A 50- year-old white male presented for an exam with no subjective complaints. His medical history was remarkable for hypertension, a cerebrovascular accident (CVA), transient ischemic attacks (TIAs), hyperlipidemia, bilateral carotid artery disease, vertebrobasilar artery disease and a five-year history of diabetes. He also reported undergoing a rare surgical procedure to correct vessel blockage on the left side of his head two years prior.
The patients ocular history was remarkable for complete vision loss in the left eye, laser surgery in the left eye and a retrobulbar alcohol block to relieve pain in the left eye. He said that his left eye was relatively comfortable and that he only experienced intermittent pain.
Diagnostic Data
Best-corrected visual acuity was 20/20 O.D. and no light perception O.S. His pupils were round and reactive O.D. but fixed and dilated O.S.; there was a reverse afferent pupillary defect O.S. No muscle restrictions were noted in either eye, and confrontation visual fields were full in the right eye.
Intraocular pressure measured 12mm Hg O.D. and 24mm Hg O.S. Gonioscopy revealed an open anterior chamber angle with ciliary body visible in all quadrants of the right eye. There were no visible angle structures in the left.
Anterior segment findings were unremarkable in the right eye, but diffuse iris rubeosis was present in the left. Dilated fundus examination revealed a healthy, well-perfused optic nerve O.D. There were hemorrhages in all quadrants that extended into the periphery (figure 1). No neovascularization of the disc or elsewhere was noted. Macular hemorrhages were present without clinically significant macular edema.
The left optic nerve revealed 3+ disc pallor, attenuated vessels and poor vascular architecture within the posterior pole. Scattered hemorrhages were also present in the left eye, although not to the extent of the right, and a tight pattern of panretinal laser photocoagulation scars was noted 360 degrees in the periphery (figure 2).
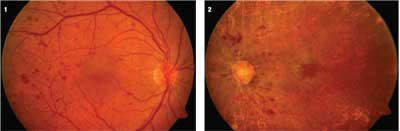 | |
| 1. Hypoperfusion retinopathy O.D. Blot hemorrhages in all quadrants extend into the peripheral retina 360 degrees. 2. Central retinal artery occlusion O.S. secondary to embolus during vertebral artery reconstruction and residual hemorrhaging secondary to retinal hypoperfusion. Neovascular glaucoma eventially developed, requiring extensive panretinal photocoagulation. A retrobulbar alcohol block was also required to manage pain. |
Diagnosis
We diagnosed this patient with hypoperfusion retinopathy in each eye. The left eye also had suffered a central retinal artery occlusion (CRAO) with the subsequent development of neovascular glaucoma.
Treatment and Follow-up
We reviewed the patients medical record in which a cerebral arteriogram revealed 100% occlusion of both carotid arteries and 99% occlusion of each vertebral artery. Due to the severity of his vascular status, and because of continued neurological symptoms (TIAs, knee drops and syncope), this patient had elected to undergo reconstructive grafting of the left vertebral artery.
Before the patients surgery, the records showed that the left fundus was very similar in appearance to the right, with hemorrhages extending into the periphery in all quadrants. Approximately one year after surgery, an embolus occluded the left central retinal artery which subsequently resulted in neovascular glaucoma. An alcohol block was required to manage the eye pain and, in time, the left eye had to be enucleated.
We now monitor him every four months for changes that might require further intervention. The patient recently underwent panretinal photocoagulation in the right eye because of neovascularization of the optic nerve and retina. Polycarbonate lenses were prescribed to protect his right eye.
Discussion
Hypertension and atherosclerosis represent the primary etiologies of most degenerative cerebrovascular diseases and stroke. Ischemia and infarction are the final common denominators that result in nervous tissue damage.
Risk factors for stroke vary and are classified as modifiable or non-modifiable (see Risk Factors for Stroke, below).
|
Risk Factors for Stroke1,4,12,16 |
|
Non-modifiable Factors |
| Age. Risk of stroke increases with age and doubles every 10 years after the age of 55. Rate of death following stroke increases with age. |
| Gender. Prior to age 65, men have about a 20% higher risk of stroke than women. Females tend to be older when they have their first stroke and are more likely than males to die from stroke. |
| Race. Blacks have a 60% greater risk of stroke than whites. They also tend to have greater disability after stroke and are twice as likely to die from a stroke. |
| Family history. Risk of stroke increases if a first-degree relative (e.g., parent, sibling, son or daughter) has had a stroke. Inherited deficits in clotting and metabolism increase the risk of stroke. |
|
Modifiable Factors |
| Hypertension. This is the most important modifiable risk factor. Some 90% of all patients who are normotensive at age 55 are eventually diagnosed with hypertension. For elderly patients, reductions of 11.4mm Hg in mean systolic blood pressure and 3.4mm Hg in diastolic blood pressure reduce the risk of stroke by 36%. Also, successful long-term treatment of hypertension can reduce the risk of stroke by at least 33%. |
| Smoking. Risk of stroke is dose-dependent, increasing with the number of cigarettes smoked per day. After smoking cessation, the risk of stroke decreases within two to five years. |
| Carotid stenosis. Carotid artery disease is responsible for 20% to 30% of strokes annually. Annual stroke rate for asymptomatic hemodynamically significant stenosis is 2%. Carotid endarerectomy for asymptomatic carotid artery stenosis (with more than than 60% occlusion) reduces the five-year risk of ipsilateral stroke from 11% to 5.1%. |
| Atrial fibrillation. The most frequent cardiac risk factor for stroke, it affects 2.2 million people in the United States. Stroke rates among patients with atrial fibrillation vary from 0.5% to 12%. About 15% of ischemic strokes are attributed to atrial fibrillation, with 70% of all strokes in the 65- to 85-year-old age group attributed to this cardiopathy. |
| Physical inactivity. Increased activity (30 minutes/day of aerobic exercise) reduces the risk of stroke across all genders, races and age groups. A dose-response relationship is seen with both the duration and intensity of exercise. |
| Diabetes. The risk of stroke is two to four times greater among patients who have diabetes. |
| Hyperlipidemia. Lowering lipid levels with statin medications is associated with a reduction in the occurrence of first stroke in those who have coexisting heart disease. |
|
Prior stroke. Risk of recurrence in those who have already had a stroke is twice as high as the risk of a first stroke. One in six ischemic stroke survivors will have another stroke within two years. |
Transient ischemic attacks (TIAs), defined as transient neurological dysfunction that lasts less than 24 hours, are the most reliable indicators of impending stroke. The time from no symptoms to maximum symptoms is typically five minutes or less.
An individual who has had one or more TIAs is 10 times more likely to have a stroke than someone of the same age and gender who has not experienced a TIA.1
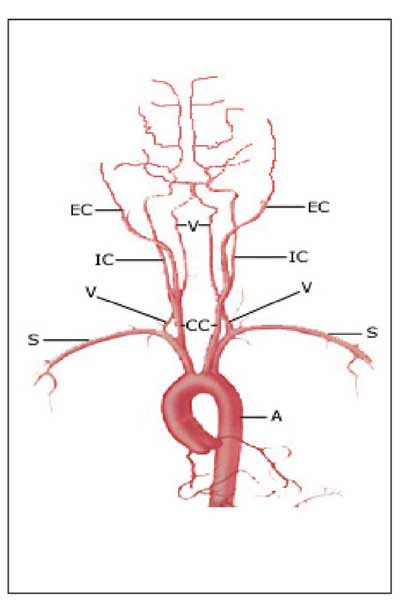 |
| 3. Origin of the major intracranial arteries from the aortic arch: aorta(A), subclavian artery (S), common carotid artery (CC), vertebral artery (V), internal carotid artery (IC) and external carotid artery (EC). |
At least one-third of those who experience these ischemic episodes go on to have a stroke. Indeed, approximately 15% to 30% of strokes that occur after the initial TIA happen during the first month, and 40% to 50% of all strokes subsequent to the initial TIA occur within the first year.1 But, recent research shows that the risk of stroke occurring seven days, 30 days and one year after the initial TIA may be higher than commonly quoted.2,3 For patients who survive the first year after the TIA free of stroke, the annual risk of a subsequent stroke is approximately 4% (see Warning Signs of Stroke, below).4
|
Warning Signs of Stroke |
| Sudden numbness or weakness of the face, arm or leg, on one side of the body. |
| Sudden confusion or difficulty speaking or understanding. |
|
Sudden loss of vision in one or both eyes. |
|
Dizziness, sudden trouble with walking, loss of balance or coordination. |
|
Sudden severe headache of unknown origin. |
Hemodynamic symptoms (TIAs, weakness, dizziness, etc.) associated with vertebral artery disease occur secondary to either emboli or vessel stenosis. The most common etiology of vertebral artery disease is atherosclerosis. Current estimates suggest that up to one-third of vertebrobasilar ischemic episodes are caused by emboli from plaques formed in the subclavian, vertebral, and/or basilar arteries.5 On occasion, other less frequently encountered etiologies have been identified (see Etiologies of Vertebrobasilar Artery Disease, below).
For hemodynamic symptoms to manifest, both vertebral arteries and the compensatory vascular supply from the anterior circulation via the circle of Willis (also called cerebral arterial circle) must be significantly compromised. Generally, more than 75% stenosis of both vertebral arteries is required before disease symptoms appear.5
| Etiologies Of Vertebrobasilar Artery Disease 5,6,7,8 |
| Aneurysms |
| Atherosclerosis |
| Dissections |
| Embolism |
| Fibromuscular dysplasia |
|
Hypertension |
|
Osteophyte compression |
|
Takayasu disease (inflammation of the aorta and its major branches) |
Changes in posture or position, cardiac insufficiency, and significant stenosis of the proximal subclavian artery causing subclavian-vertebral steal syndrome (brainstem ischemia aggravated by arm exercise) can also induce transient ischemic attacks.
Medical conditions that can mimic and confound the diagnosis of vertebrobasilar ischemia include bilateral internal carotid artery disease, inappropriate use of anti-hypertensive medications, anemia, brain tumors, benign vertiginous states, basilar artery migraine, inner ear pathology and post-subarachnoid hemorrhage and vasospasm.5-8
The most common symptoms associated with vertebrobasilar disease include dizziness, vertigo and nausea. These symptoms reflect a compromise of structures related to the vestibular apparatus, which is located throughout much of the brainstem. Accurate diagnosis of vertebrobasilar territory disease, however, requires the presence of additional symptoms besides dizziness and nausea. (See Common Neurological Symptoms of Vertebrobasilar Artery Disease, below.)
| Common Neurological Symptoms Of Vertebrobasilar Artery Disease 1,5 |
| Alternating paresthesias |
| Ataxia (failure of muscle coordination) |
| Cortical blindness |
| Diplopia |
| Dizziness |
| Dysarthria (speech disturbance) |
| Dysphasia (difficulty swallowing) |
| Headaches |
| Knee drops |
| Nausea/vomiting |
|
Nystagmus |
|
Perioral numbness |
|
Photopsia |
|
Sensory loss |
|
Tinnitus |
|
Transient ischemic attack |
|
Vertigo |
|
Visual field loss |
While manifestations of carotid artery disease are typically unilateral, signs and symptoms suggestive of vertebrobasilar disease are generally bilateral with poorly defined neurological manifestations. The basilar artery is a single midline vessel with branches supplying both sides of the brainstem, so motor and sensory defects can be unilateral, bilateral or alternating. (see Anatomy of Blood Flow to the Brain, below.)
 |
| 4. Major arterial supply to the brain: anterior cerebral artery (ACA), middle cerebral artery (MCA)and posterior cerebral artery (PCA). |
Transient, bilateral vision loss, lasting seconds to minutes, is the most commonly reported ocular symptom. These episodes of ischemia are more varied than those that occur in patients who have carotid artery disease. Other visual sequelae reported in patients who have vertebrobasilar territory disease include diplopia, photopsias, cranial nerve palsies and visual field defects.
|
Anatomy of Blood Flow to the Brain |
| Arterial blood flow to the brain is derived from the paired carotid and vertebral arteries. Each minute, approximately 700ml of blood flows to the brain through the carotid arteries and their branches, whereas about 200ml of blood flows via the vertebrobasilar system. The carotid arteries supply the anterior two-thirds of the cerebral hemispheres, including the deep white matter and the basal ganglia.
The vertebrobasilar system is part of the posterior circulation, which consists of the two vertebral arteries and the basilar artery. The vertebrobasilar supply perfuses the remaining posterior and medial portions of the cerebral hemispheres, thalamic region, brainstem, cerebellum and cervical spinal cord. The carotid and vertebrobasilar systems interconnect with their counterparts in the opposite hemisphere via the circle of Willis. The anterior and posterior cerebral circulations originate at the aortic arch. The first branch off the arch is the brachiocephalic (innominate) artery. This trunk gives rise to the right common carotid artery, the right vertebral artery and the right subclavian artery. The second branch off the aortic arch is the left common carotid artery. Finally, the third branch is the left subclavian artery, from which the left vertebral artery arises (figure 3). The internal carotid artery divides to form the anterior cerebral artery (ACA) and the middle cerebral artery (MCA). The ACA is responsible for perfusion of the medial aspect of the cerebral hemisphere, and the MCA supplies the lateral aspect (figure 4). Occlusion of the ACA or one of its branches results in loss of sensation and weakness of the contralateral lower extremities, whereas occlusion of the MCA or one of its branches causes similar deficits in the contralateral upper extremities. The vertebral arteries ascend and unite at the base of the pons to form the basilar artery. Branches of the basilar artery supply the brainstem and cerebellum. The basilar artery bifurcates near the base of the midbrain to form paired posterior cerebral arteries (PCA) that branch to supply the occipital lobes and feed into the circle of Willis. Occlusion of any of these vessels most often results in symptoms of dizziness, vertigo and nausea. |
When patients experience symptoms that are suggestive of vertebrobasilar disease, evaluation may include:
Transcranial Doppler imaging. Doppler imaging of the posterior circulation is possible but difficult, with examination of the entire basilar artery being possible in only 30% of patients. Sensitivity and specificity of transcranial Doppler imaging of the vertebrobasilar system is at best 87% and 80%, respectively.9
Magnetic resonance angiography (MRA). MRA now allows for three-dimensional imaging of posterior circulation territories.
Conventional angiography. As with carotid artery disease, an arteriogram is the diagnostic gold standard for diagnosing this particular vasculopathy.
Medical management of patients with vertebrobasilar territory disease hinges on diagnostic and laboratory findings. Although some patients are suitable candidates for surgical reconstruction, others can be managed medically with various oral therapeutic agents.
For surgical purposes, the vertebral arteries are divided into four segments. These areas represent various levels along the course of the artery that provide sites for reconstructive bypass surgery.
Complications from surgery vary and are dependent on the level of reconstruction. A combined morbidity/mortality rate of 0.9% occurs in those cases in which reconstruction occurs nearer the vertebral branch off the subclavian, the most common site of vertebral artery obstruction. Reconstruction at more distal sites carries a combined mortality/morbidity rate of 4%.
Common perioperative complications include stroke, hematoma, thrombosis, and injury to the sympathetic chain (Horners syndrome), spinal accessory nerve and vagus nerve. In the hands of an experienced surgeon, combined stroke and death rates are 4% or less, and more than 80% of patients can expect relief of symptoms after surgical bypass.5
Investigational evaluation of percutaneous balloon angioplasty and stent placement for the treatment of vertebrobasilar territory ischemia is currently being considered for those individuals who have persistent symptoms and who are poor surgical candidates.10,11
Antiplatelet drugs are typically used in an attempt to prevent secondary ischemic stroke and recurrent TIA. Aspirin is the most frequently administered medication after stroke or TIA and has been studied most extensively for its effect on reducing recurrences. Initiation of aspirin (160mg/day to 325mg/day) within 48 hours after the onset of stroke symptoms has been shown to reduce the risk of stroke recurrence and reduce the odds of nonfatal myocardial infarction and nonfatal stroke by 22%.12-14
The U.S. Food and Drug Administration has approved dosages that range from 50mg/day to 325mg/ day, and in Europe doses as low as 30mg/day have been shown to reduce stroke recurrence.15
Other antithrombotic medications include Plavix (clopidogrel, Bristol-Meyers Squibb/ Sanofi Pharmaceutical), Ticlid (ticlopidine, Roche) and Aggrenox (aspirin/extended-release dipyridamole, Boehringer Ingelheim). Of the agents available, aspirin is the most commonly used drug, and this trend will likely continue because of its convenience and cost. Ticlid has been replaced by Plavix in many instances due to the tendency of ticlopidine to induce neutropenia (decreased total white cell counts) and platelet abnormalities. After the initial ischemic event, patients are usually started on aspirin, unless there are contraindications. If symptoms continue, other antithrombotic medications can be added.
The European Stroke Prevention Study demonstrated that combination antiplatelet therapy is superior to single agent therapy in reducing the risk of stroke recurrence, with aspirin and dipyridamole combination therapy reducing the risk of recurrence by 36% vs. aspirin or dipyridamole alone at 18% and 16%, respectively.15 Warfarin has not been shown to be superior to these antiplatelet therapies in the secondary prevention of stroke except among those patients with atrial fibrillation.
Surgical reconstruction of the vertebral artery is an option available to a defined subset of patients who suffer from ischemia that occurs secondary to compromise of the vertebrobasilar distribution.
Clinically, we rarely encounter patients who have extensive, bilateral stenosis requiring such drastic intervention. However, clinicians must recognize the signs and symptoms of this vasculopathy and be aware of the medical evaluation, management and surgical options available to these patients.
Drs. Graybeal and Whitaker practice with the Tuscaloosa Veterans Affairs Medical Center, Tuscaloosa, Ala.
1. American Stroke Association. Stroke curriculum for medical students. Modules 1-6. 2000.
2. Patient notes: transient ischemic attacks. Postgrad Med. 2002 Mar;111(3):111-8.
3. Lovett JK, Dennis MS, Sandercock PA, et al. Very early risk of stroke after a first transient ischemic attack. Stroke 2003 Aug;34(8):e138-40.
4. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991 Jun 26;265(24):3255-64.
5. Eskandari M, Garcia ND. Vertebral artery atherothrombosis. Available at: www.emedicine.com/med/topic3464.htm. (Accessed October 13, 2006)
6. Berguer R, Flynn LM, Kline RA, Caplan L. Surgical reconstruction of the extracranial vertebral artery: management and outcome. J Vasc Surg 2000 Jan;31(1 Pt 1):9-18.
7. Berguer R, Morasch MD, Kline RA. A review of 100 consecutive reconstructions of the distal vertebral artery for embolic and hemodynamic disease. J Vasc Surg 1998 May;27(5):852-9.
8. Caplan L. Posterior circulation ischemia: then, now, and tomorrow. The Thomas Willis Lecture-2000. Stroke 2000 Aug;31(8):2011-23.
9. Flemming KD, Brown RD Jr. Cerebral infarction and transient ischemic attacks. Efficient evaluation is essential to beneficial intervention. Postgrad Med 2000 May 15;107(6): 55-62, 72-4, 79-80
10. Malek AM, Higashida RT, Phatouros CC, et al. Treatment of posterior circulation ischemia with extracranial percutaneous balloon angioplasty and stent placement. Stroke 1999 Oct;30(10):2073-85.
11. Chastain HD 2nd, Campbell MS, Iyer S, et al. Extracranial vertebral artery stent placement: in-hospital and follow-up results. J Neurosurg 1999 Oct;91(4):547-52.
12. Ingall TJ. Preventing ischemic stroke. Current approaches to primary and secondary prevention. Postgrad Med 2000 May 15;107(6):34-6, 39-42, 47-50.
13. Collaborative overview of randomised trials of antiplatelet therapyI: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists Collaboration. BMJ 1994 Jan 8;308(6921):81-106.
14. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet 1997 May 31;349(9065): 1569-81.
15. Diener HC, Cunha L, Forbes C, et al. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996 Nov; 143(1-2):1-13.
16. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002 Dec 18;288(23):2981-97.

