 |
Cerebrovascular accident (CVA), or stroke, is a medical emergency that occurs as a result of ischemia or hemorrhage leading to abnormal perfusion of brain tissue. The initial symptoms of stroke may include sudden loss of speech, dizziness, confusion, weakness or paralysis of one side of the body, headache and seizure. Because ocular manifestations may be the presenting signs of stroke, the optometrist’s role in the stroke patient’s care is rapidly expanding.
Symptoms and Signs
Common visual symptoms of stroke include blur, visual field loss and diplopia. A patient experiencing a transient ischemic attack (TIA) may report amaurosis fugax, or a fleeting (usually monocular) blindness that occurs rapidly and resolves in a few minutes. Symptoms of bilateral transient vision loss may result from vertebrobasilar insufficiency. Patients who suffer a TIA are at risk for a major CVA shortly thereafter.1
Retinal emboli may precede cerebral stroke and are associated with an increased incidence of vascular disease and stroke-related death.2 Other common ocular manifestations include cranial nerve involvement and homonymous field loss.
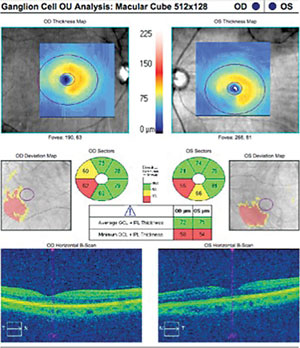 | |
| Fig. 1. SD-OCT ganglion cell analysis in a patient with corresponding homonymous field defects following a stroke. Note GCC thinning inferotemporal to the foveal center OD and inferonasal OS, shown as areas within the blue squares on the deviation maps. |
Prompt Action
Prompt diagnosis and treatment of stroke and TIA are crucial, as early action can minimize brain damage and potential complications. A patient may come to you with some of the symptoms and signs listed above, thinking it is only an eye issue. It is important for the clinician to think beyond the eye in such cases. If you observe signs that indicate a patient is having, or about to have, a stroke, immediately call 9-1-1 so that medical personnel can begin life-saving treatment on the way to the emergency room.
Ideally, a multidisciplinary health care team will evaluate the stroke patient. Neuroimaging plays a vital role in the workup of acute stroke by providing information essential to accurately triage patients, expedite clinical decision-making with regards to treatment and improve outcomes (Table 1). If the patient suffered an ischemic stroke, the team may administer a thrombolytic drug, such as tissue plasminogen activator (tPA).3 In hemorrhagic stroke, medications, surgery or endovascular procedures may be necessary to stop the bleeding and save brain tissue.4
Assessing the Damage
Axonal degeneration is a phenomenon that occurs when a nerve fiber loses function after an injury or other traumatic event, such as CVA. This process begins at the anatomic site of the damage and can happen in an anterograde fashion (toward the post-synaptic end) or in a retrograde fashion (toward the presynaptic cell body). When the degeneration crosses a synapse, it is referred to as trans-synaptic.5
In stroke patients, recent research shows that thinning of the retinal ganglion cell complex (GCC), as seen on optical coherence tomography (OCT), can help practitioners detect retrograde degeneration.5 Evidence of retrograde trans-synaptic degeneration exists in patients with homonymous hemianopsias from occipital ischemia. This relationship is reflected in thinning of the GCC and maintains the topographic relationship of the visual field defect (Figure 1).
Rehab and Neuroplasticity
Stroke affects the brain’s information processing, and the effect on a patient’s visual function is variable, often depending on the location and extent of the insult. Visual changes associated with stroke can be categorized as sensory (visual acuity and visual field), motor (extraocular muscle motility) and perceptual.6
| Table 1. Neuroimaging for Stroke1 The neuroradiology team will select from among various studies: Computed Tomography (CT): Advantages include widespread access and speed of acquisition. In hyperacute phases, a non-contrast CT scan is usually ordered to exclude or confirm hemorrhage. Magnetic Resonance Imaging (MRI): Provides excellent soft tissue contrast. Fluid attenuated inversion recovery (FLAIR) images provide detection of acute subarachnoid hemorrhage. Magnetic resonance angiography (MRA) can be performed in combination with MRI to help guide therapeutic decision-making. MRI can detect atherosclerotic lesions in the neck and head. Nuclear Imaging: Functional imaging with positron emission tomography (PET) and single photon emission computed tomography (SPECT) might reveal carotid plaque vulnerability for rupture and help in evaluating brain viability. Ultrasonography: Carotid Doppler for the diagnosis of carotid stenosis. Cerebral Angiography: Imaging of vascular diseases of the brain and great vessels of the neck. 1. Xavier AR, Qureshi AI, Kirmani JF, et al. Neuroimaging of stroke: a review. Southern Medical Journal. 2003;96(4):367-79. |
The term neuroplasticity refers to the brain’s ability to structurally alter itself and create new axonal connections in response to changing internal and external conditions. Neuroplasticity occurs in the brain under two main conditions:
- During normal brain development when the immature brain first begins to process sensory information through adulthood.
- As an adaptive mechanism to compensate for lost function or to maximize remaining function in the event of brain injury or stroke.7
The goal of vision rehabilitation in post-CVA patients is to maximize visual function for various activities of daily living. The cognitive and psychological status of the patient are assessed and integrated into the rehabilitation program. Optometric physicians skilled in vision rehabilitation are an important part of the multidisciplinary stroke rehabilitation team.
Stroke is the fifth leading cause of death in the United States and results in a drastic reduction in quality of life.8 Optometrists are integral to the care team, helping stroke patients manage the ocular effects and maintain quality of life.
1. Purvin V. Cerebrovascular disease and the visual system. Ophthalmol Clin N Am. 2004;17:329-55.2. Wong TY, Klein R. Retinal arteriolar emboli: epidemiology and risk of stroke. Curr Opin Ophthalmol. 2002 Jun;13(3):142-6.
3. Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better stroke outcome: the NINDS rt-PA stroke study. Neurology. 2000;55:1649-55.
4. American Heart Association/American Stroke Association. Stroke Treatments. 2013.
5. Herro AM, Lam BL. Retrograde degeneration of retinal ganglion cells in homonymous hemianopsia. Clinical Ophthalmology (Auckland, NZ). 2015;9:1057-64.
6. Khan S, Leung E, Jay WM. Stroke and visual rehabilitation. Top Stroke Rehabil. 2008 Jan-Feb;15(1):27-36.
7. Bowdena MG, Woodbury ML, Duncan PW. Promoting neuroplasticity and recovery after stroke. Curr Opin Neurol. 2013;26(1):37-42.
8. Centers for Disease Control and Prevention. Stroke. www.cdc.gov/stroke/.
Stroke Q & A
Dr. Bansal is an assistant professor at Nova Southeastern University, and specializes in neuro-optometric rehabilitation. |

