lung apex, it may compress preganglionic sympathetic axons, producing a Horner’s syndrome.9 Diagnosis can be made with a purified protein derivative (PPD) accompanied with an anergy panel.9 A chest x-ray and erythrocyte sedimentation are also helpful in confirming the diagnosis.9
Pancoast tumor or superior pulmonary sulcus carcinoma was first described in 1924 by H.K. Pancoast.10 Clinical characteristics of Pancoast tumor include shoulder pain, loss of limb function, atrophy of the muscles of the hand, Horner’s syndrome and dullness of feeling in the region of the upper chest.10 A true Pancoast tumor usually extends through the visceral pleura into the parietal pleura and chest wall. The tumor is considered to be epithelial in its histopathology but its exact origin remains uncertain. Despite its small size and general lack of metastasis, Pancoast tumor has a rapid and almost universal mortality rate. Approximately 80% to 90% of all lung cancers are linked or associated with smoking.10 Other risk factors include exposure to asbestos, radon gas, uranium, arsenic fumes, isopropyl oil, nickel, metallic iron, iron oxide and beryllium.10
Management Approach
In general, the treatment for Horner’s syndrome depends upon the cause. In many cases there is no treatment that improves or reverses the condition. Treatment in acquired cases is directed toward eradicating the disease that is producing the syndrome. Recognizing the signs and symptoms is tantamount to early diagnosis and expedient referrals to specialists.
The timeframe for testing is important because cocaine has the ability to inhibit the uptake of Pholedrine and Paradrine into the presynaptic vesicle, reducing accuracy.5-9 Some of the older literature suggests employing phenylephrine 1% solution for localization.
This patient was referred to neuro-ophthalmology, where appropriate topical testing confirmed the presence of Horner’s syndrome. Neuroimaging was ordered, uncovering a carotid artery dissection for which oral anticoagulation therapy with clopidogrel and aspirin was ordered. The patient recovered well over three months.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Wilkins, RH, Brody, IA, Durham, NC. Horner’s syndrome. Arch Neurol 1968;19(5):540-542. 2. Horner, F. Uber eine form von ptosis. Klin Monatsbl Augenh 1869;7(1):193. 3. Tantum, LA. Pupil anomalies. In: Onofrey BE, ed. Clinical optometric pharmacology and therapeutics. Philadelphia, PA.; J.B. Lippincott Co. 1991;13:1-13. 4. Burde, RM, Savino, RJ, Trobe, JD. Anisocoria and abnormal pupillary light reaction. In: Burde, RM, Savino, PJ, Trobe, JD, eds. Clinical decisions in neuro-ophthalmology, 2nd ed. St. Louis, MO.; Mosby Year Book Inc. 1992:321-346. 5. Myles, WM, Maxner, CE. Localizing value of concurrent sixth nerve paresis and postganglionic horners’s syndrome. Can J Ophthalmol 1994;29 91 0:39-42. 6. Maloney, WF, Younge, BR, Moyer, NJ. Evaluation of the causes and accuracy of pharmacologic localization in horner’s syndrome. Am J Ophthalmol 1980;90:394-402. 7. Bates, AT, Chamberlain, S, Champion, M, et al. Pholedrine–a substitute for hydroxyamphetamine as a diagnosis eye drop test in Horner’s syndrome. J Neurology, Neurosugery, and Psychiatry 1995;58:215-217. 8. Thompson, HS, Pilley, SFJ. Unequal pupils- a flow chart for sorting out the anisocorias. Survey Ophthalmol 1976;21(1):45-48. 9. Cullom, RD, Chang, B. Neuro-ophthalmology : Horner’s Syndrome. In: Cullom, RD, Chang, B, eds. The Wills Eye Manual, 2nd ed. Philadelphia, PA.; J.B. Lippincott Co. 1993: 241-246. 10. Sartori, F, Rea, F, Calabro, F, et al. Carcinoma of the superior pulmonary sulcus. J ThoracCardiovasc Surg 1992;104:679-683. 11. Majeed A, Ribeiro NP, Ali A, et al. A rare presentation of spontaneous internal carotid artery dissection with Horner's syndrome, VIIth, Xth and XIIth nerve palsies. 12. Alonso Formento JE, Fernández Reyes JL, Envid Lázaro BM, et al. Horner's syndrome due to a spontaneous internal carotid artery dissection after deep sea scuba diving. Case Rep Neurol Med. 2016;2016:5162869. 13. Macdonald DJ, McKillop EC. Carotid artery dissection after treadmill running. Br J Sports Med. 2006;40(4):e10; discussion e10. 14. Verdin V, Holemans C, Otto B, et al. Horner's syndrome revealing a spontaneous carotid artery dissection. Rev Med Liege. 2013;68(1):11-5. 15. Shankar Kikkeri N, Nagarajan E, Sakuru RC, Bollu PC. Horner Syndrome Due to Spontaneous Internal Carotid Artery Dissection. Cureus. 2018;10(9):e3382. 16. Chan CC, Paine M, O'Day J. Carotid dissection: a common cause of Horner's syndrome. Clin Exp Ophthalmol. 2001;29(6):411-5. 17. Schelfaut D, Dhondt E, De Raedt S, et al. Carotid artery dissection: three cases and a review of the literature. Eur J Emerg Med. 2012;19(3):181-7. 18. Solomon S, Lustig JP. Benign Raeder's syndrome is probably a manifestation of carotid artery disease. Cephalalgia. 2001;21(1):1-11. 19. Zournas C, Kapaki E, Doris S, et al. Raeder's syndrome. Report of two cases. Int Angiol. 1995;14(4):415-7. |

