Photo Atlas of Ocular DiseaseReview of Optometry has created the following new resource—a photo atlas of ocular diseases across the entire spectrum of eye care. In addition to over 200 high-quality photos, you'll find clinical pearls for each condition and links to relevant articles that provide detailed guidance. An index of the entire atlas can be found here or you can check out the conditions featured in their respective categories: |
Alterations of the retina can be caused by a wide variety of etiologies, ranging from benign findings to sight- or life-threatening pathologies, making it extremely important to make an accurate diagnosis. When examining the retina, dilation is often crucial as it allows for evaluation of more peripheral structures and the ability to obtain a steady stereoscopic view. Multiple fundus lenses are used to view the retina, including both contact and non-contact lenses, as well as techniques such as scleral depression, use of adjunct filters and exam techniques such as the Watzke-Allen sign. It is important to use the tools necessary to properly evaluate the retina clinically as you move towards ordering additional imaging.
Multiple options now exist for imaging the retina as well, with each technology giving a unique insight into the retina’s structure. These include optical coherence tomography (OCT), OCT-angiography (OCT-A), fundus autofluorescence (FAF), fluorescein angiography (FA), indocyanine green angiography (ICGA) and multispectral imaging.
While some conditions can be accurately diagnosed and managed with fundus evaluation alone, others may be best visualized with advanced retinal imaging and some may require simultaneous use of multiple types (multimodal imaging) to arrive at an accurate diagnosis. Nevertheless, it is important to begin with a proper case history and clinical examination, first considering the patient’s complaints and demographics before moving forward with ordering retinal imaging. It is then crucial to accurately interpret the imaging obtained to arrive at a proper diagnosis.
Primary care ODs with young, healthy patients may lack routine exposure to some of the retina’s more exotic findings. The following section provides sample images of an array of retinal pathologies as they are seen both clinically and when imaging is used. It is important to keep in mind that the same condition can have a variety of presentations that may not be entirely captured by the sample image.
Feel free to click the condition that interests you to jump to it, or scroll to look through all the conditions.
Central serous chorioretinopathy
Rhegmatogenous retinal detachment
Retinal angiomatous proliferation
Central retinal vein occlusion
Central retinal artery occlusion
Branch retinal artery occlusion
Intraretinal microvascular abnormalities
Nonproliferative diabetic retinopathy
Proliferative diabetic retinopathy
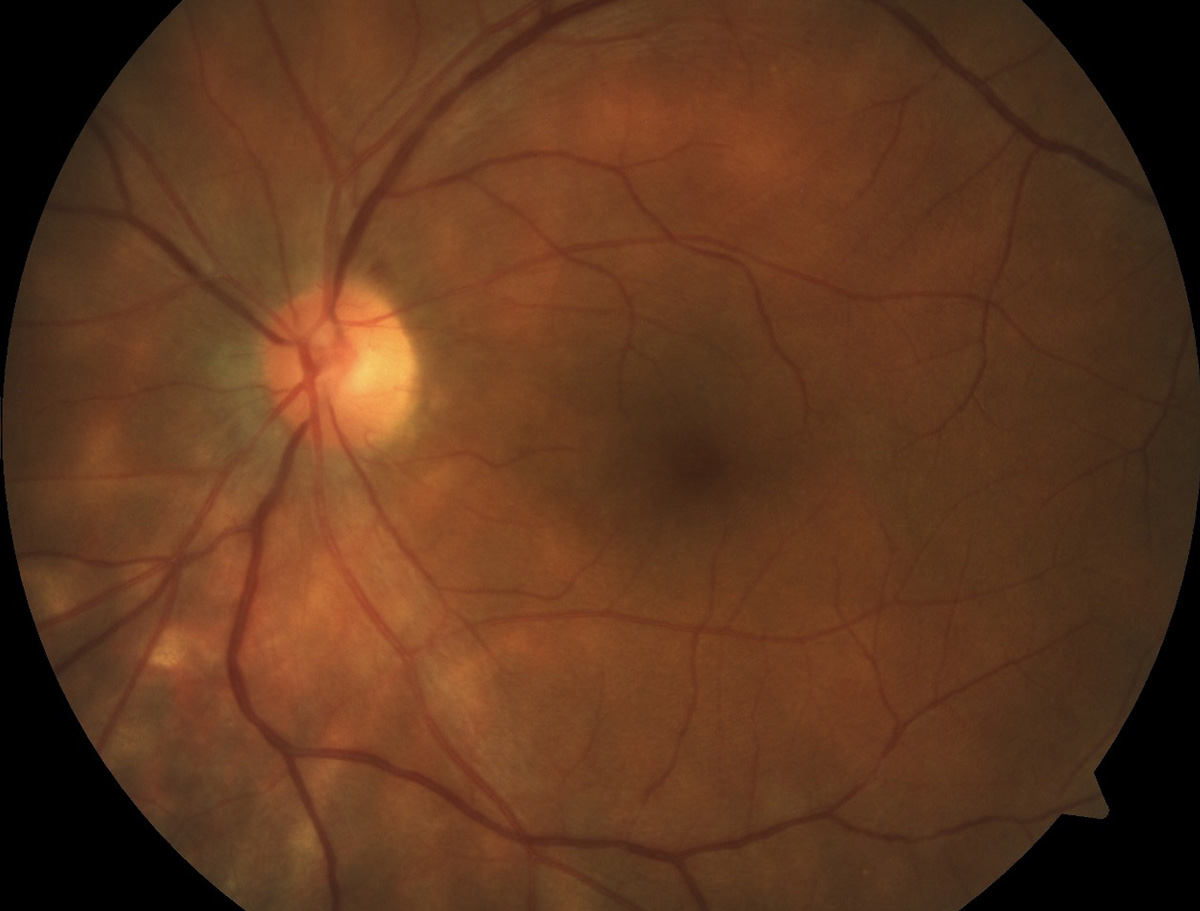
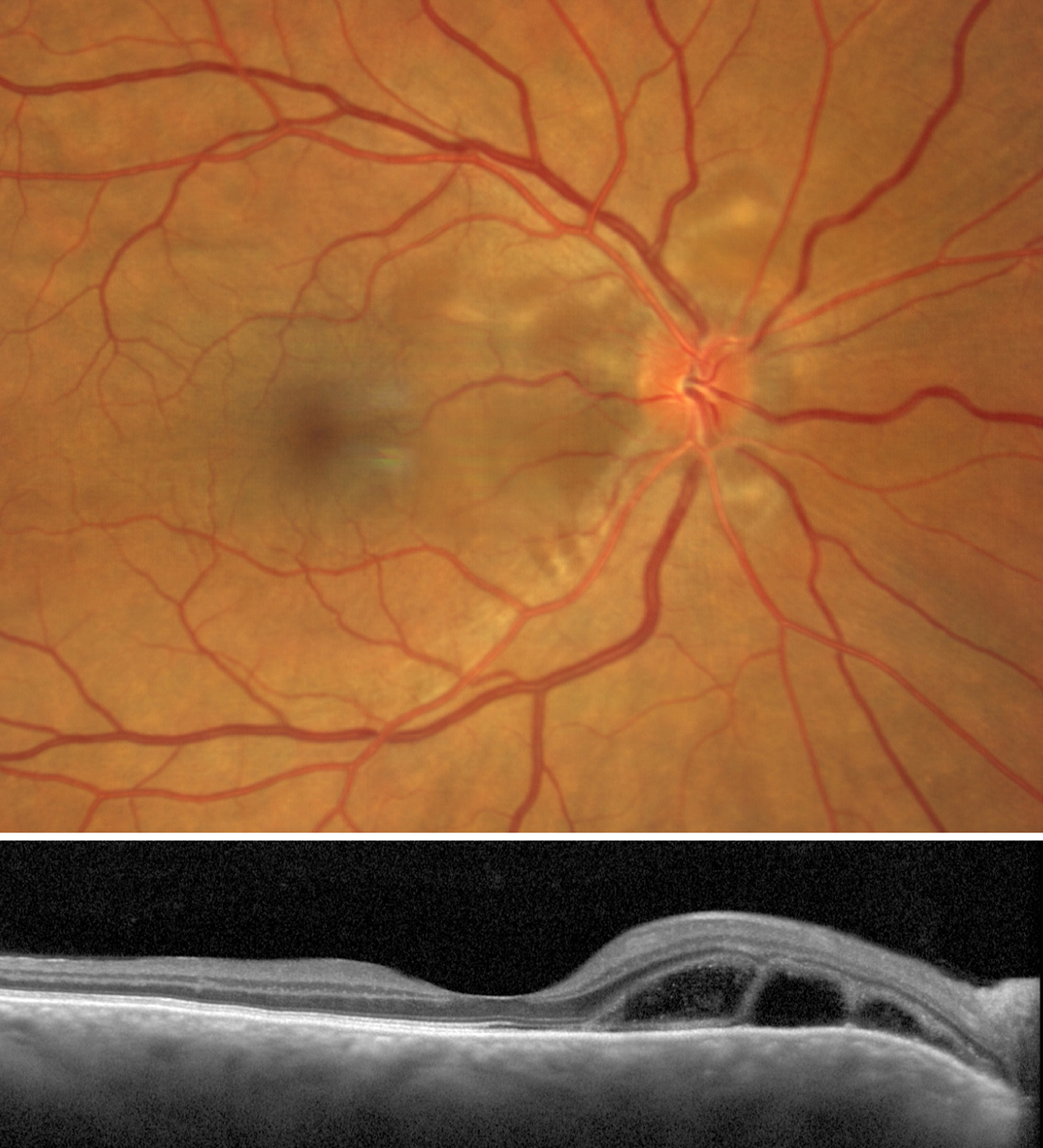
Central serous chorioretinopathy
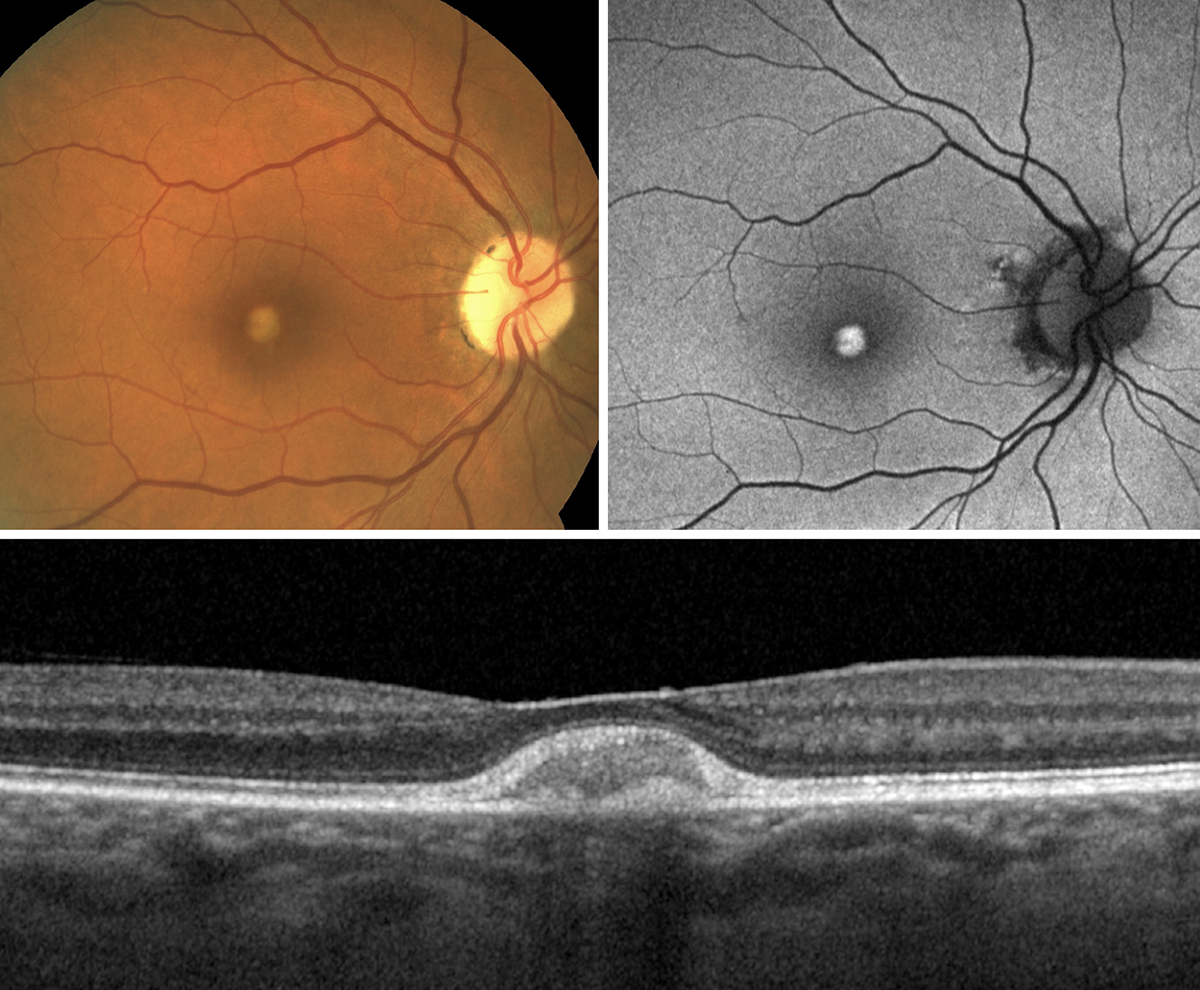
 |
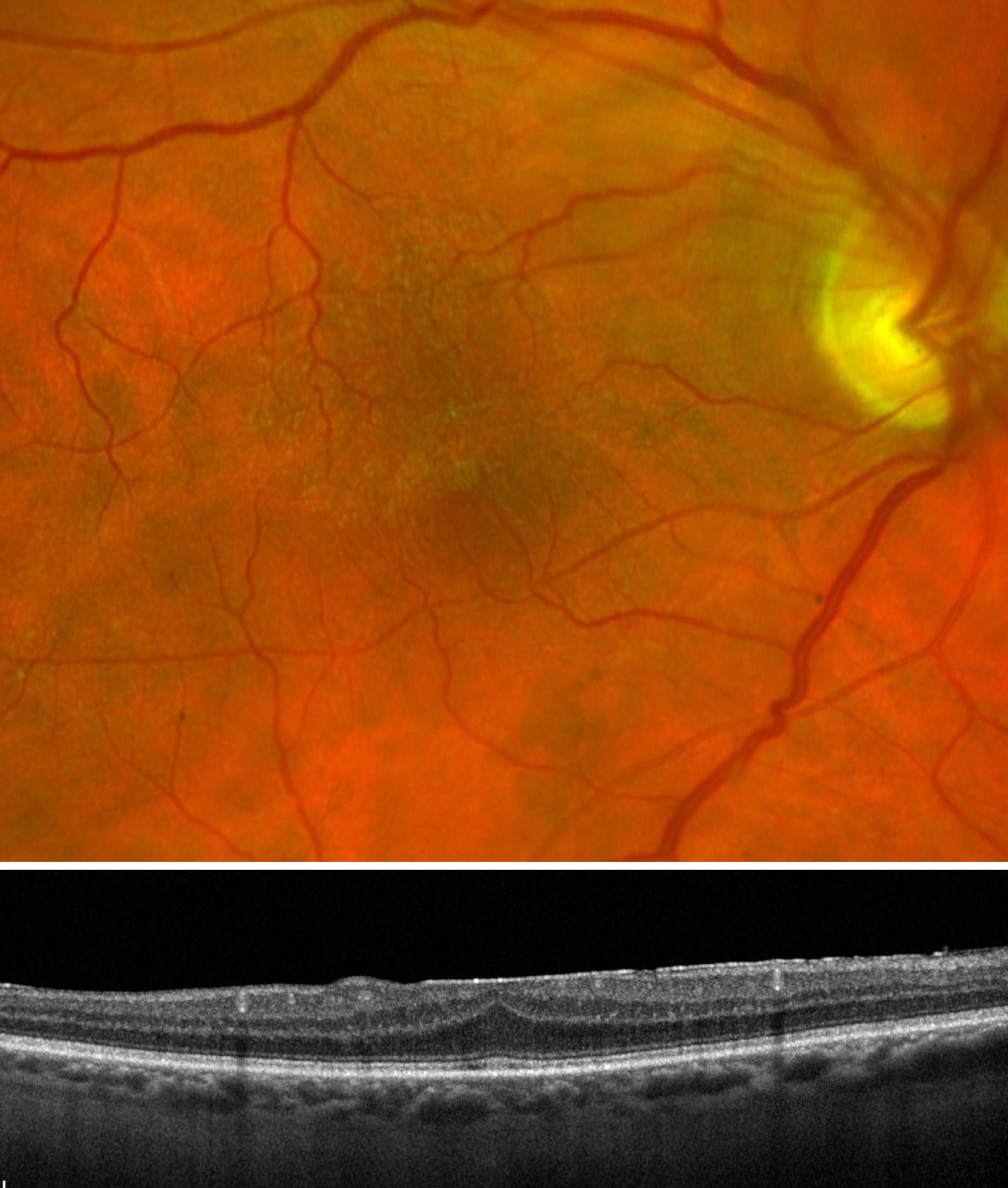
| Photo: Rami Aboumourad, OD. Click image to enlarge. |
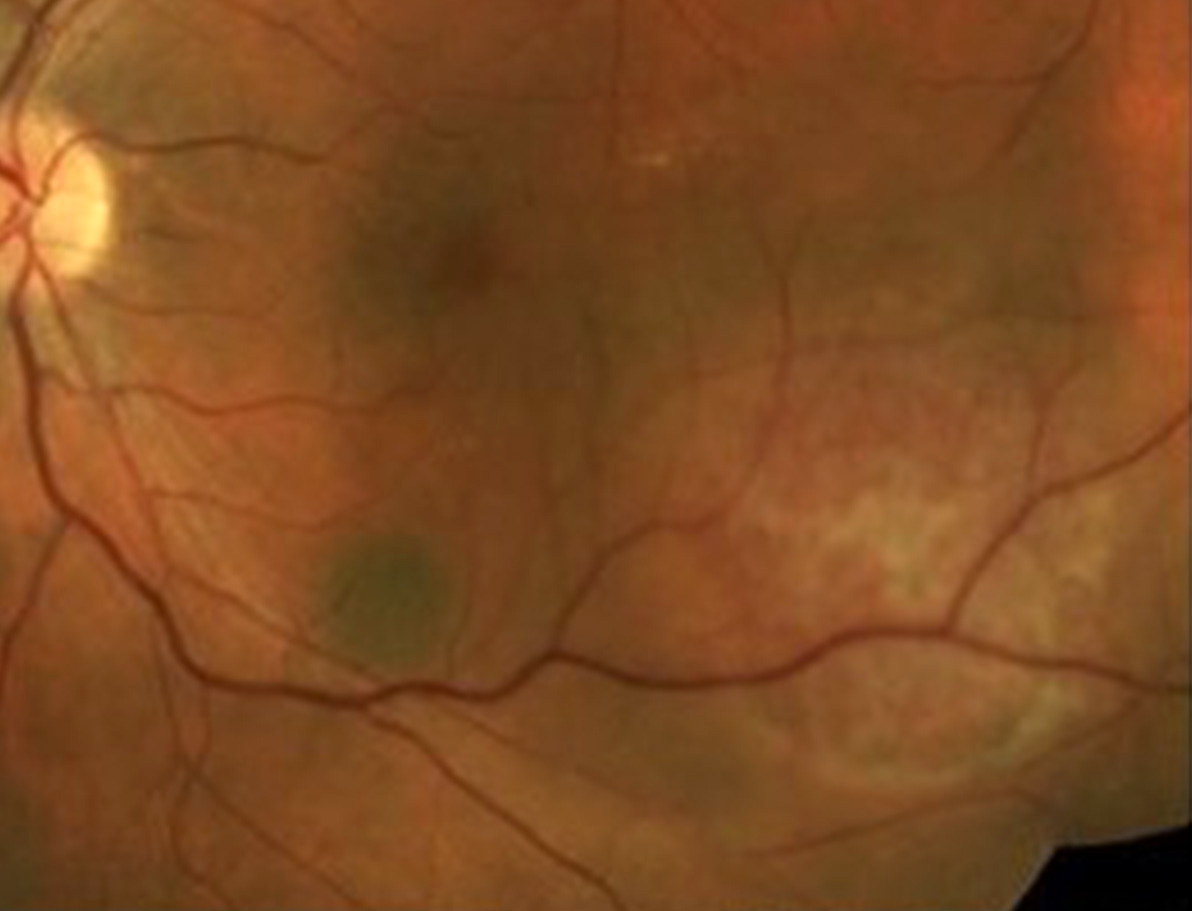
Fundus photo of central serous chorioretinopathy showing a well-demarcated round area of subretinal fluid in the superior macula and involving the fovea. There is also focal subretinal fibrinous exudation near the source (confirmed via FA) of exudation.
Suggested reading:
Get Serious About Central Serous Chorioretinopathy
Men with CSCR Have Higher Rates of Recurrence and Vision Decline
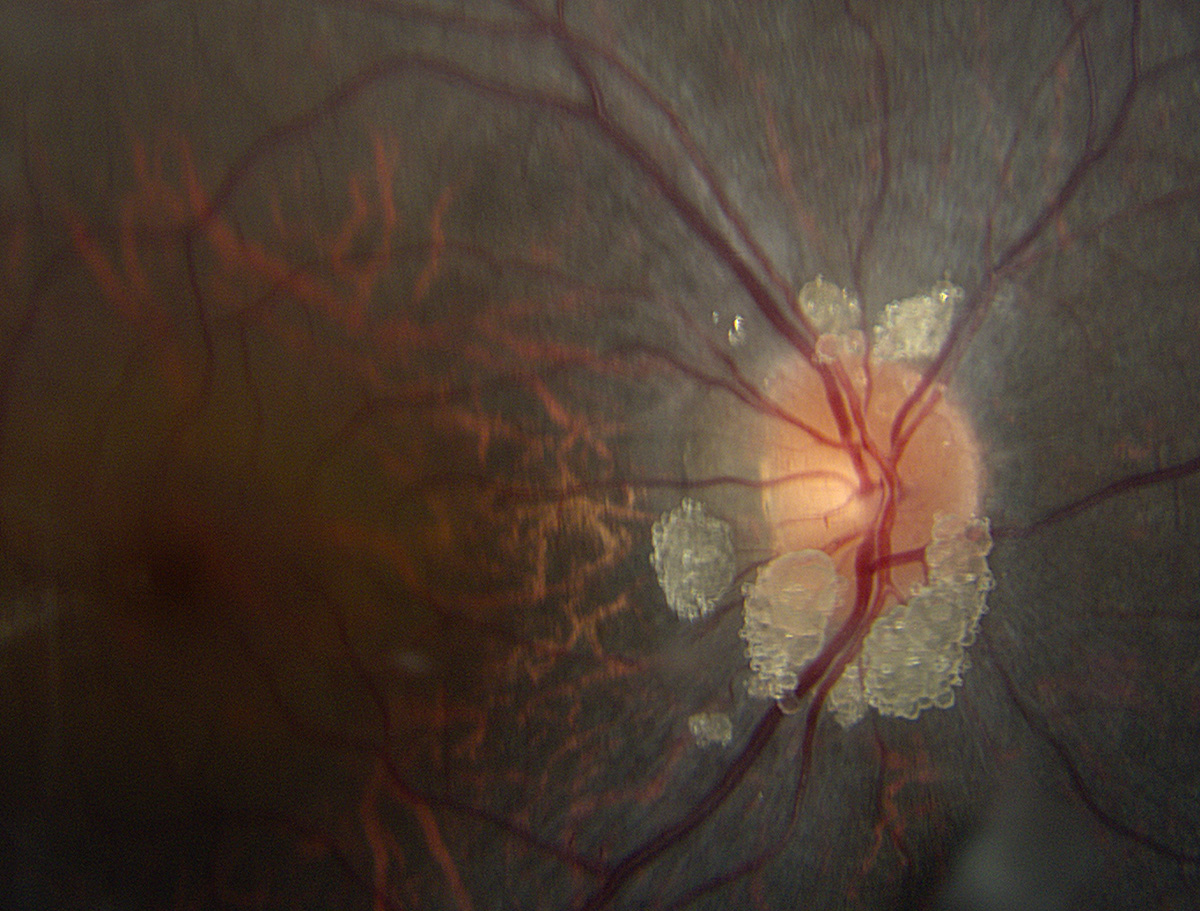
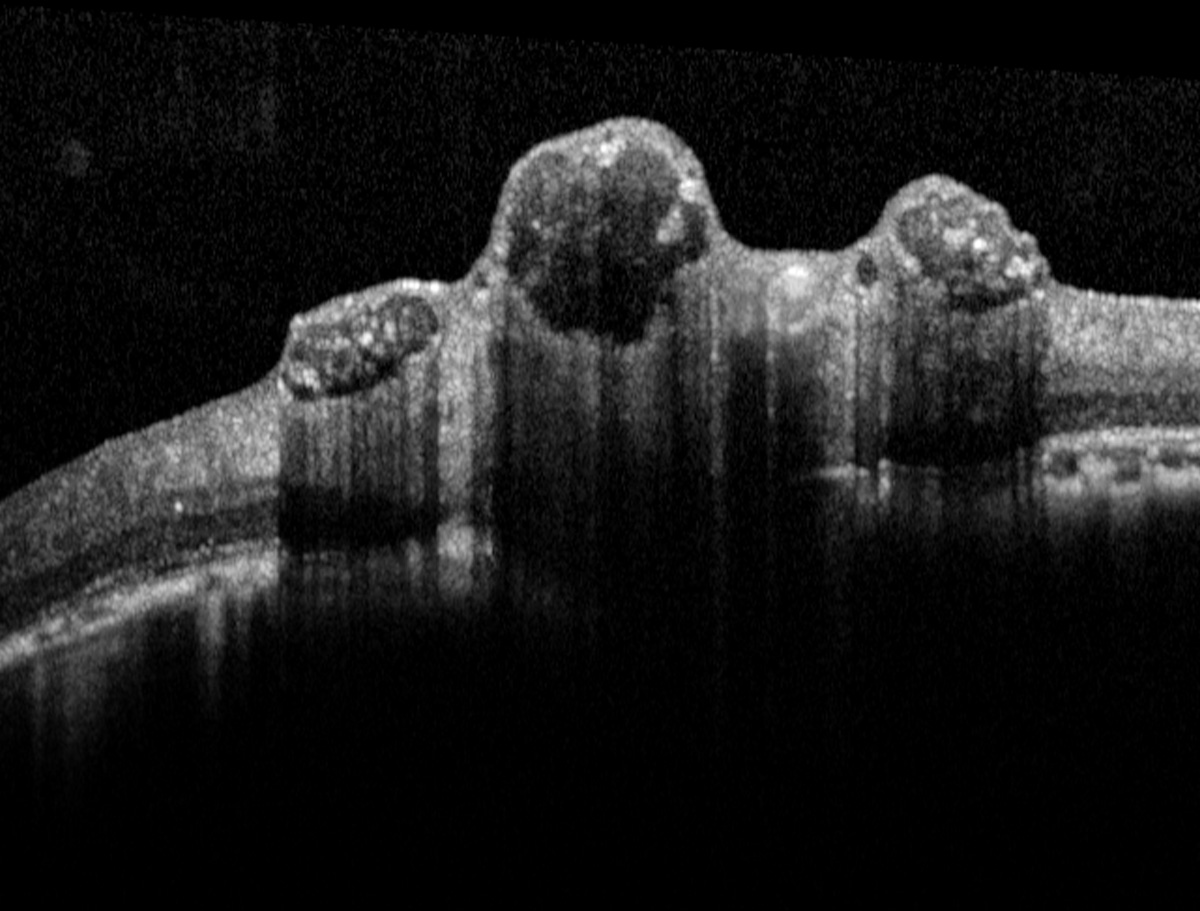
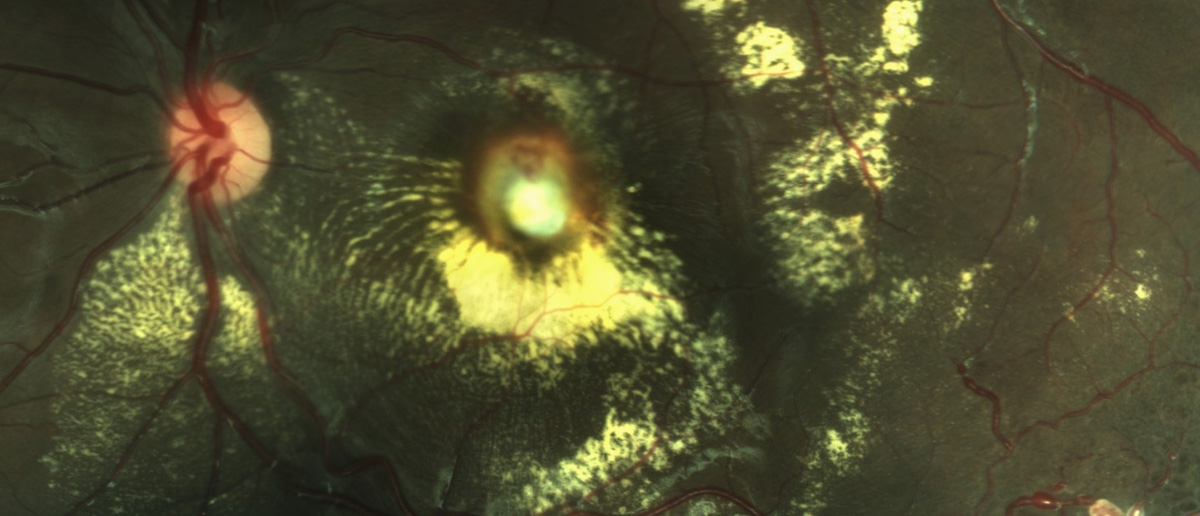
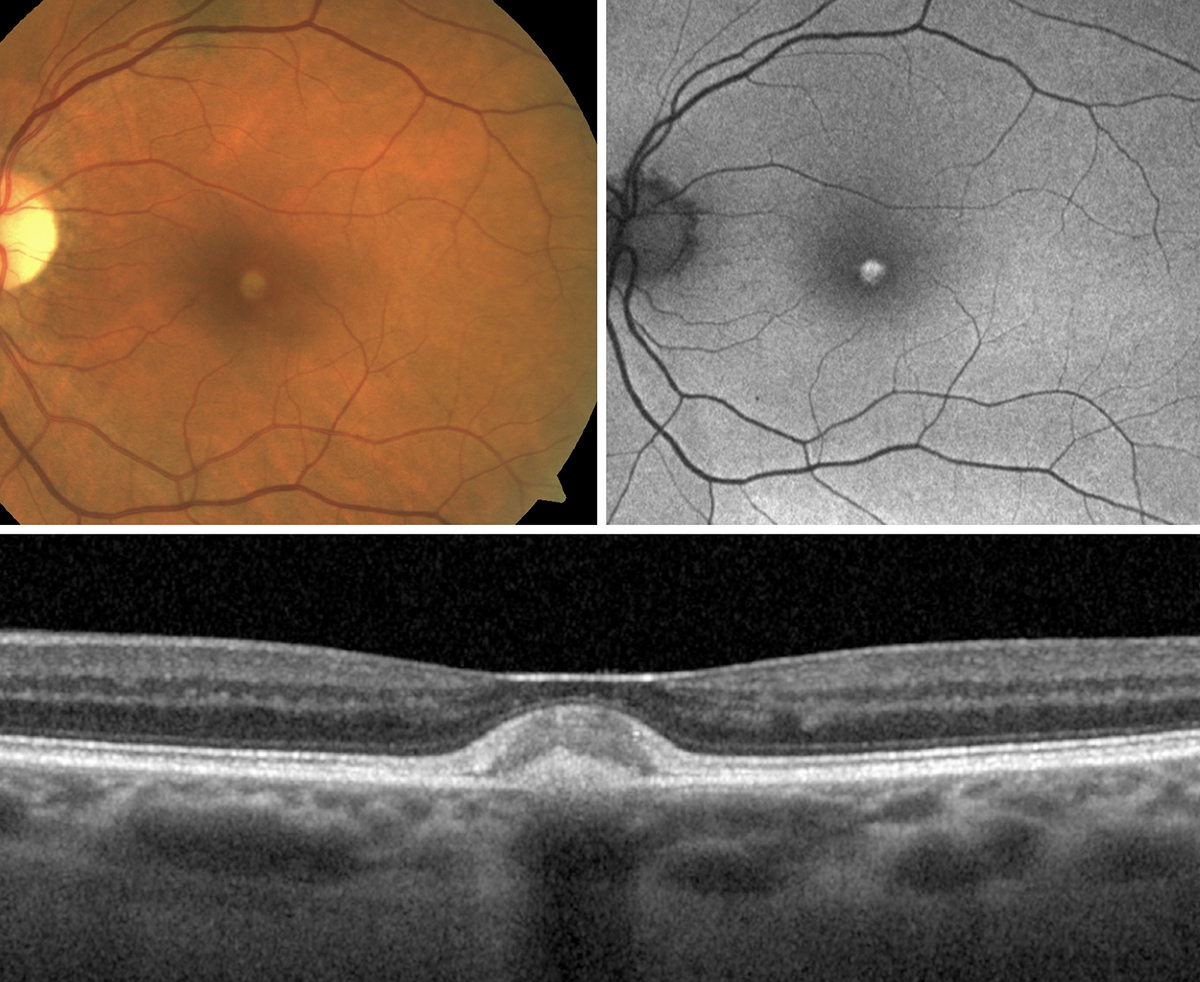
Astrocytic hamartoma
 |
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Fundus photo (first image) of retinal astrocytic hamartomas showing the typical appearance of elevated, globular, yellow-white nodules. These lesions arise from glial tissue and will hyperautofluoresce once calcified. OCT through retinal astrocytic hamartomas (second image) shows characteristic "moth-eaten" or optically empty hyporeflective spaces within the RNFL.
Suggested reading:
Don’t Berry this Clinical Finding
CMV retinitis
 |
| Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
CMV retinitis with classic frosted branch angiitis—yellow lesions surrounding blood vessels. CMV retinitis can also appear with a "ketchup and cheese" hemorrhagic necrosis or with granular necrotic tissue. CMV retinitis can occur in patients who are HIV positive, and while it is now rare with current HIV therapies, one must still be on the lookout for it.
Suggested reading:
The Bugs Behind Infectious Retinitis
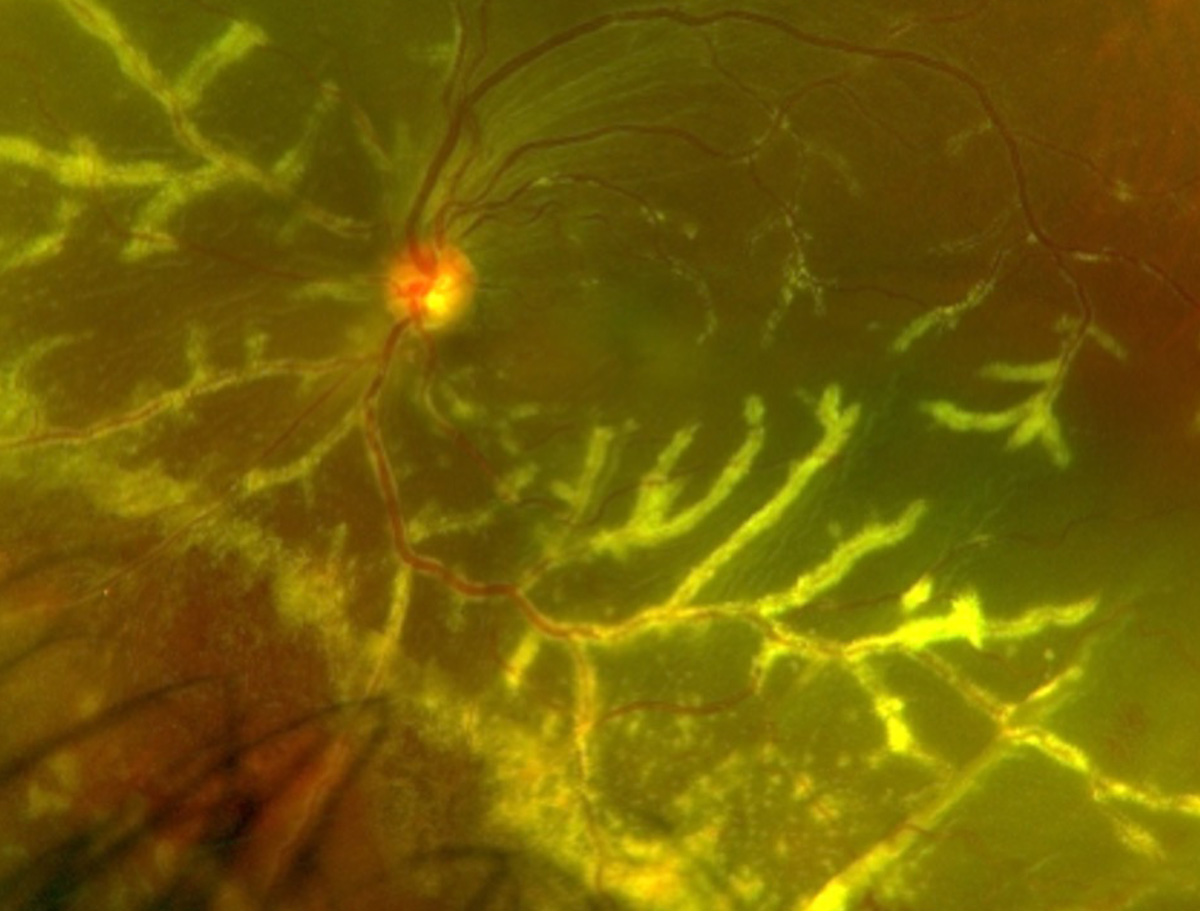
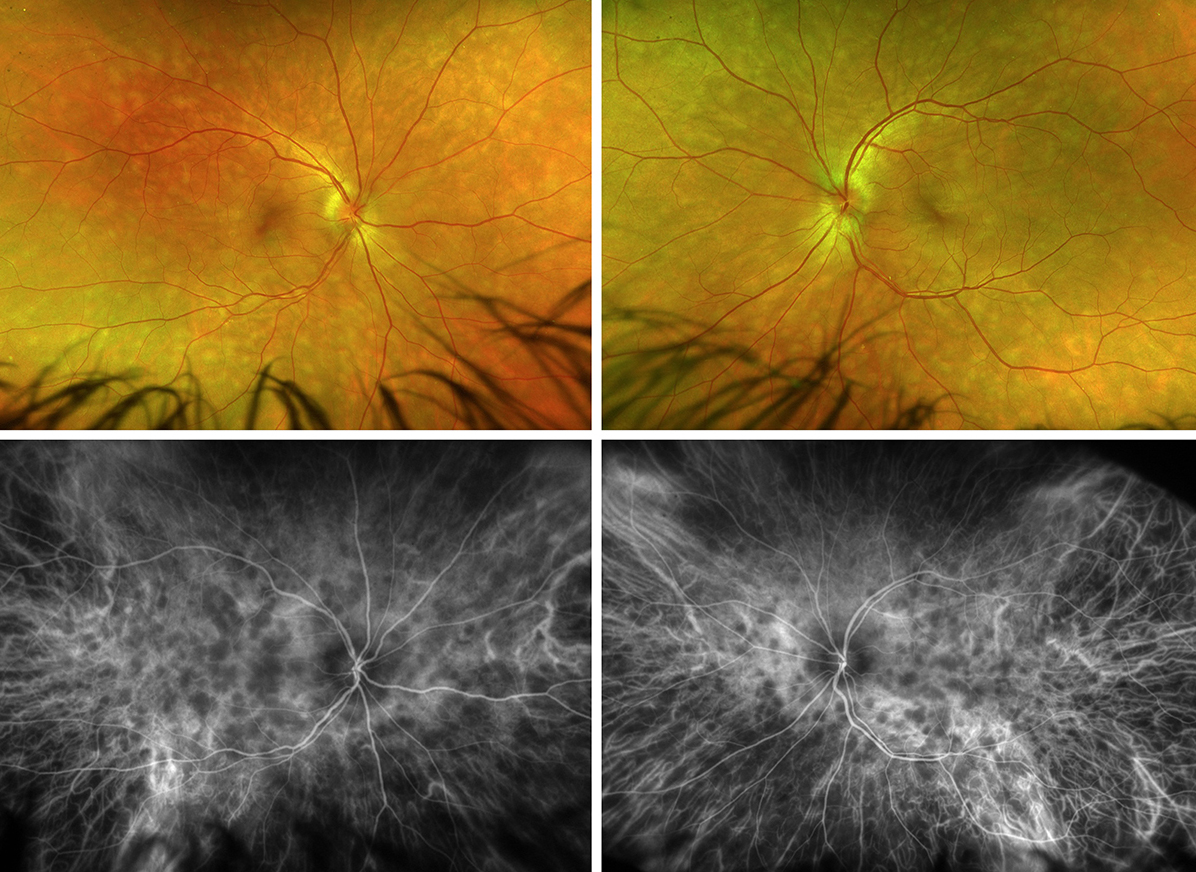
Birdshot retinopathy
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Deep, yellow oval shaped birdshot lesions radiating from the disc. These classic choroidal lesions may not appear initially during the course of the disease and patients may first present with non-specific symptoms such as photopsias, floaters and nyctalopia. Adjunct testing such as OCT, FAF, IVFA and ICGA can be very helpful in assisting with the diagnosis of birdshot. Patients may also present with a mild anterior chamber reaction and/or mild vitritis.
Suggested reading:
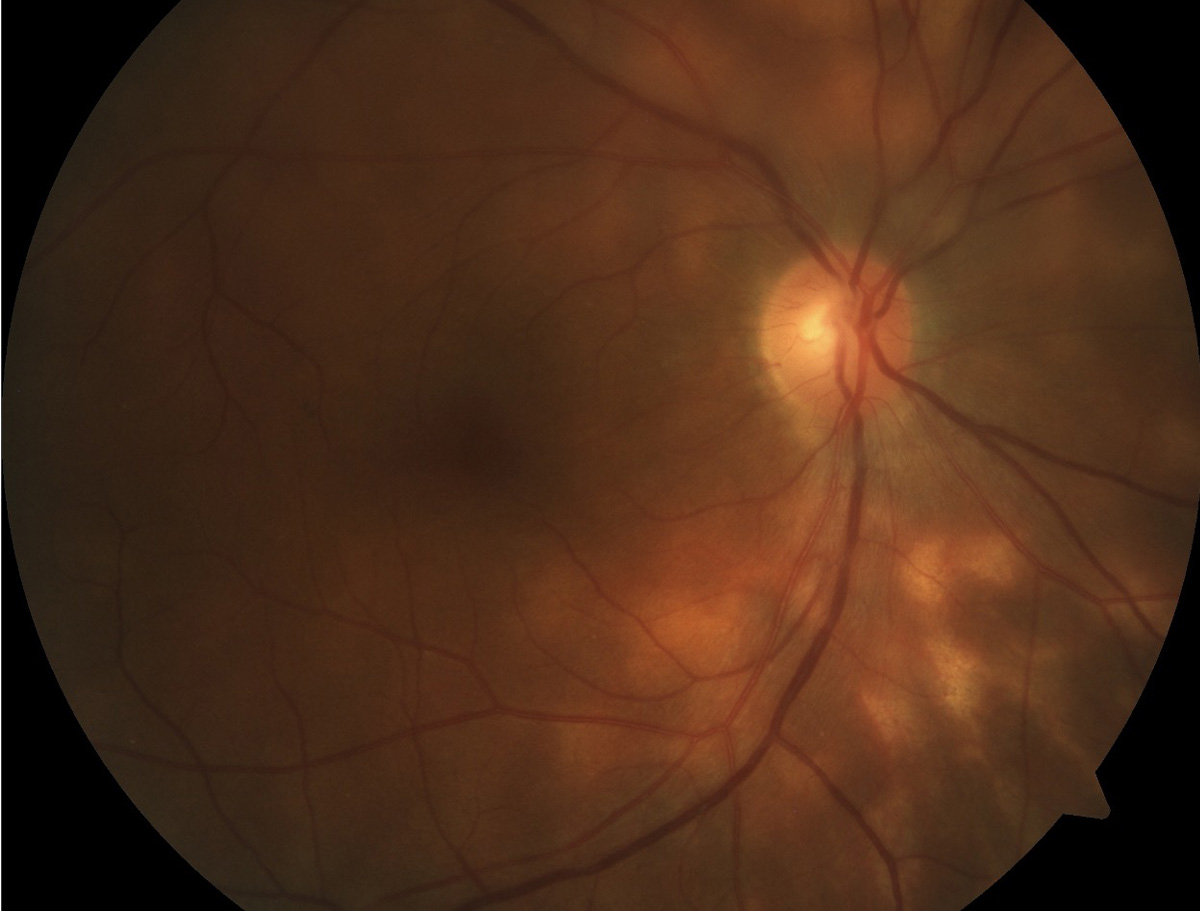
Coats disease
 |
| Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Coats disease’s most striking findings are large areas of exudation and irregular, telangiectatic vessels or aneurysms. It most commonly presents unilaterally in young male patients.
Suggested reading:
Coats’ Disease Affects Both Eyes
Macular telangiectasia
 |
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Fundus photo of macular telangiectasia (first image). The telangiectatic vessels in the macula are unique because they make abrupt right angles. The second image is an OCT of macular telangiectasia showing abrupt inner-retinal atrophy and cavitation with ILM draping temporal to the fovea. Additionally, there is disruption in the IS/OS line temporal to the fovea.
Suggested reading:
Severe Vision Loss Rare In MacTel
Noninvasive Screening Tools Earn Good Marks for MacTel
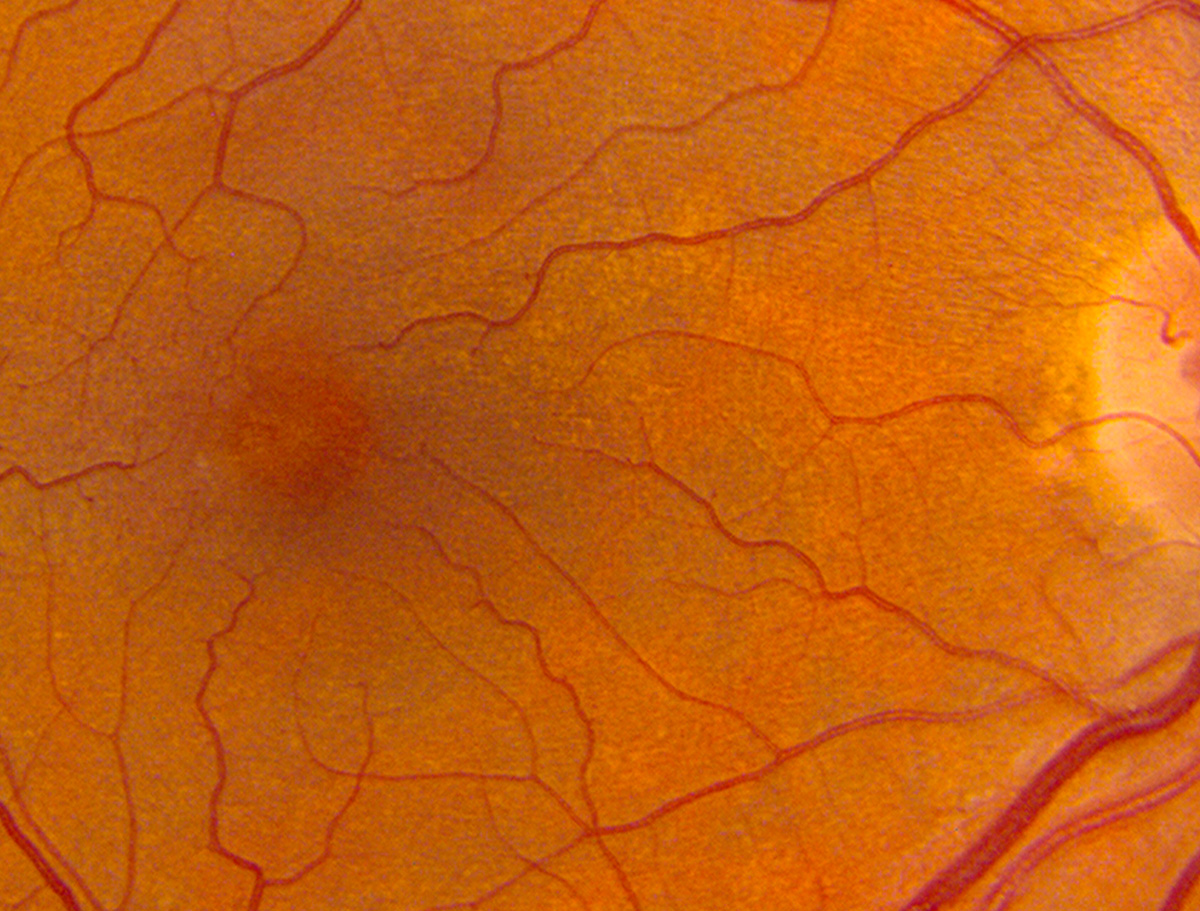
Lattice degeneration
 |
| Photo: Rami Aboumourad, OD. Click image to enlarge. |
Fundus photo OS shows 90 degrees of circumferential midperipheral lattice retinal degeneration with atrophic holes and some pigmentation.
Suggested reading:
A Field Guide to Retinal Holes and Tears
Navigating the Retinal Periphery
Can We Pre-empt Damage from Retinal Detachment?
Lattice Degeneration Top Risk Factor for RRD, Retinal Tear After Cataract Surgery
Peripheral Vitreoretinal Abnormalities Presage Retinal Breaks with Increasing Age
Rhegmatogenous retinal detachment
 |
| Photo: Rami Aboumourad, OD. Click image to enlarge. |
Fundus photo of a macula-on superotemporal rhegmatogenous retinal detachment. The causative break is a horseshoe tear at 11 o'clock, but there are additional horseshoe tears that can be visualized at 8, 9 & 10 o'clock. These patients should undergo 360° scleral depression to look for additional breaks.
Suggested reading:
Rhegmatogenous Retinal Detachment: How to Detect, How to Manage
A Field Guide to Retinal Holes and Tears
Can We Pre-empt Damage from Retinal Detachment?
OCT Aids Retinal Detachment Risk Assessment
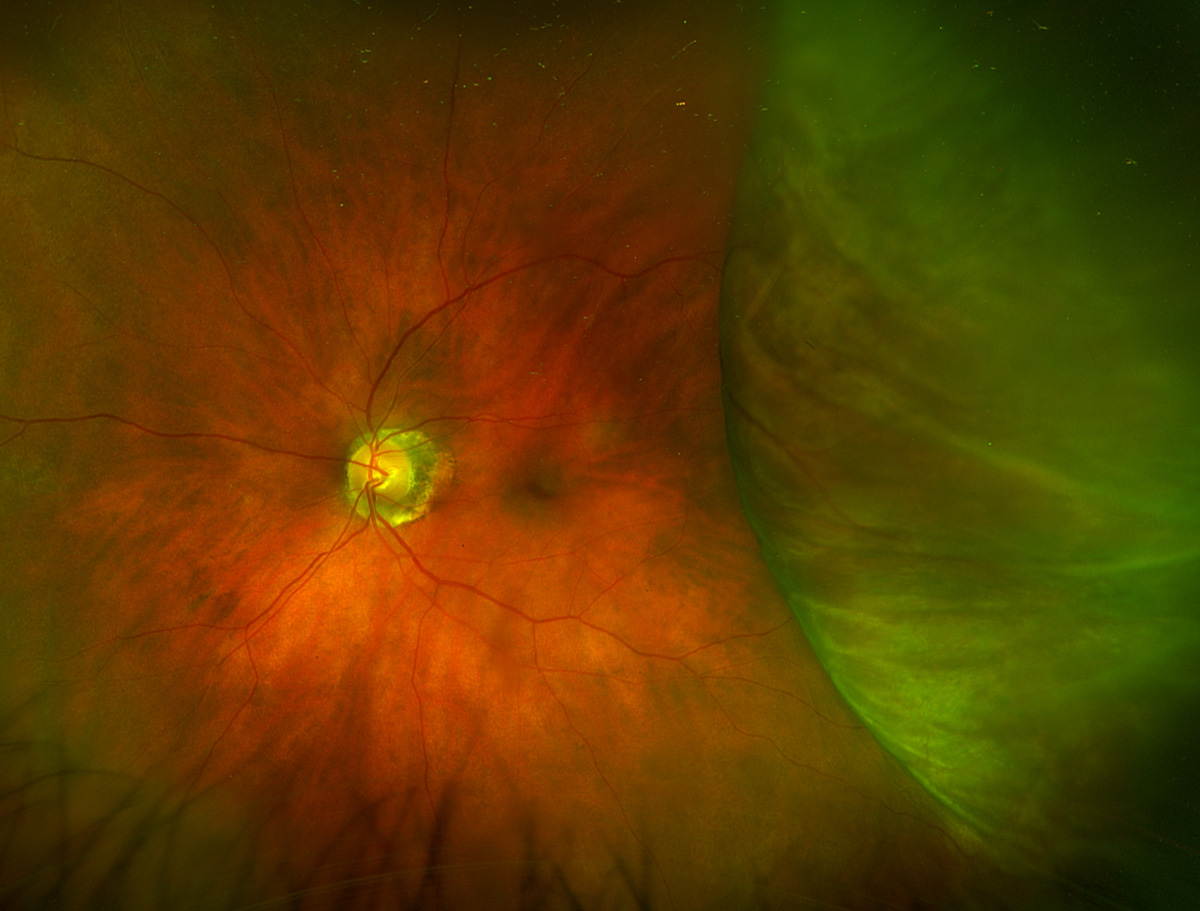
Tractional retinal detachment
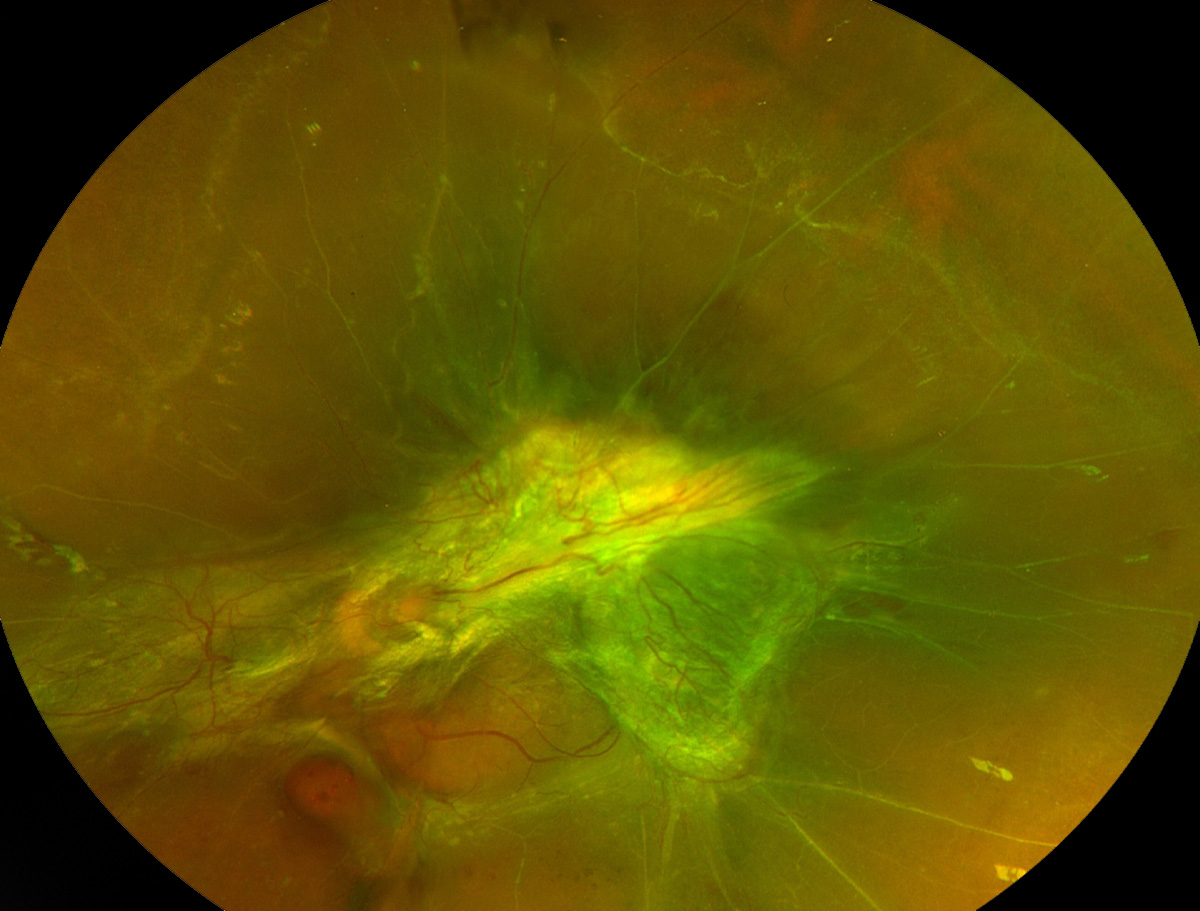 |
| Photo: Jessica Haynes, OD. Click image to enlarge. |
Tractional retinal detachments form from neovascularization in a variety of retinal pathologies. As the neovascularization grows, it uses the vitreous as a scaffold. As it becomes fibrosed, it contracts and lifts the retina, forming a TRD. On clinical examination various signs of diabetic retinopathy can be present. Irregular neovascular blood vessels are often visualized amongst the yellow, elevated fibrotic tissue, and pre-retinal or vitreous hemorrhages are also often present. The traction on the retina can also lead to a retinal break causing a combined rhegmatogenous and tractional retinal detachment. This patient has a tractional retinal detachment from proliferative diabetic retinopathy.
Suggested reading:
A Field Guide to Retinal Holes and Tears
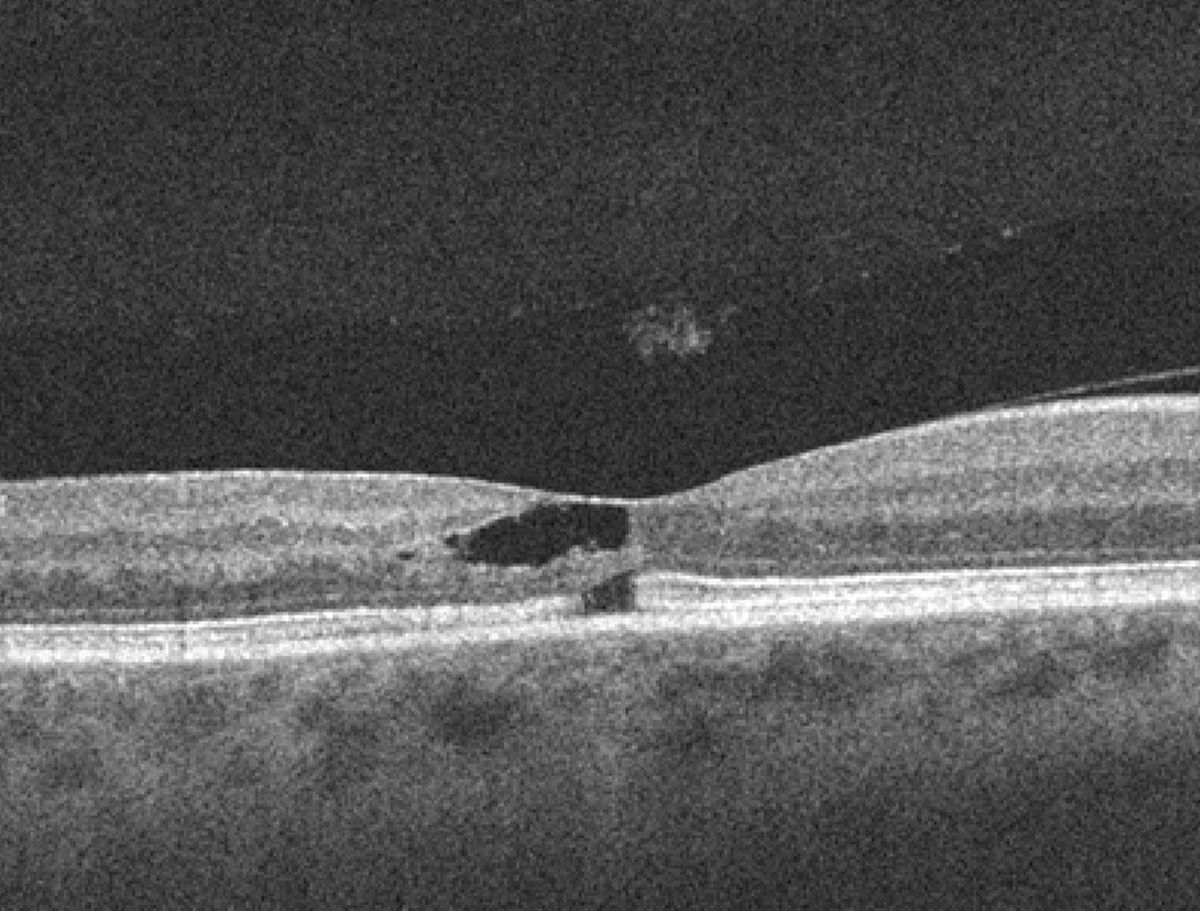
Vitreomacular traction
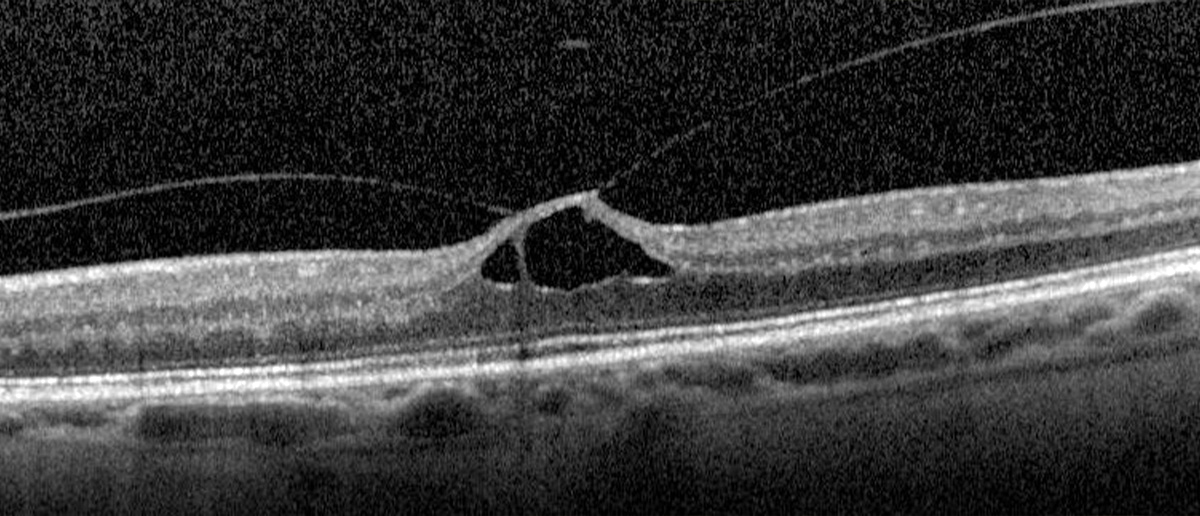 |
| Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
OCT of vitreomacular traction will show a lifting of the posterior vitreous hyaloid with residual attachments to the macula that distort retinal anatomy. This traction may result in cystic spaces.
Suggested reading:
Five Cases You Shouldn't Refer
Timing the Retinal Referral: Tips for Success
Myopic tractional maculopathy
 |
| Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Myopic traction maculopathy leads to a splitting of retinal layers in the macular region. It is best visualized using OCT.
Suggested reading:
Characteristics of Advanced Myopic Traction Maculopathy Identified
Horseshoe tear
 |
| Photo: Rami Aboumourad, OD. Click image to enlarge. |
Peripheral fundus exam shows two adjacent horseshoe retinal tears superotemporally within an area of lattice degeneration. These patients require careful scleral depressed examination bilaterally to ensure all breaks are identified.
Suggested reading:
A Field Guide to Retinal Holes and Tears
Timing the Retinal Referral: Tips for Success
For Horseshoe Tears, Two Tests are Better Than One
Can We Pre-empt Damage from Retinal Detachment?
Retinoschisis
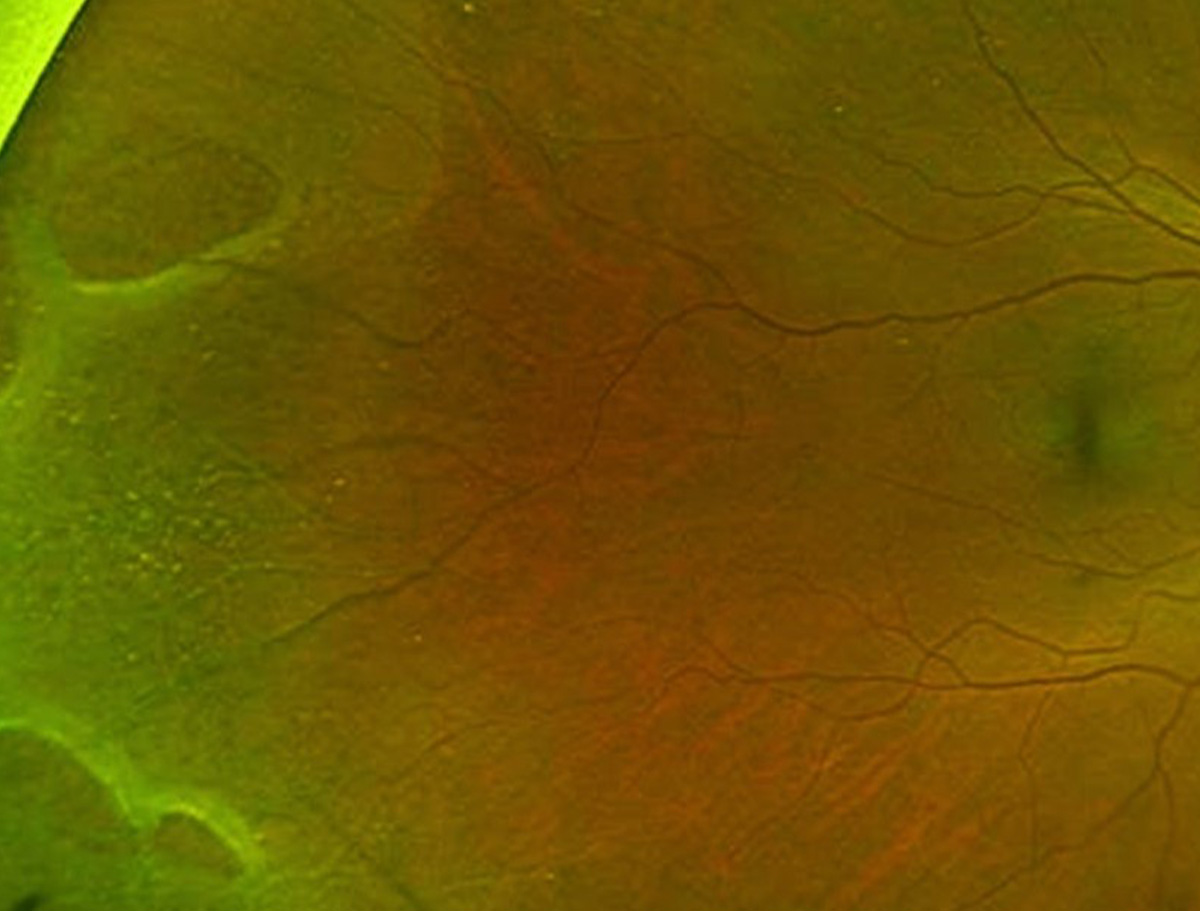 |
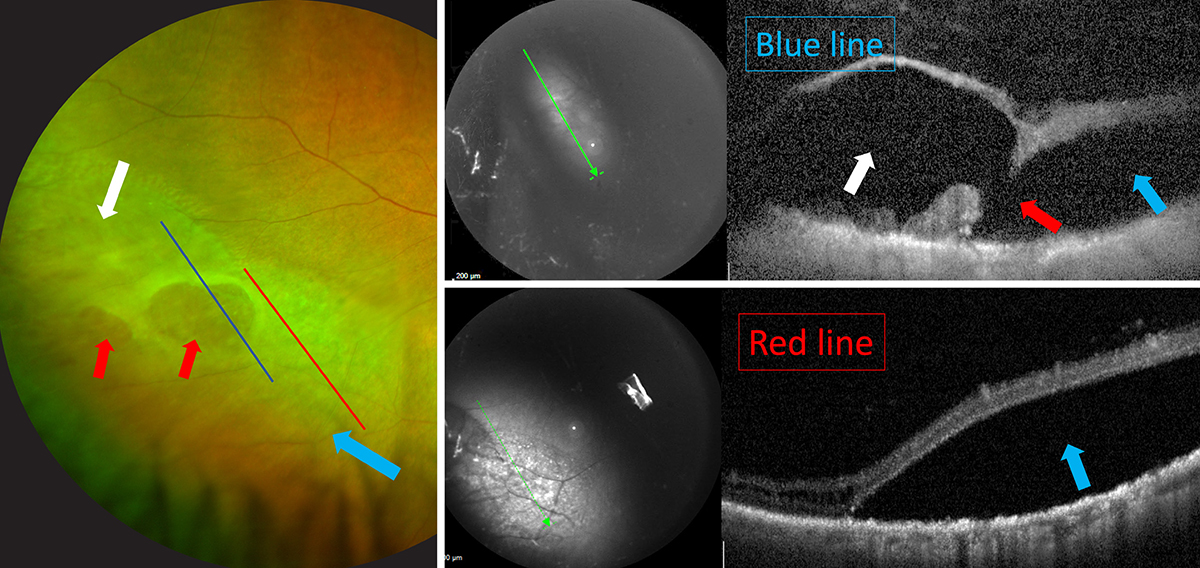
| Photos: Mohammad Rafieetary, OD; Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
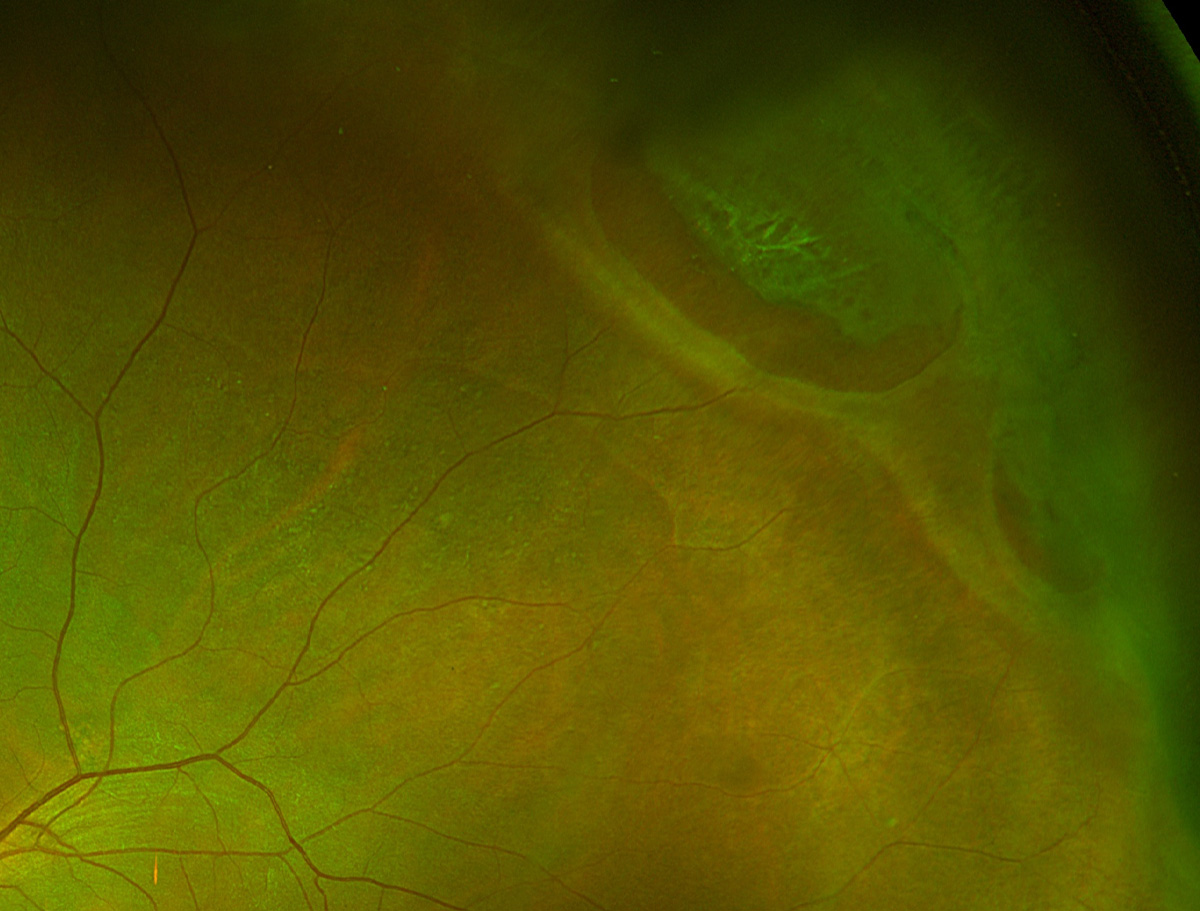
A retinoschisis is a splitting of the retina typically at the level of the outer plexiform layer. Peripheral retinoschisis (first image) most often occurs temporally, superior temporally or inferior temporal, and is most often bilateral.
The term "retinoschisis" has been used to describe a few different types of conditions, such as myopic macular schisis, but when one is referencing the peripheral retinal degeneration known as retinoschisis, these are often round, bullous elevations most commonly located inferior temporal temporal or superior temporal; they are typically bilateral.
On clinical examination, it can be difficult to distinguish a retinoschisis from other findings such as white without pressure and retinal detachment. In addition, a retinoschisis can develop into a retinal detachment. A peripheral retinoschisis can develop holes or breaks in the inner retinal layers (inner layer break) and/or the outer retinal layers (outer layer break). If fluid penetrates through an outer layer break, an area of retinal detachment can form.
The second image (photo and OCTs) is a patient with schisis-related retinal detachment and outer layer retinal breaks. The white arrows point towards a region of schisis cavity. The red arrows point towards the outer layer breaks and the blue arrows point towards a region of detachment.
Suggested reading:
Navigating the Retinal Periphery
Can We Pre-empt Damage from Retinal Detachment?
Retinal tufts
 |
| Photos: Mohammad Rafieetary, OD. Click image to enlarge. |
Cystic retinal tufts often present as localized, fluffy white lesions in the peripheral retina. They may have associated RPE hyperplasia and be pigmented as well. On OCT, retinal tufts will show areas of vitreous adhesion to the retinal surface.
Suggested reading:
Navigating the Retinal Periphery
A Field Guide to Retinal Holes and Tears
Can We Pre-empt Damage from Retinal Detachment?
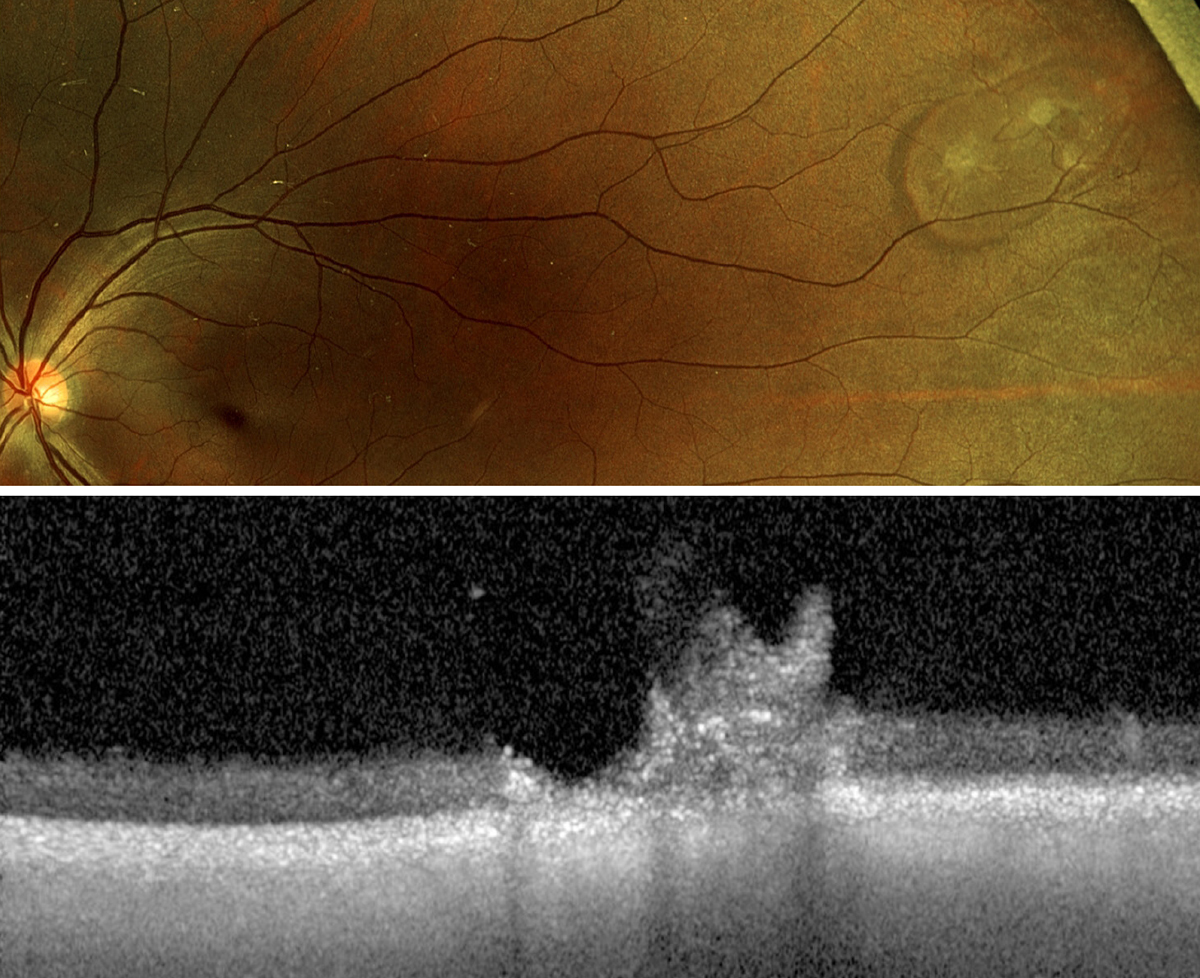
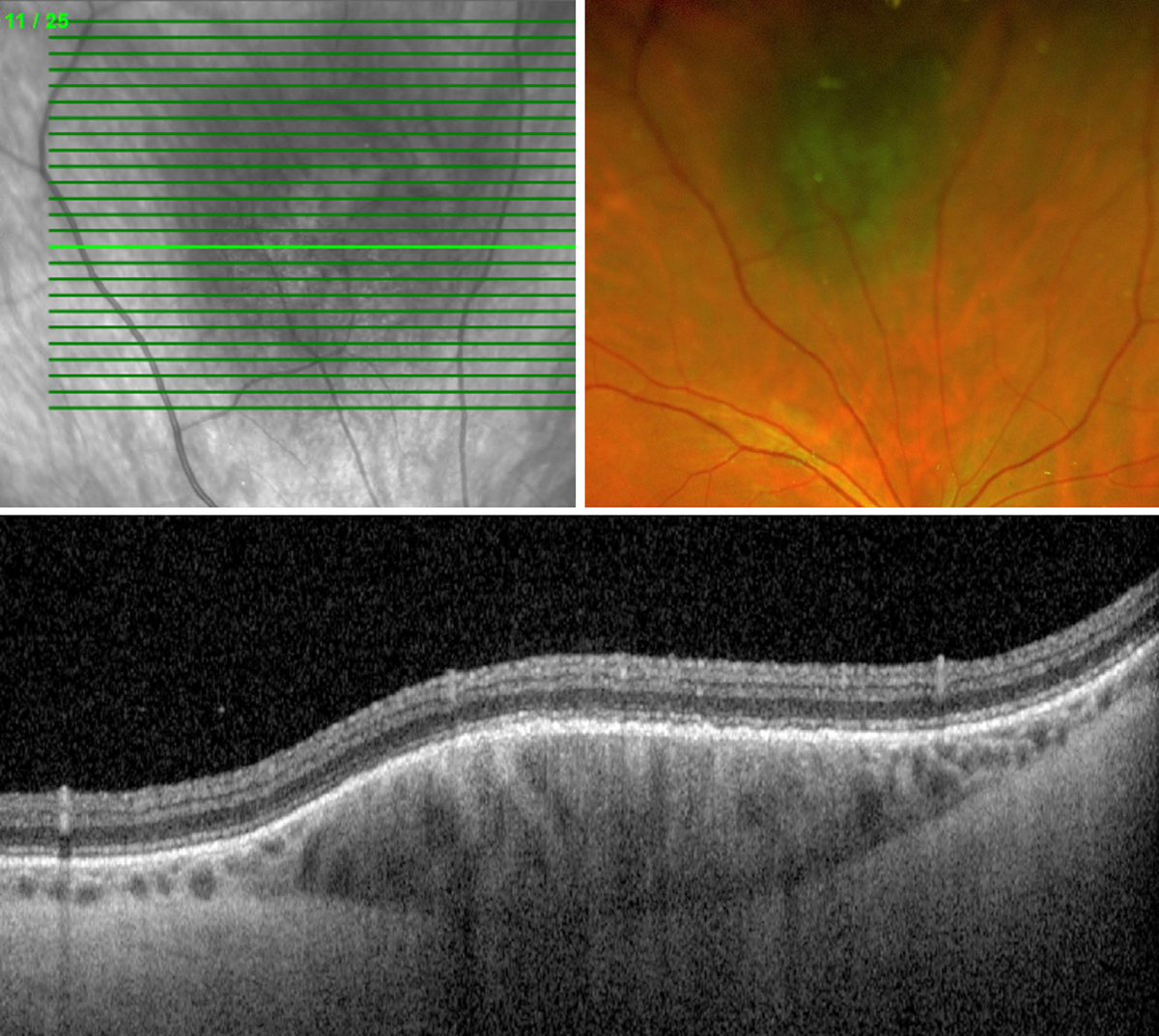
Choroidal effusion
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Choroidal detachments or effusions are a separation of the choroid from the sclera. They occur when there is accumulation of fluid or blood in the suprachoroidal space. They can be caused by many etiologies, including hypotony, inflammation, metastasis and in the setting of choroidal effusion syndrome. They are typically large, round, elevated, opaque lesions. This patient has a choroidal detachment from hypotony post trabeculectomy.
Suggested reading:
Choroidal Folds: A New Wrinkle in Retinal Care
Macular hole
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
 |
| Click image to enlarge. |
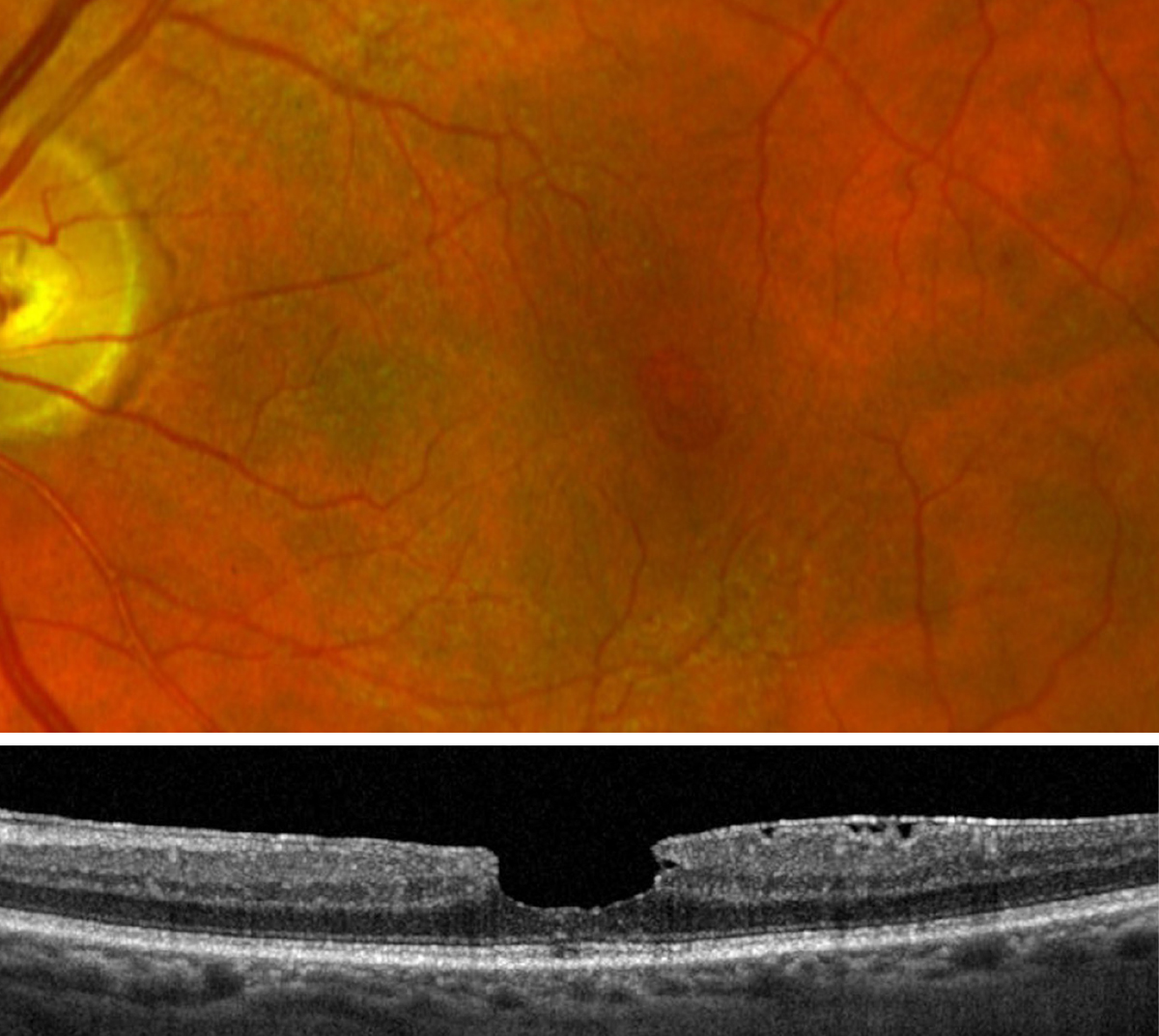 |
| Click image to enlarge. |
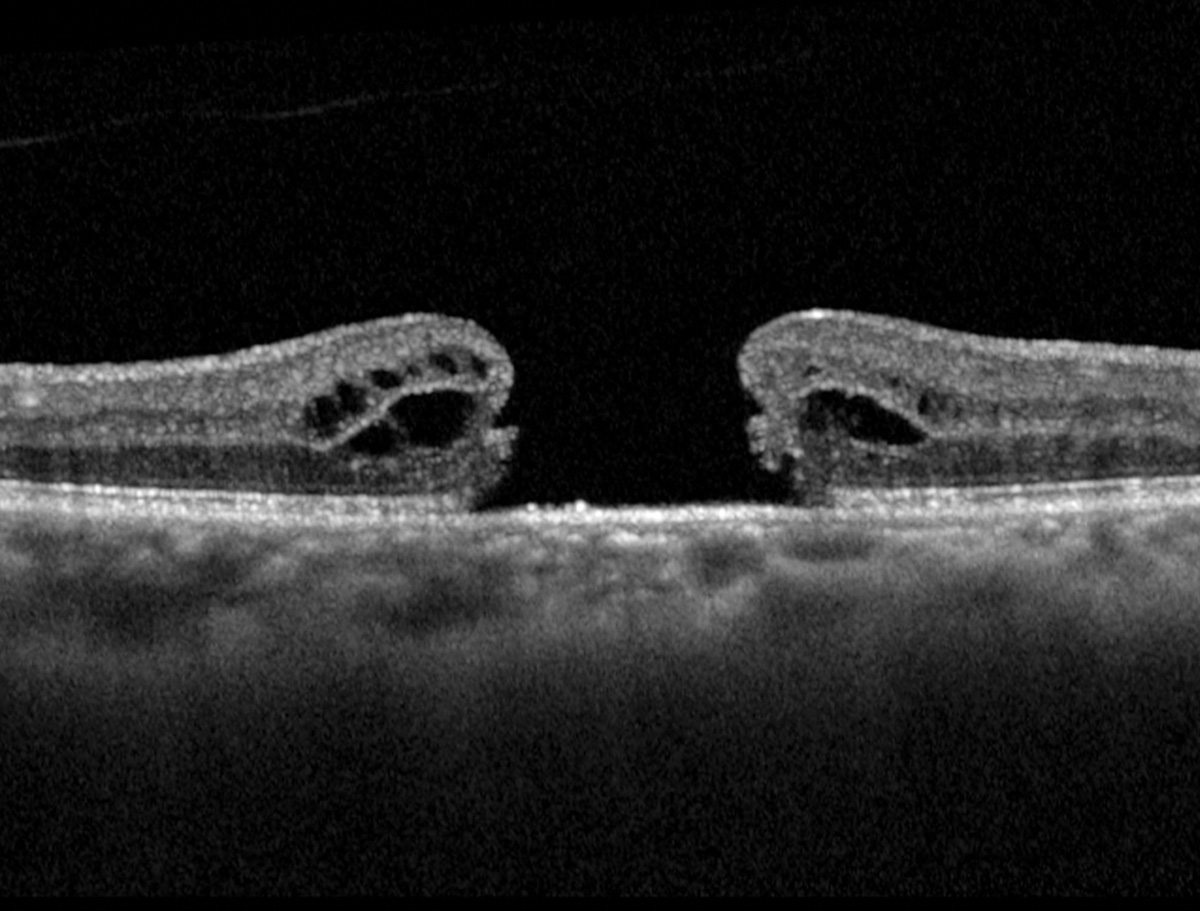
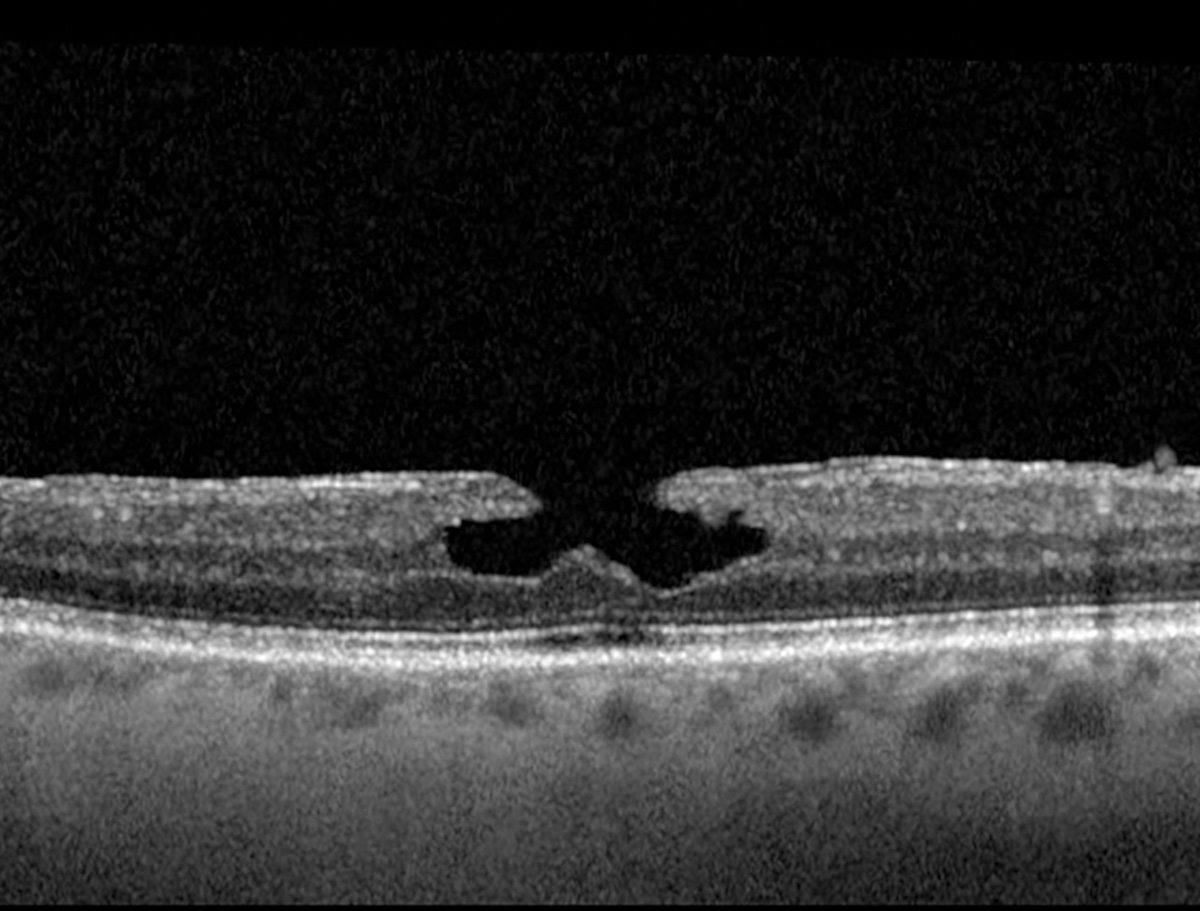
A full-thickness macular hole (FTMH) may be visualized with fundus examination (first image) as a round, reddish lesion in the fovea. The patient may also present with scotomas, metamorphopsia or decreased visual acuity. OCT is an invaluable tool in confirming the presence of a FTMH (second image). There will be a gap in the entirety of the neurosensory retina.
A lamellar macular hole (third image), by contrast, consists of an irregular foveal contour with a separation of the inner retina layers from the outer retinal layers, without a full-thickness retinal break. These may be difficult to visualize on clinical examination and may appear as a distorted light reflex or round, reddish lesion in the fovea. OCT is the best tool to differentiate a lamellar macular hole from FTMH; however, other clinical tricks such as the Watze-Allen sign can also be beneficial.
The term macular pseudohole is a pre-OCT term used to describe a round, reddish appearance in the fovea (fourth image) without presence of a full-thickness macular hole; hence, "pseudo" hole. Classically, the term has been used in the presence of an epiretinal membrane that causes a deformation of the foveal pit with "sharp" abrupt borders. It is this irregular foveal pit that gives the clinical appearance of a round, reddish circular lesion. OCT will help to confirm the presence of ERM and the pseudohole foveal contour. In addition, OCT will help to confirm that there is not a FTMH. Additionally, the Watzke-Allen technique can be used clinically. With this technique, a rectangular beam is placed on the fovea and the patient is asked if they see a gap or break in the beam. If they do, then a FTMH is suspected. If they do not, the presentation could be a pseudohole.
Suggested reading:
A Field Guide to Retinal Holes and Tears
Timing the Retinal Referral: Tips for Success
Are You Clear on Your Macular Function Screening Responsibilities?
Early AMD
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
Early AMD is typically defined as having small- to medium-sized drusen with no large drusen or pigmentary changes.
Suggested reading:
Understanding AMD Presentations and Prognoses
How to Stay One Step Ahead of AMD
How Early Diagnosis Can Improve AMD Outcomes
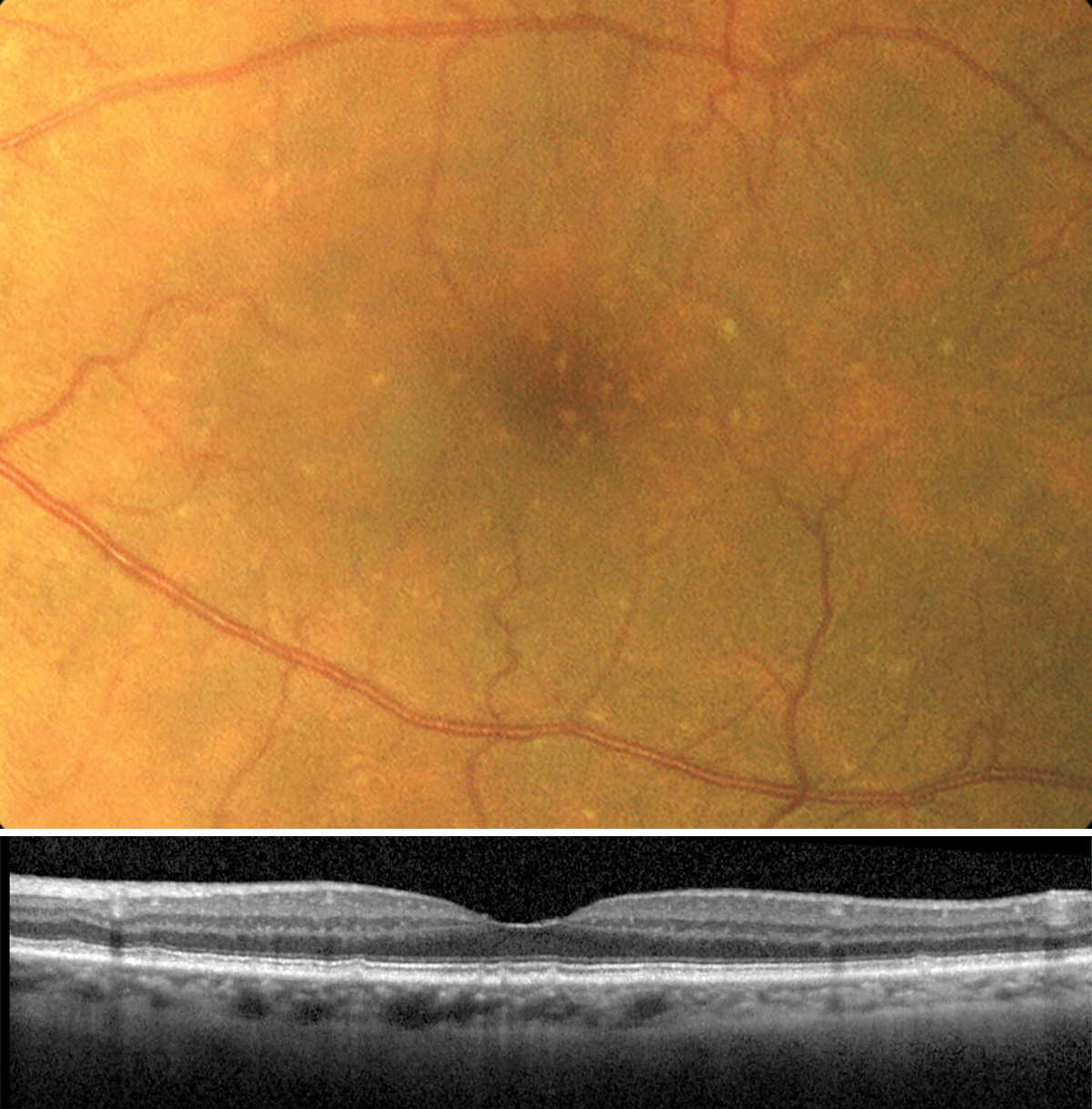
Intermediate AMD
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Intermediate-stage AMD is defined by presence of large drusen and/or pigmentary changes. Large drusen are considered to be greater than 125µm in size. On clinical examination, a reference 125µm can be gauged by looking at a major retinal vessel as it crosses the disc margin, as that diameter is also about 125µm. Drusen are typically yellow deposits that appear deeper in the retina. This patient has numerous large-sized drusen deposits.
In the OCT image of intermediate-stage AMD, multiple large drusen are also present. The most typical presentation of drusen are moderately reflective deposits that sit under the retinal pigment epithelium; however, some drusen will have irregular reflectivity within them on the OCT and there are drusen deposits called reticular pseudodrusen that sit on top of the RPE.
Suggested reading:
Understanding AMD Presentations and Prognoses
How to Stay One Step Ahead of AMD
Identifying Conversion to Wet AMD
Study Identifies Potential Markers of AMD Progression from Early to Intermediate
Dry AMD
 |
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
A case of advanced dry AMD with drusen, retinal pigment epithelial changes and geographic atrophy. It is worth noting the absence of any subretinal or sub-RPE hemorrhage on fundus exam. The fundus autofluorescence image shows multifocal geographic atrophy, represented as foci of hypoautofluorescent lesions with scattered hyperautofluorescence throughout the macula.
Suggested reading:
Five Questions on Dry AMD Monitoring and Management
Gaining Ground on Geographic Atrophy
Identifying Conversion to Wet AMD
Evaluating Visual Quality in AMD
Exudative AMD
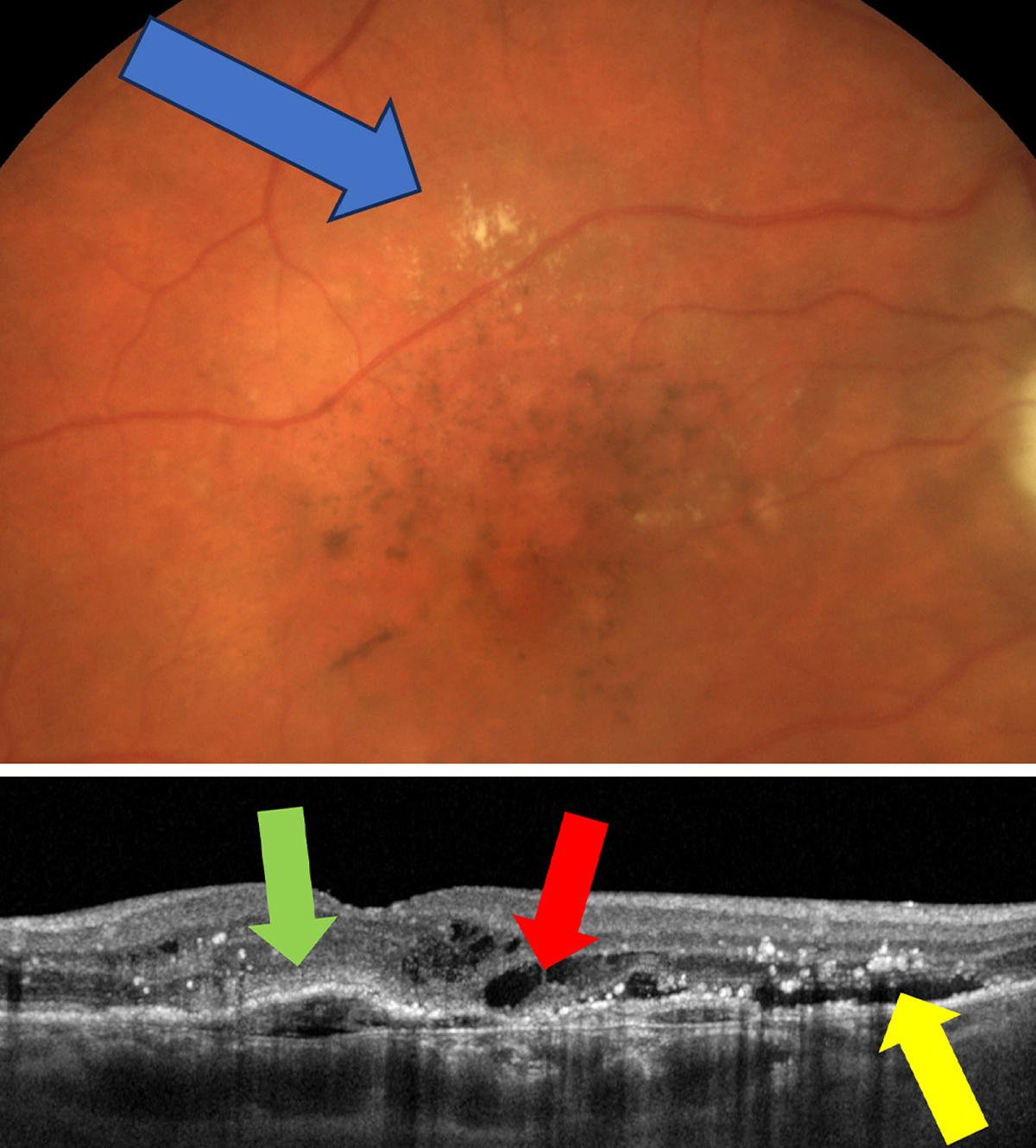 |
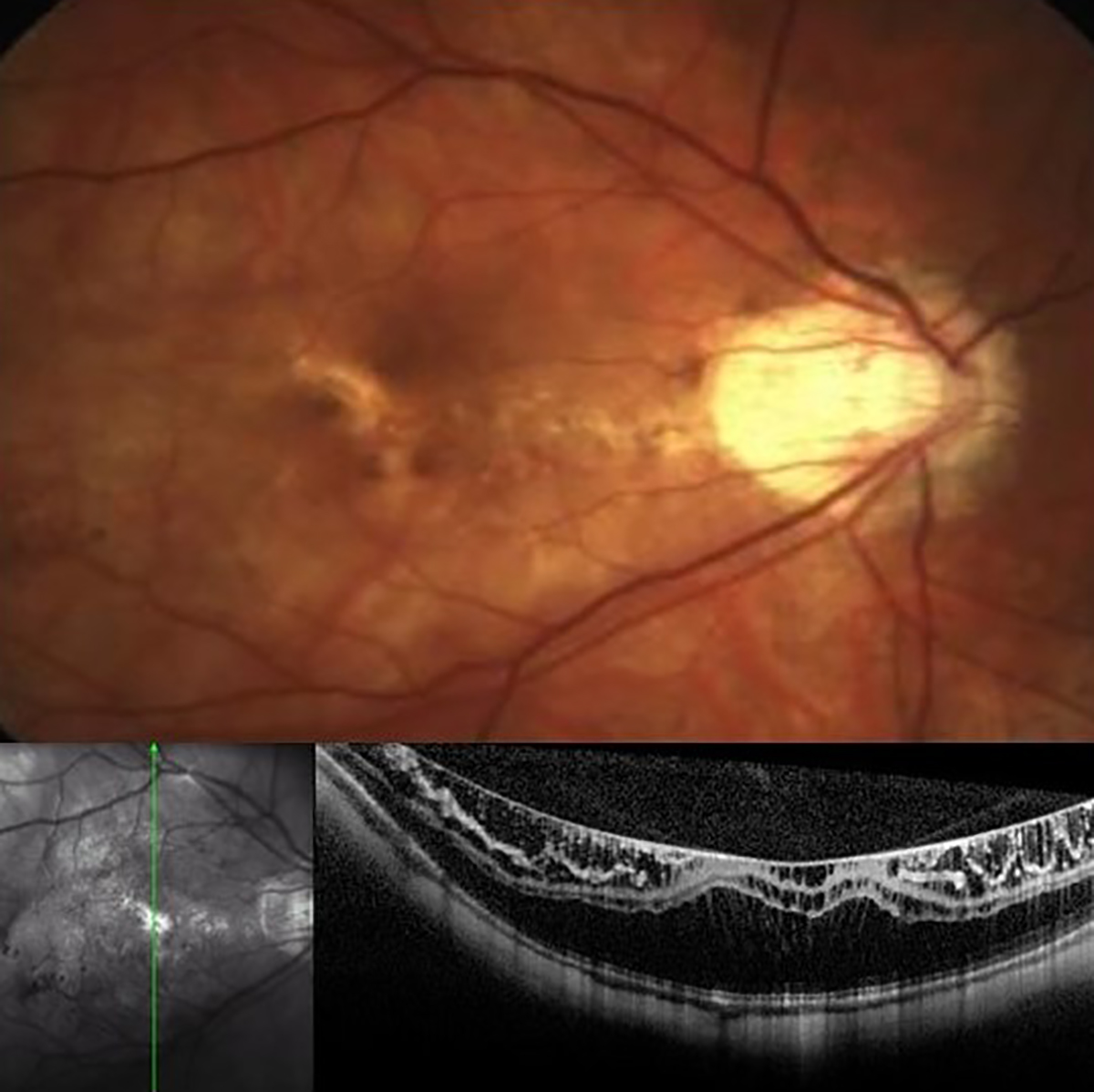
| Photos: Jessica Haynes, OD. Click image to enlarge. |
A patient with exudative AMD. The blue arrow on the fundus photo points towards exudate—a clinical clue that choroidal neovascularization could be present. On OCT, there is a pigment epithelial detachment with overlying subretinal hyperreflective material (green arrow), intraretinal fluid (red arrow) and subretinal fluid (yellow arrow)—all suggestive of CNV.
Suggested reading:
Understanding AMD Presentations and Prognoses
Neovascularization: A Small Solution to a Big Problem
Identifying Conversion to Wet AMD
Evaluating Visual Quality in AMD
Study Describes Anatomical Features that Contribute to Poor VA in Wet AMD
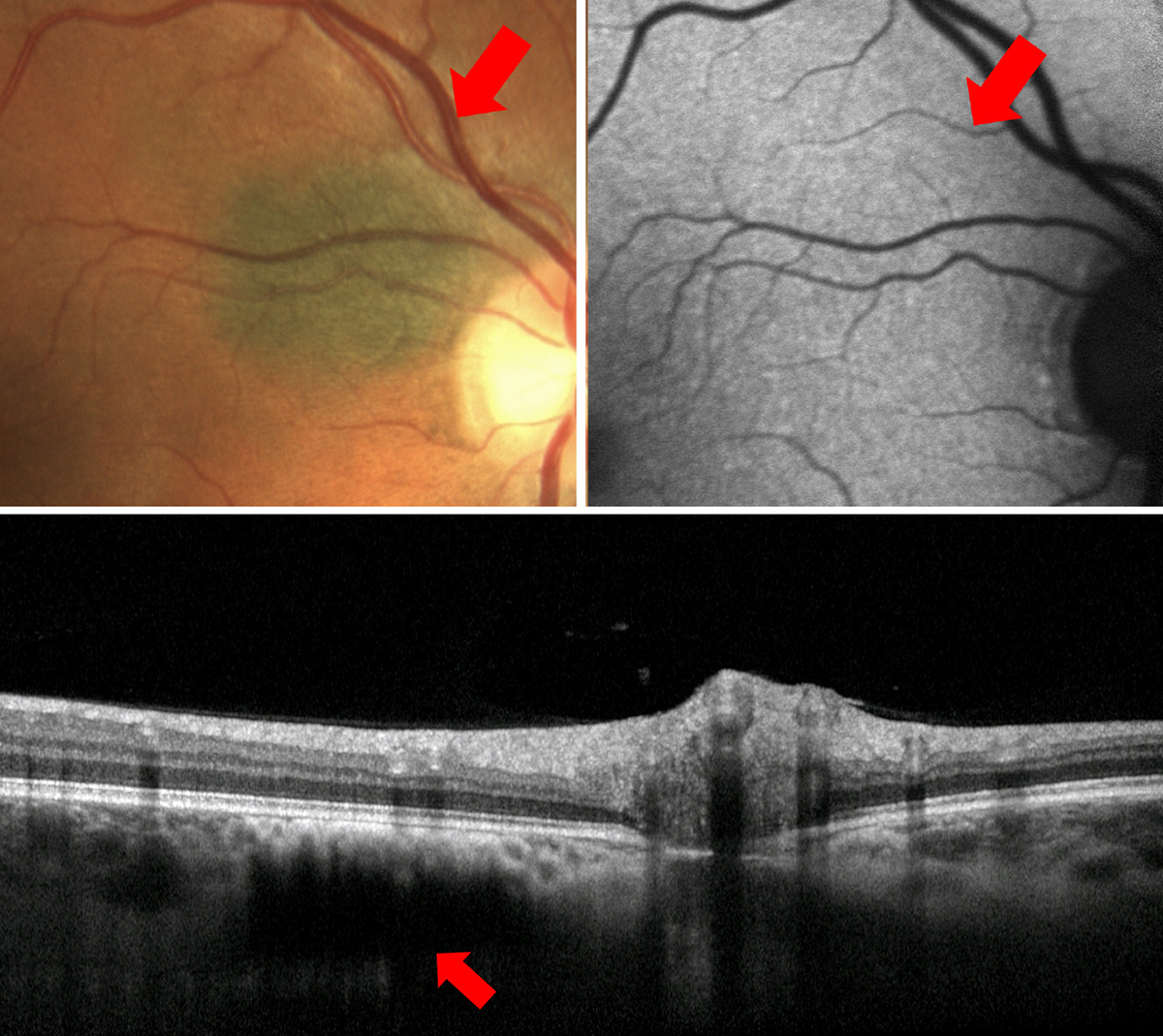
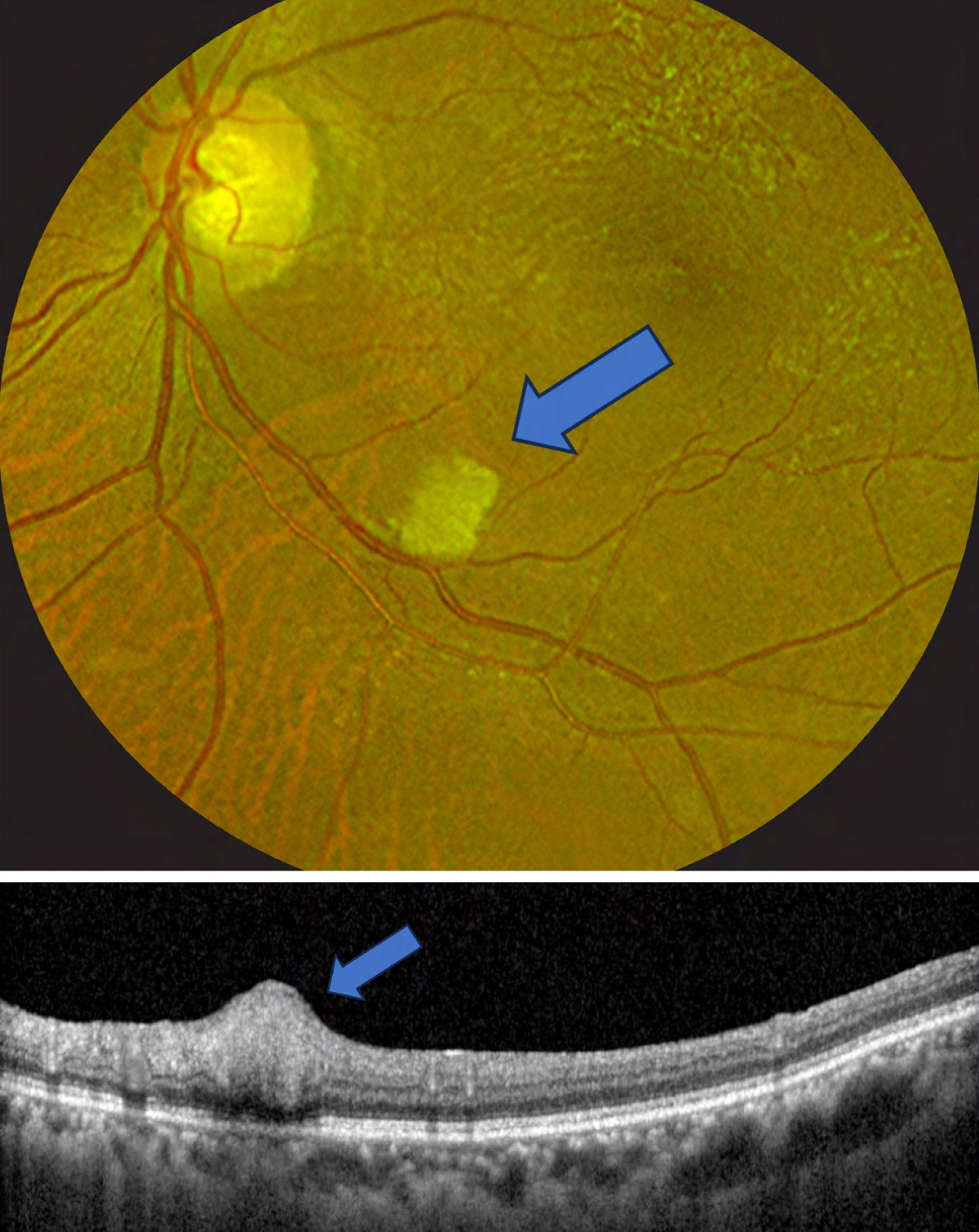
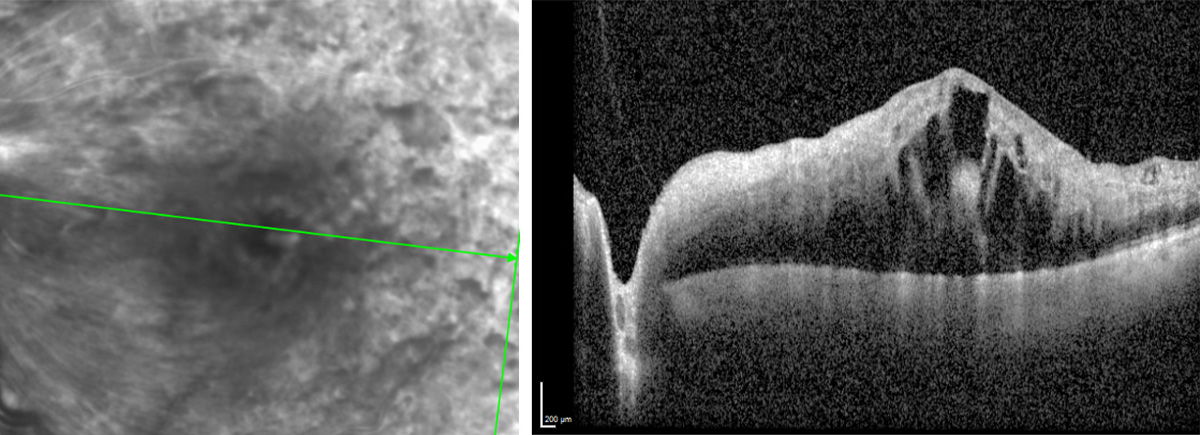
Retinal angiomatous proliferation
 |
| Click image to enlarge. |
In RAP—a form of age-related macular degeneration—abnormal vasculature proliferates from the retinal circulation and progresses posteriorly into the subretinal space.
Suggested reading:
Neovascularization: A Small Solution to a Big Problem
Identifying Conversion to Wet AMD
Commotio retinae
 |
| Photo: University of Iowa. Click image to enlarge. |
Commotio retinae results from blunt trauma, causing transient damage that appears as areas of whitening or opacification.
Suggested reading:
Timing the Retinal Referral: Tips for Success
Choroidal hemangioma
 |
| Photos: Mohammad Rafieetary, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
 |
| Click image to enlarge. |
Choroidal hemangioma are vascular tumors of the choroid that often appear as orange elevated choroidal masses. On IVFA, their most distinguishing characteristic is early lacy hyperfluorescence that continues to leak with time. Other images using OCT and fundus autofluorescence demonstrate additional details.
Suggested reading:
CHRPE
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
CHRPE are congenital benign lesions of the RPE. They are often darkly pigmented, but can develop white window defects called lacunae. With time they can become entirely depigmented. These lesions are flat on clinical examination and do not disappear with a green filter. FAF and OCT can be very useful to confirm a lesion is a CHRPE. On FAF, CHRPE will be well demarcated and entirely hypoautofluorescent. On OCT, CHRPE will be flat lesions of the RPE. The RPE in pigmented lesions will often be slightly hyperreflective and thick. In depigmented lesions, the RPE may be thinning with increased light transmission into the choroid. The outer retina overlying CHRPE is atrophic and thinned.
Suggested reading:
Timing the Retinal Referral: Tips for Success
Choroidal nevus
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Choroidal nevi are benign tumors of the choroid. They typically present as pigmented lesions and may have overlying drusen deposits. Adjunct testing may be helpful to confirm the diagnosis of choroidal nevus such as FAF and OCT.
The patient in the first set of images presents with a small, flat, choroidal nevus adjacent to the optic nerve. On OCT, choroidal nevi can have varying levels of hyperreflectivity and can also have some level of thickness, but it will be noted that the lesion exists in the choroid. This particular lesion on OCT is flat with hyperreflectivity in the choriocapillaris and posterior shadowing. OCT is also helpful to rule out presence of subretinal fluid--a bad sign that could indicate choroidal melanoma. On FAF, choroidal nevi may be invisible, as is the case here, or may have some mild mottled autofluoresence. On clinical examination, use of green filter may be helpful to distinguish choroidal nevi from CHRPE. When a red filter is applied, choroidal nevi will become much less visible or disappear from view, whereas CHRPE will still be visible.
In the second case, the choroidal nevus in question does show some elevation on OCT. Keep in mind that elevation over 2mm is highly concerning for choroidal melanoma. OCT also shows overlying drusen and absence of subretinal fluid—both of which are positive indications that the lesion is a choroidal nevus vs. a more serious choroidal melanoma. Choroidal nevi must be monitored, however, for they have risk to convert to choroidal melanoma.
Suggested reading:
Mnemonic Helps Catch Small Choroidal Melanoma Early
Choroidal Melanoma is a Life Sentence
Choroidal melanoma
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
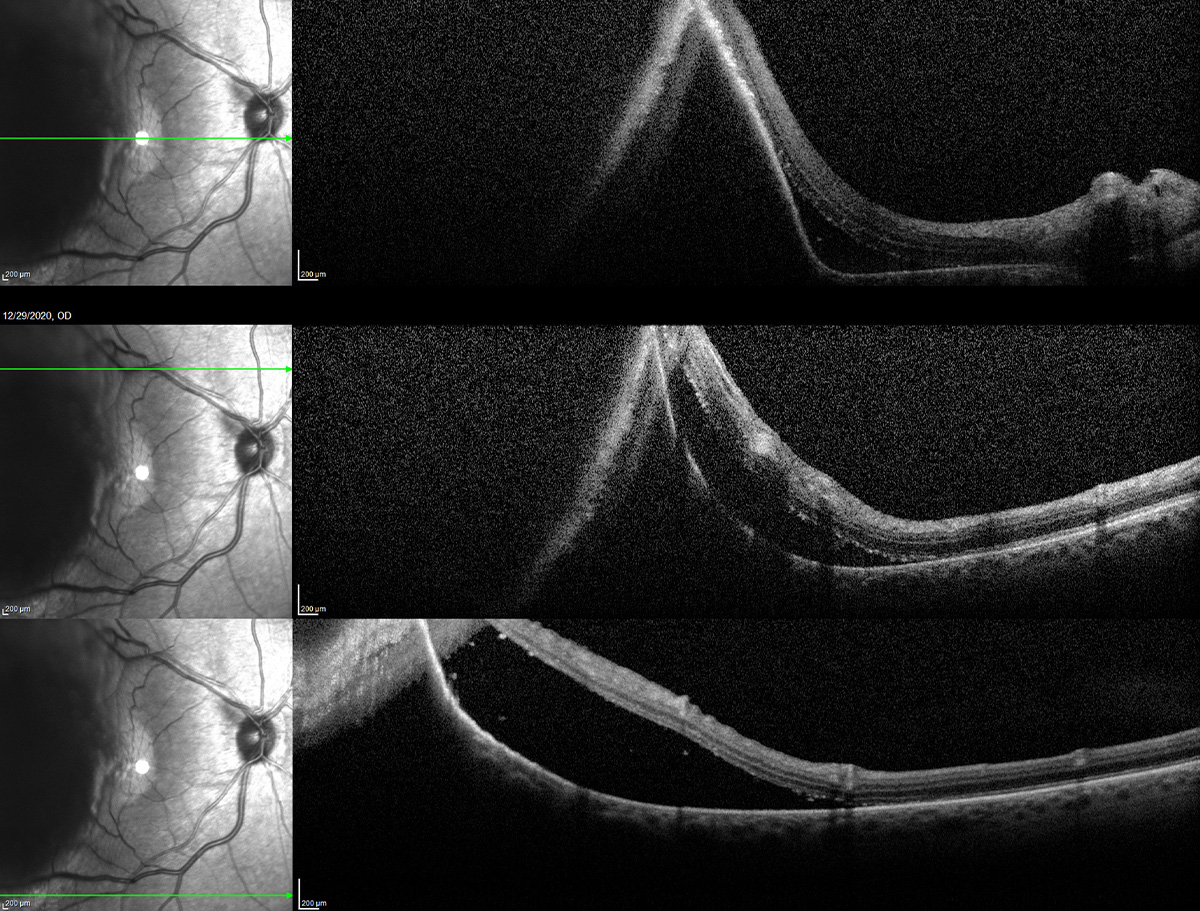 |
| Click image to enlarge. |
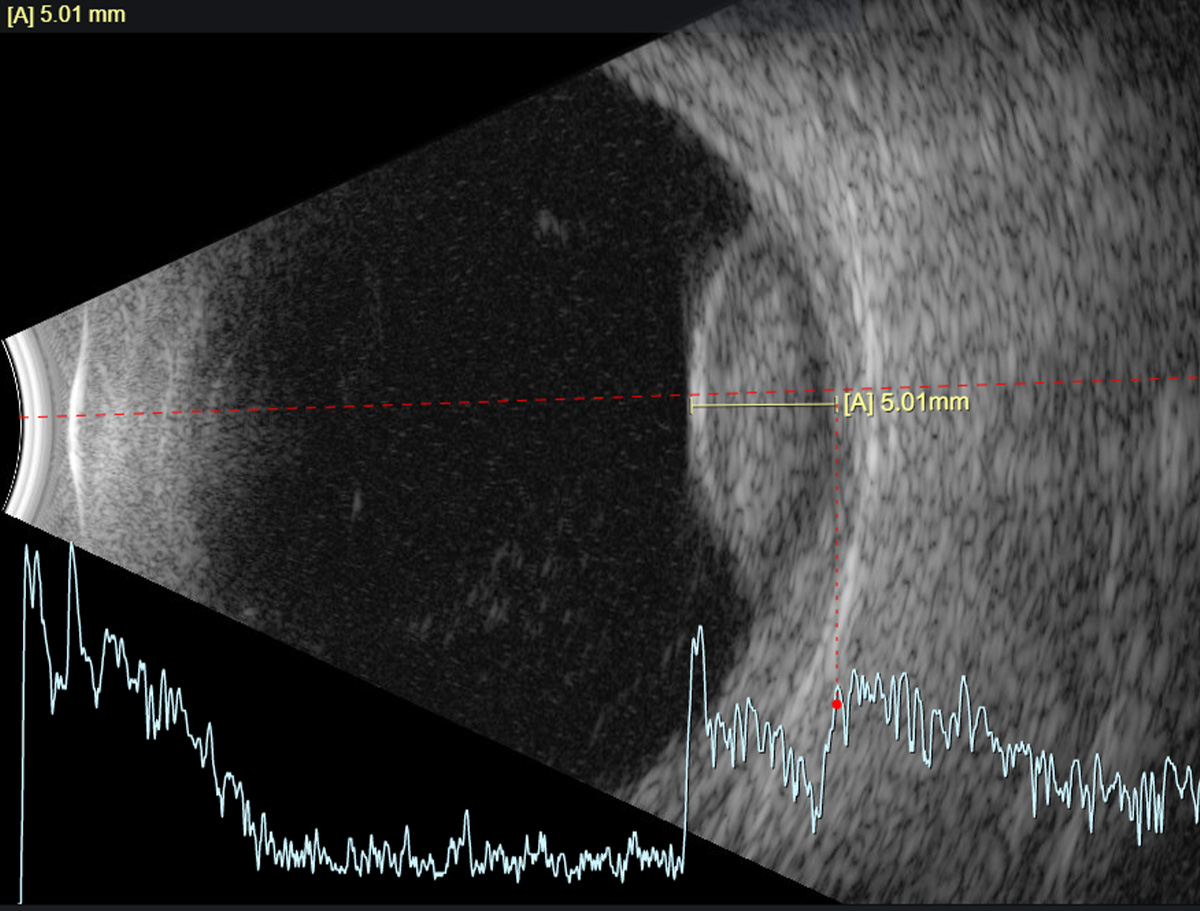 |
| Click image to enlarge. |
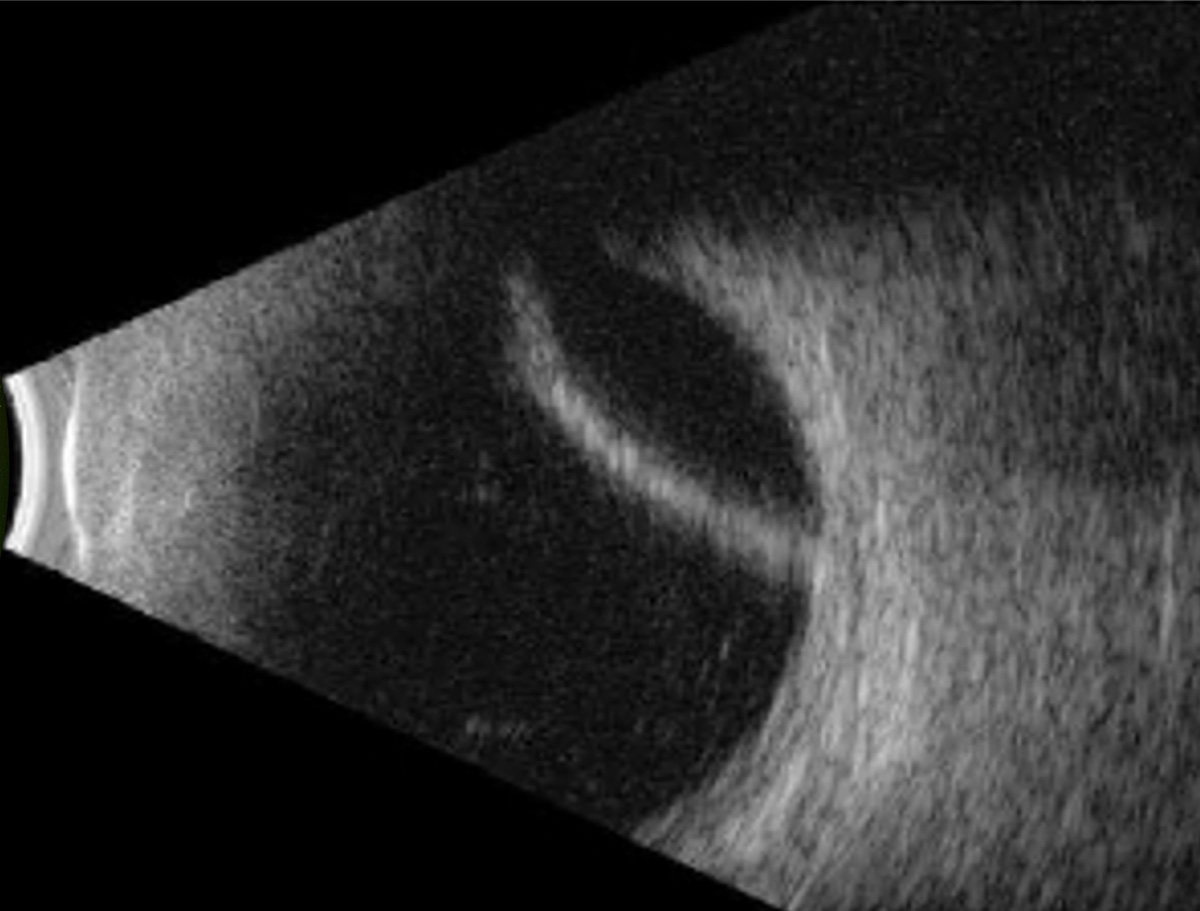
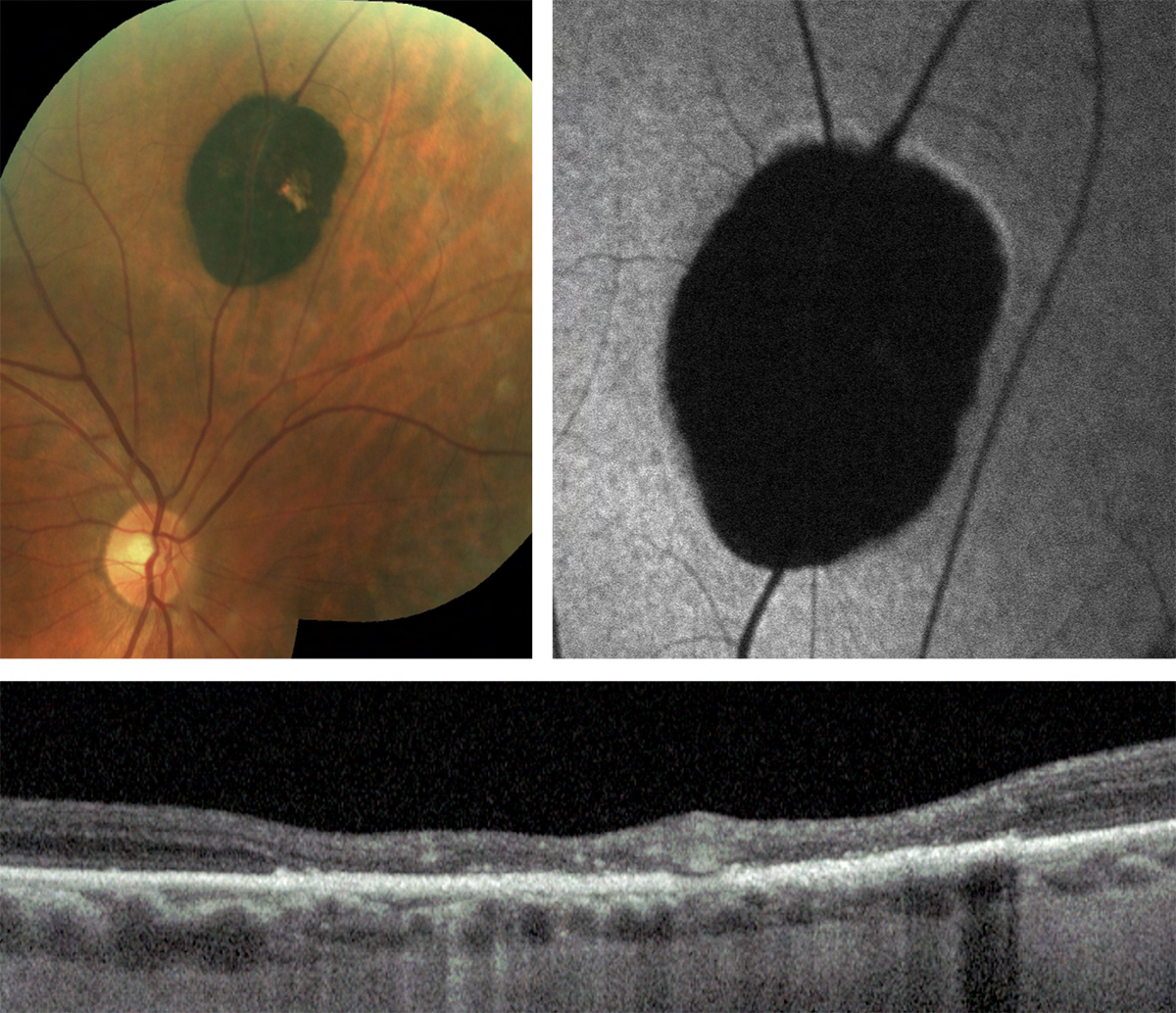
This choroidal melanoma presents as an elevated choroidal lesion with overlying orange pigment. A dilated examination with good stereopsis is helpful in determining elevation of the lesion. Additional testing such as OCT, B-scan and FAF can help to identify additional factors that differentiate a lesion such as this from a choroidal nevus.
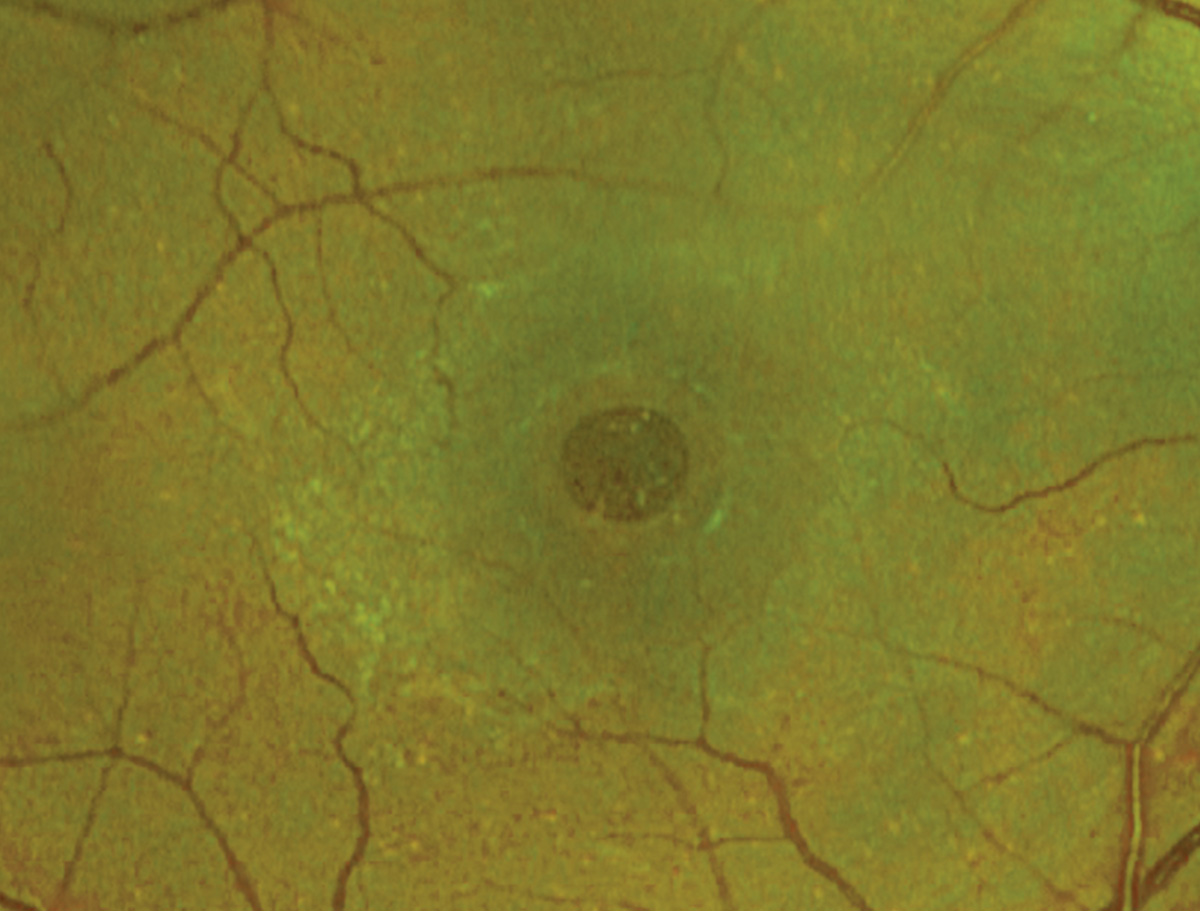
Fundus autofluorescence of choroidal melanoma demonstrates presence of overlying lipofuscin with patchy areas of hyperautofluoresence. Lipofuscin presents clinically as orange pigment and is a risk factor for presence of choroidal melanoma.
The last image shows the melanoma on B-scan ultrasound, measuring over 5mm thick with ultrasonographic hollowness. Thickness over 2mm is a risk that a lesion is in fact a choroidal melanoma, as is the finding of ultrasonographic hollowness.
Suggested reading:
Choroidal Melanoma is a Life Sentence
Multimodal Imaging of Choroidal Melanoma with Submacular Fluid
Mnemonic Helps Catch Small Choroidal Melanoma Early
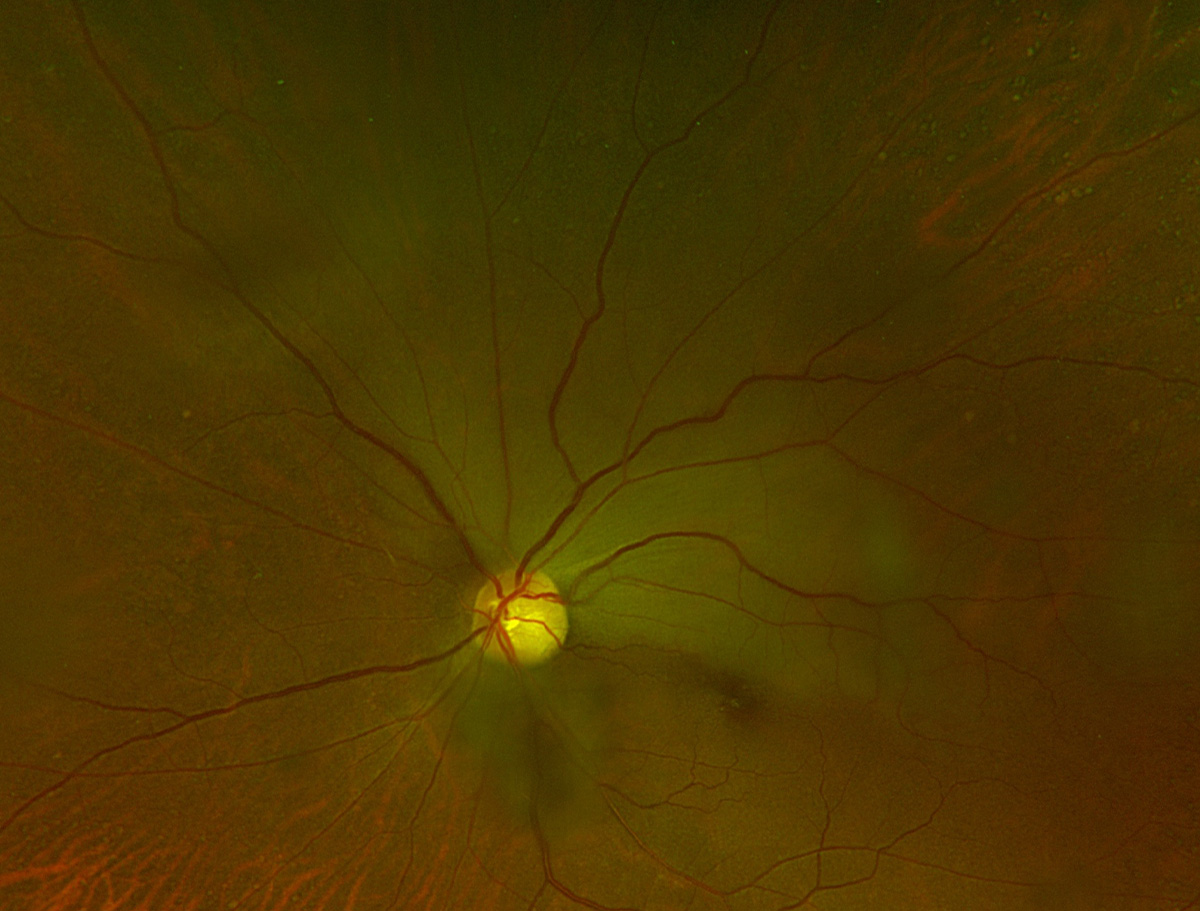
Vogt-Koyanagi-Harada syndrome
 |
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Vogt-Koyanagi-Harada syndrome is a rare granulomatous autoimmune disease and a cause of noninfectious uveitis.
In the first set of images, the fundus photo shows bilateral multifocal serous retinal detachments, hyperemic optic nerve and mild optic nerve edema. The OCT shows a bacillary layer detachment (detachment of the photoreceptor layer) as well as subretinal fluid representing neurosensory detachment.
In the second set of images, the fundus appearance is comparable to the first eye while the OCT shows more extensive bacillary layer detachment involving the fovea with eccentric subretinal fluid.
Suggested reading:
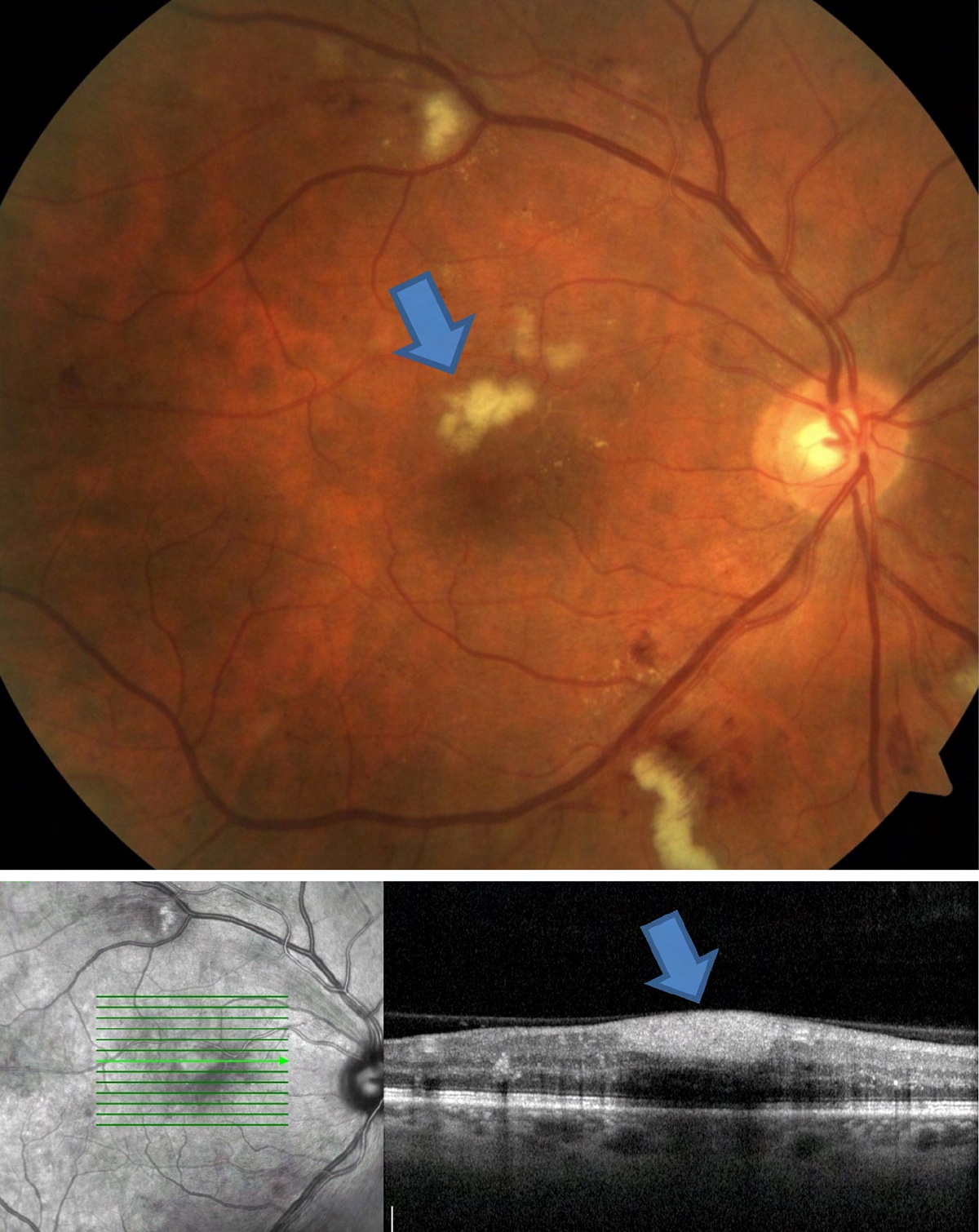
Cotton wool spots
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Cotton wool spots are small infarcts of the superficial vascular plexus that can occur in a wide variety of conditions. They appear as superficial, white, fluffy lesions that may appear elevated. The blue arrow pointing towards a cotton wool spot in a patient with diabetic retinopathy. OCT through the lesion may be helpful in confirming the finding. Here, the accompanying OCT shows area of thickened retinal nerve fiber layer—the layer affected in a cotton wool spot.
Suggested reading:
Can You Spot These Retinal Vascular Abnormalities?
Hematological Disorders and the Retina
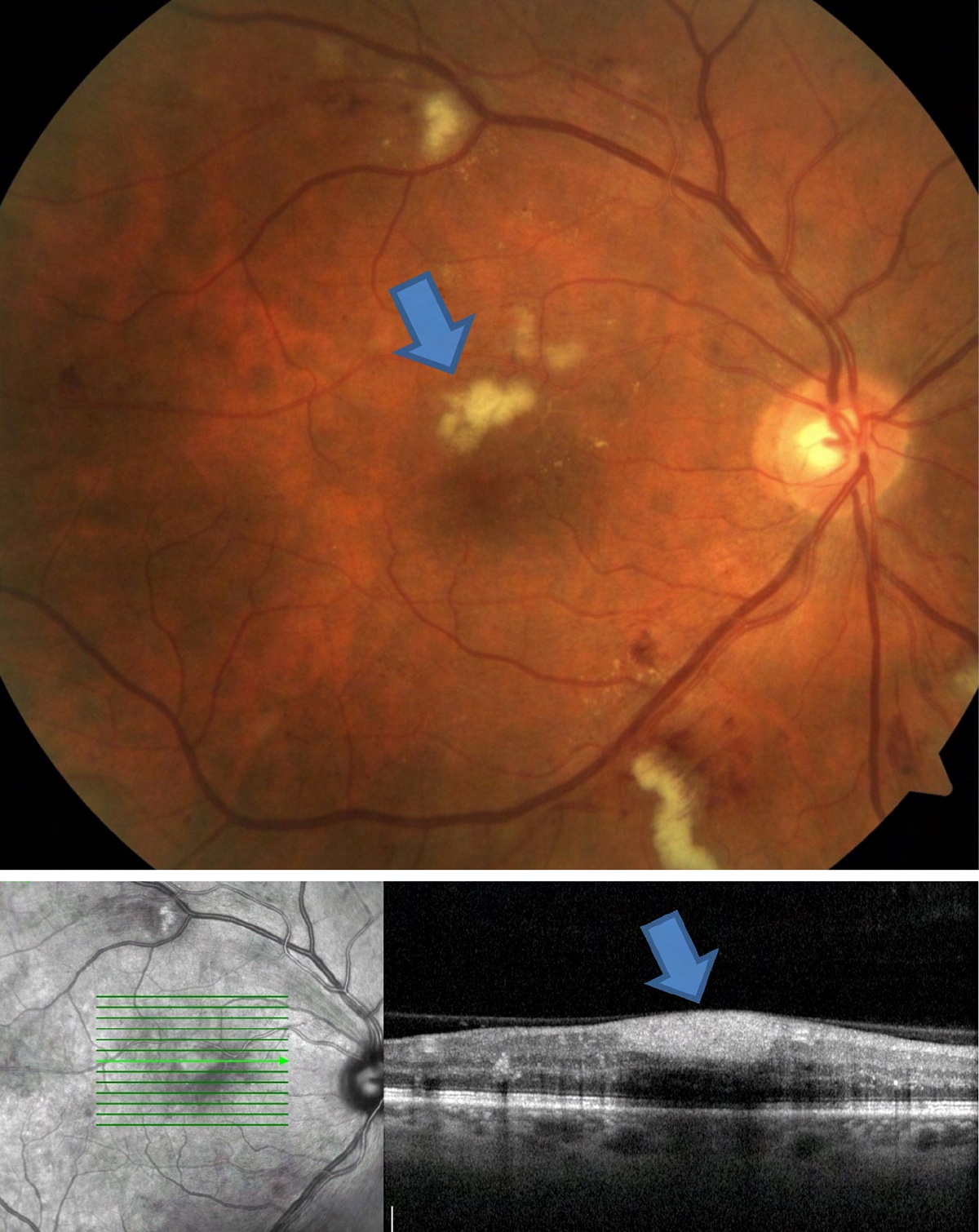
Central retinal vein occlusion
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
CRVO presents with 360° tortuous retinal veins and hemorrhages (first image); however, there can be various levels of hemorrhaging present. Additional complications include macular edema, retinal neovascularization and iris neovascularization.
The second image shows macular edema secondary to CRVO on OCT, with macular thickening, intraretinal fluid and subretinal fluid. Macular edema is a common complication of retinal vein occlusions that can lead to decreased visual acuity. On clinical examination, good stereopsis may help to reveal the macular thickening.
Suggested reading:
Branch retinal vein occlusion
 |
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
BRVO with sectoral intraretinal hemorrhaging and cotton wool spots inferotemporally. Clinical exam clues to pay attention to are the arteriovenous nicking, venous dilation and venous tortuosity. While more common in CRVO, it is still important to monitor for NVD or NVE in patients with BRVO.
Suggested reading:
BRVO Presentation Differs in Black Patients
Central retinal artery occlusion
 |
| Photo: Rami Aboumourad, OD. Click image to enlarge. |
Acute CRAO with diffuse macular whitening with central red spot (i.e., cherry red spot). The fovea remains perfused by the underlying choriocapillaris and is surrounded by ischemic (white) retina. It is important to inquire regarding symptoms of giant cell arteritis when no embolus is found.
Suggested reading:
Stroke of the Eye: Are You Prepared?
Can You Spot These Retinal Vascular Abnormalities?
Middle Maculopathy May Precede CRAO
How to Triage Non-Traumatic Ocular Emergencies
Branch retinal artery occlusion
 |
| Photo: Rami Aboumourad, OD. Click image to enlarge. |
Acute BRAO with sectoral retinal whitening of the superotemporal quadrant. No embolus is visible on clinical exam.
Suggested reading:
Stroke of the Eye: Are You Prepared?
Can You Spot These Retinal Vascular Abnormalities?
Cystoid macular edema
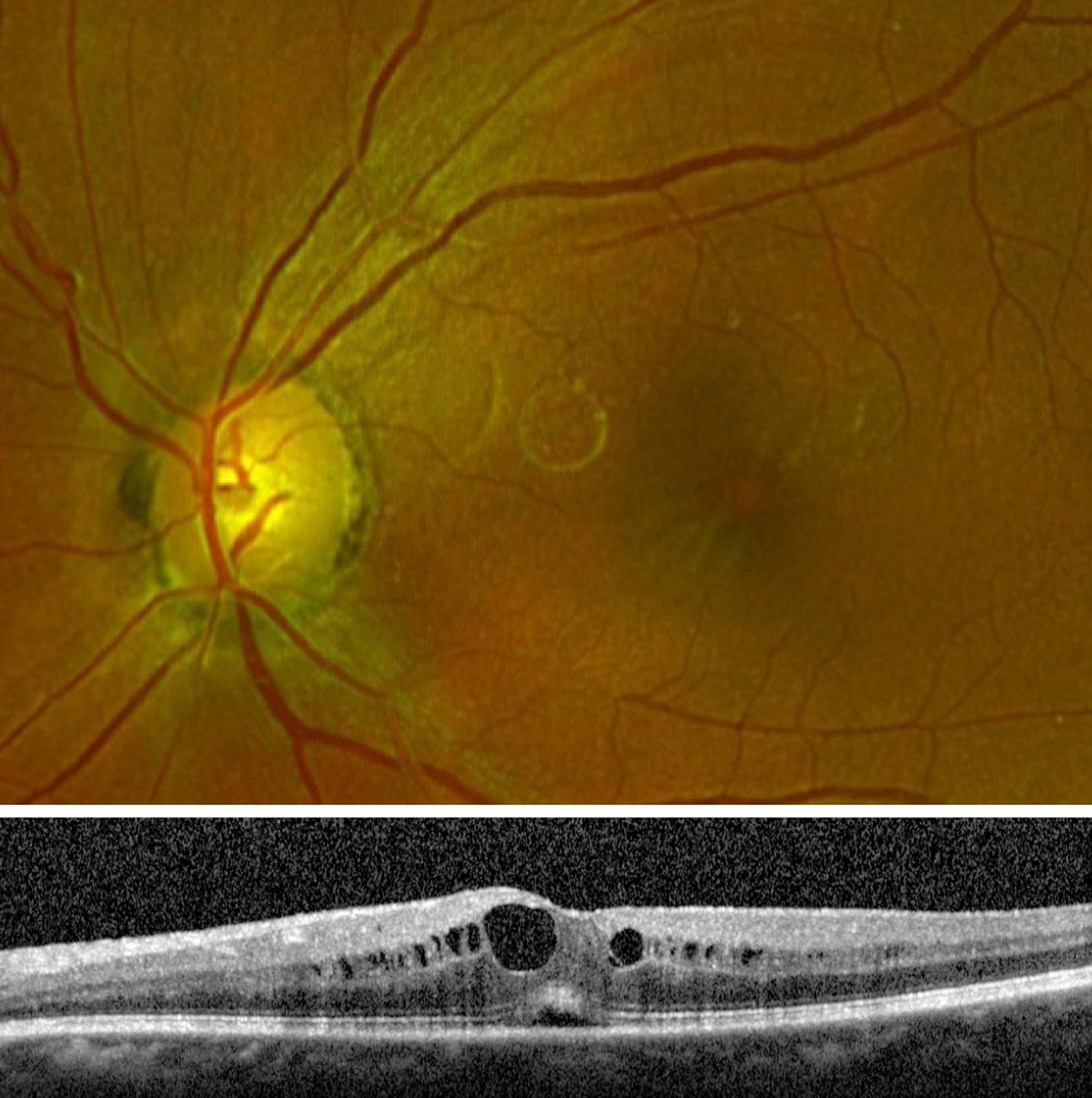 |
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
Fundus photo of CME showing a thickened and somewhat striated appearance to the macula. The OCT shows fluid-filled intraretinal cysts and subretinal fluid.
Suggested reading:
Jury Still Out on Best Treatment for Post-cataract CME
Epiretinal membrane
 |
| Photos: Jessica Haynes, OD; Rami Aboumourad, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Epiretinal membranes may be visualized clinically as yellow glistening on the macular surface (first image, top). On clinical examination they may be confused with drusen or exudate, but their more superficial and glistening look helps to distinguish them. On OCT (first image, bottom), the ERM itself will present as a hyper-reflective band that sits on the surface of the ILM. As this band contracts it can create differing degrees of irregularity to the macular surface by creating foveal inversion (loss of foveal pit), irregularity of the foveal pit, retinal striations, and macular thickening. This patient has mild macular striations and flattening of the foveal pit from presence of the ERM.
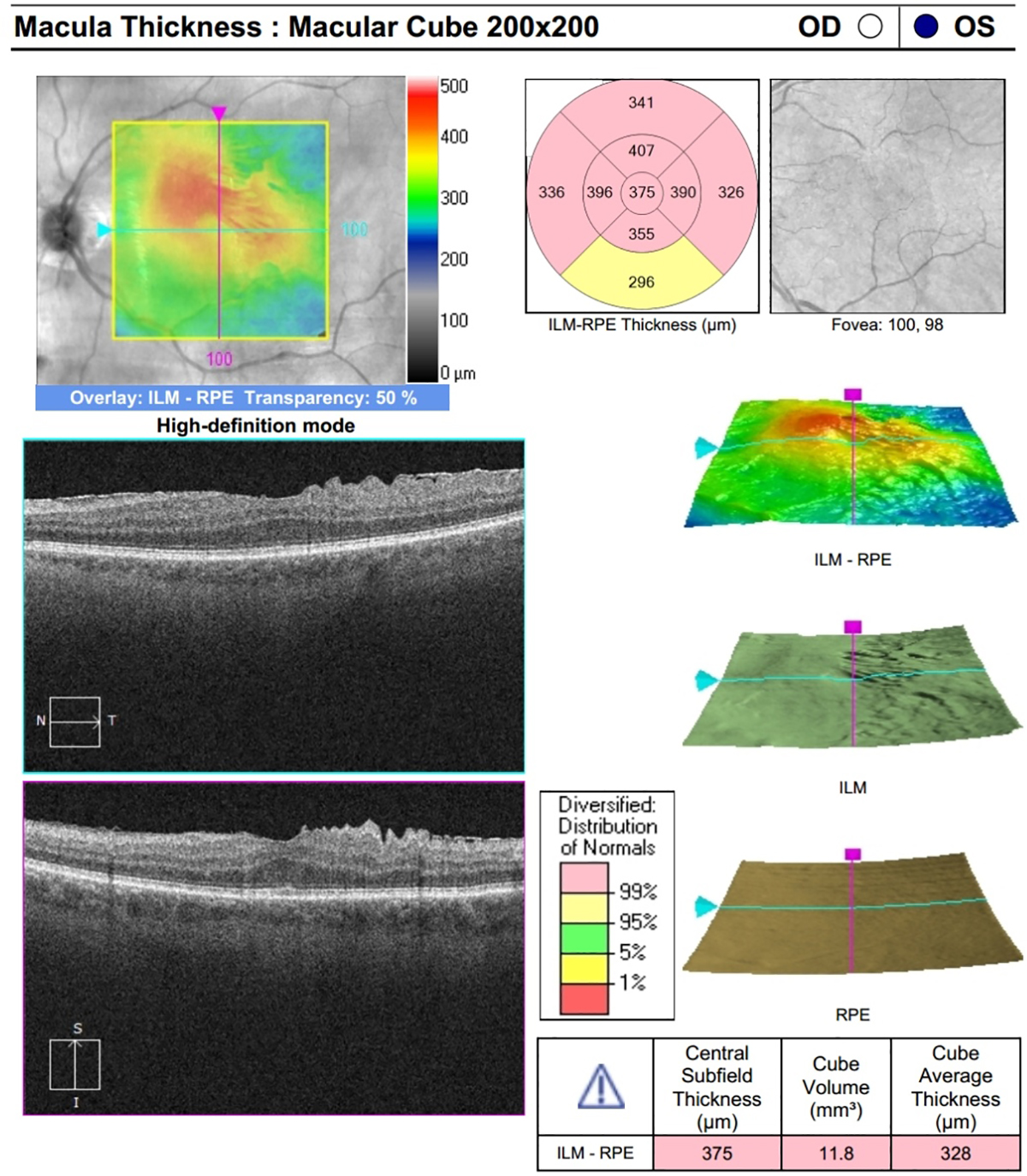
The second image is a Cirrus OCT of an ERM that shows the presence of a pre-retinal hyperreflective membrane inducing retinal traction and alteration of typical foveal architecture. The macular thickness map is particularly helpful for monitoring these patients over time.
Suggested reading:
Timing the Retinal Referral: Tips for Success
Hypertensive retinopathy
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Stage 4 hypertensive retinopathy can present with bilateral disc edema, hemorrhages, cotton wool spots and exudates. It is imperative to identify this ocular emergency by checking the patient’s blood pressure. This presentation accompanied by a severely elevated BP requires referral to a nearby emergency department.
Suggested reading:
How Hypertension and Stroke Affect the Eye
Managing Patients With Hypertensive Crisis
Panuveitis
 |
| Photo: Alison Bozung, OD. Click image to enlarge. |
Sarcoidosis-associated panuveitis may present, as in this case, with scattered yellow lesions and vitritis. Indocyanine green angiography is helpful to assess choroidal involvement, seen here as scattered hypocyanescent lesions more numerous than those seen on the dilated fundus exam.
Suggested reading:
Systemic Disease Rising to the Surface
Intraretinal microvascular abnormalities
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
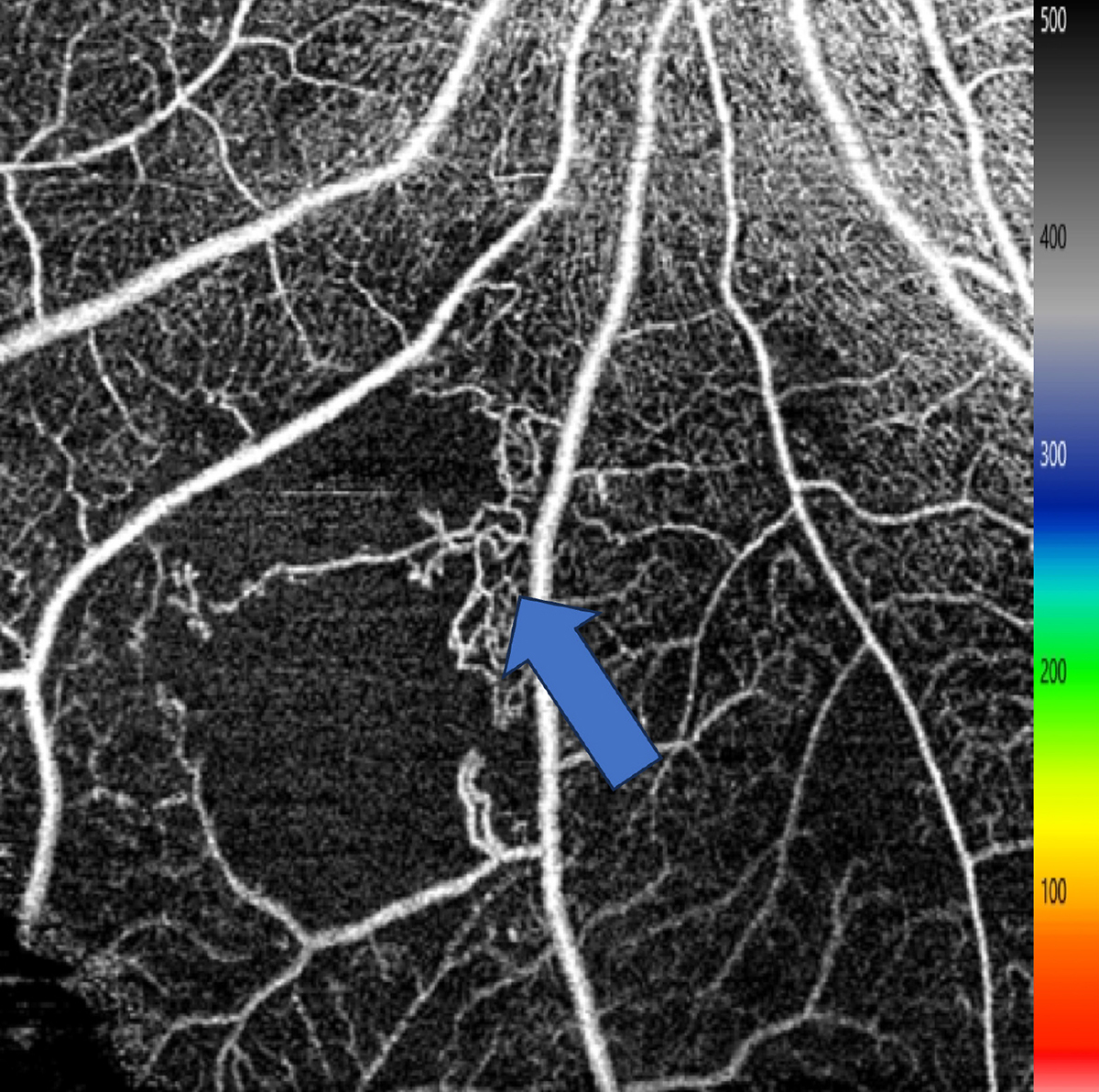 |
| Click image to enlarge. |
IRMA are small telangiectatic vessels that form from damaged capillary beds. Prominent IRMA in one quadrant meets the 4-2-1 criteria for severe NPDR. Careful evaluation is necessary to identify IRMA, as it is very easy to overlook. It can be difficult to distinguish IRMA from NVE. OCT-A may be helpful to distinguish IRMA from NVE, as IRMA will be present in the superficial or deep capillary plexi while NVE will be present on the vitreoretinal interface. In addition, intravenous fluorescein angiography can be used as IRMA typically does not leak while NVE does.
Suggested reading:
Staging of Diabetes and Diabetic Retinopathy
My Patient Has Diabetic Retinopathy...Now What?
Larger OCT-A Scans Reveal Impaired Retinal Vascular Integrity in DME Eye
Diabetes Care in the Age of Anti-VEGF
UWF Imaging Earns Good Marks in Detecting Early DR
Venous beading
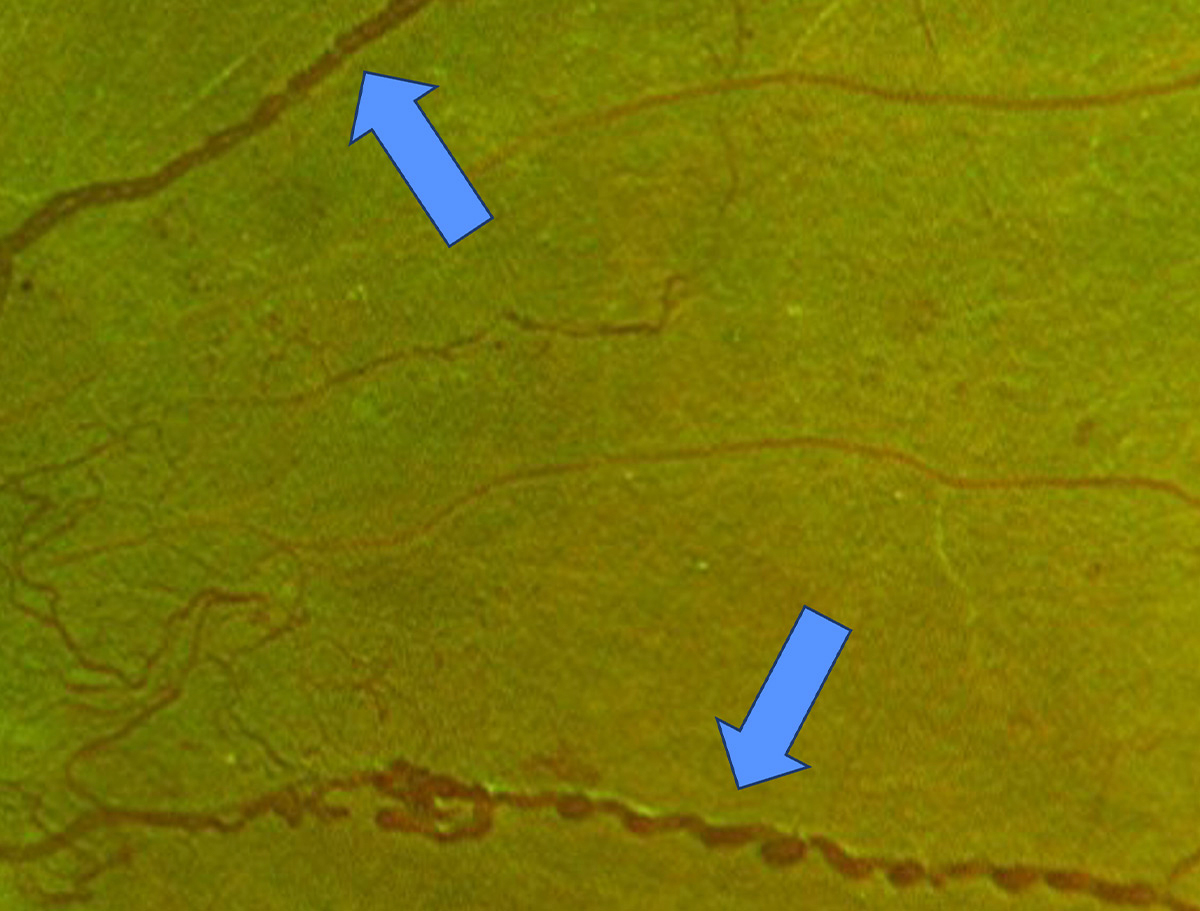 |
| Photo: Jessica Haynes, OD. Click image to enlarge. |
Venous beading is shown with blue arrows. Venous beading in two quadrants meets the criteria for the 4-2-1 rule for severe NPDR. This patient also has NVE, which constitutes PDR.
Suggested reading:
My Patient Has Diabetic Retinopathy...Now What?
Staging of Diabetes and Diabetic Retinopathy
Can You Spot These Retinal Vascular Abnormalities?
Recognizing Abnormal Vasculature
Nonproliferative diabetic retinopathy
 |
| Photo: Rami Aboumourad, OD. Click image to enlarge. |
A case of severe NPDR OS. Exam discloses significant dot-blot hemorrhaging in all four quadrants, venous beading along the superior and inferior temporal arcades, and multifocal IRMA in all quadrants (most prominent in the photo inferior and inferonasal to the optic nerve).
Suggested reading:
My Patient Has Diabetic Retinopathy...Now What?
Staging of Diabetes and Diabetic Retinopathy
Reconsider Your Approach to Diabetic Retinopathy
Diabetic Retinopathy by the Numbers
DR: See Something? Say Something
Nearly 10 Million Americans Have Diabetic Retinopathy
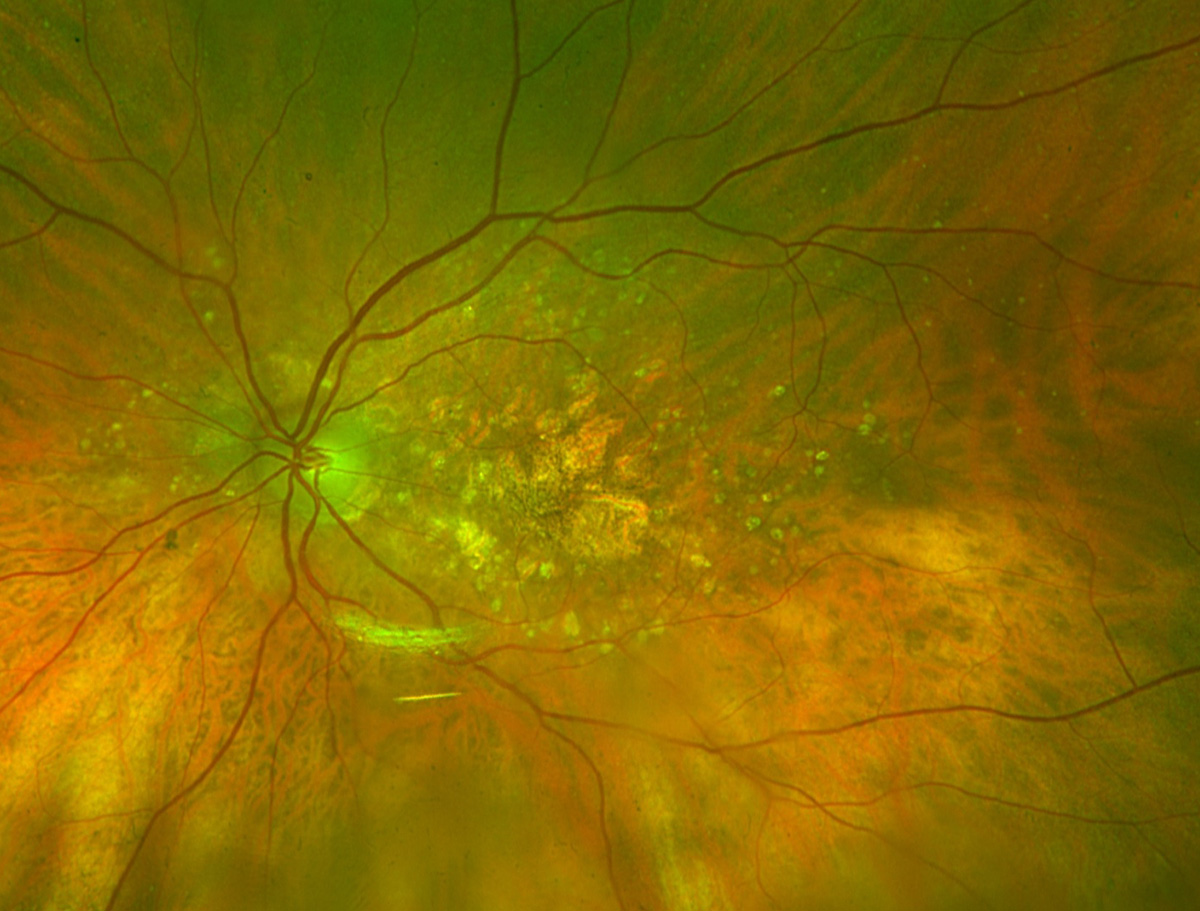
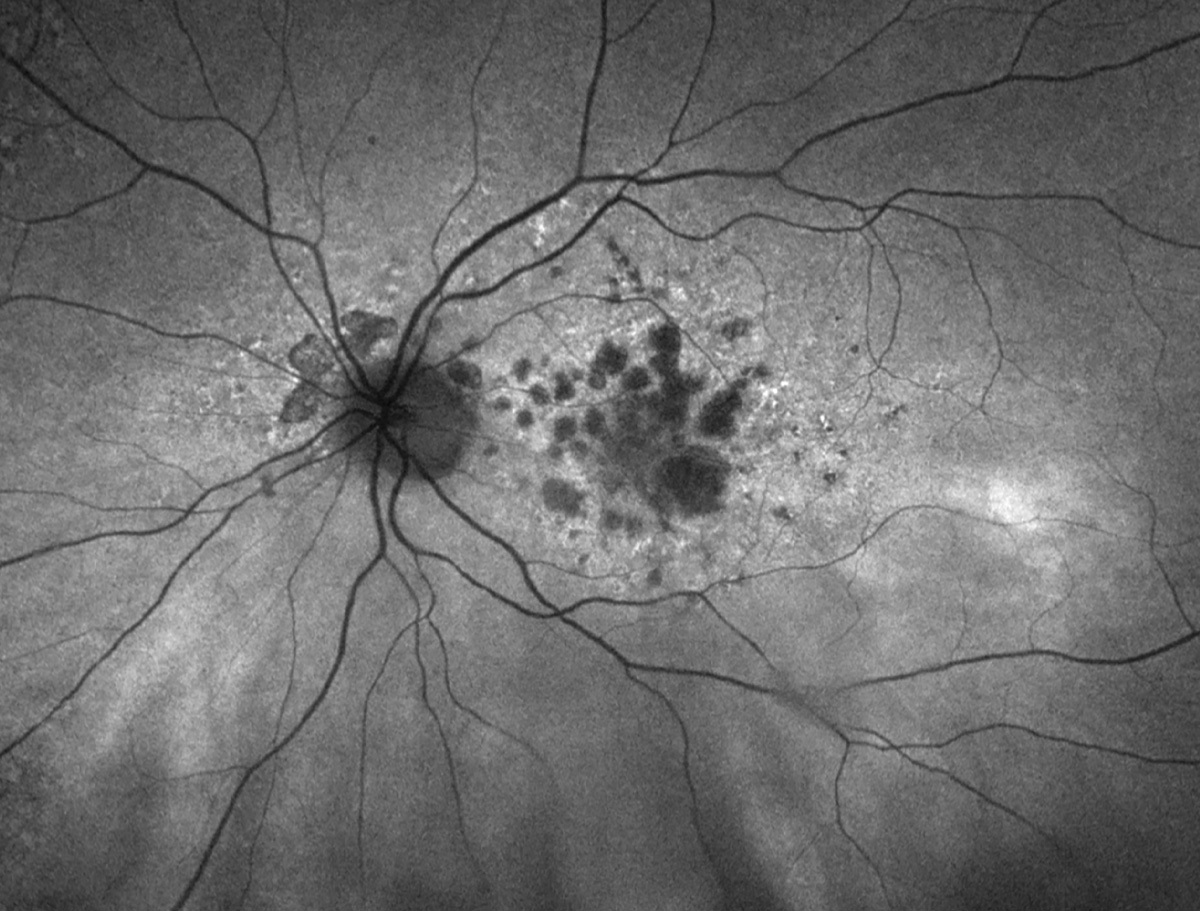
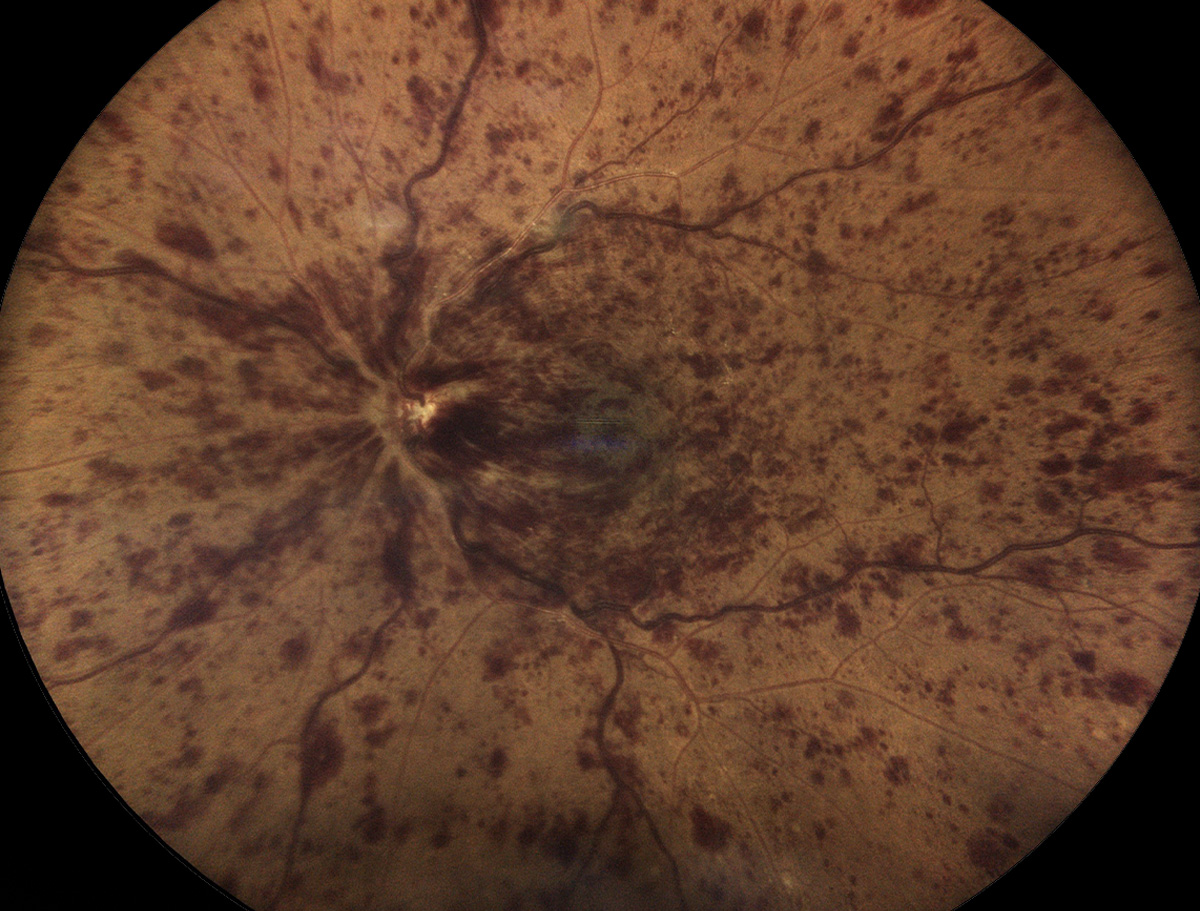
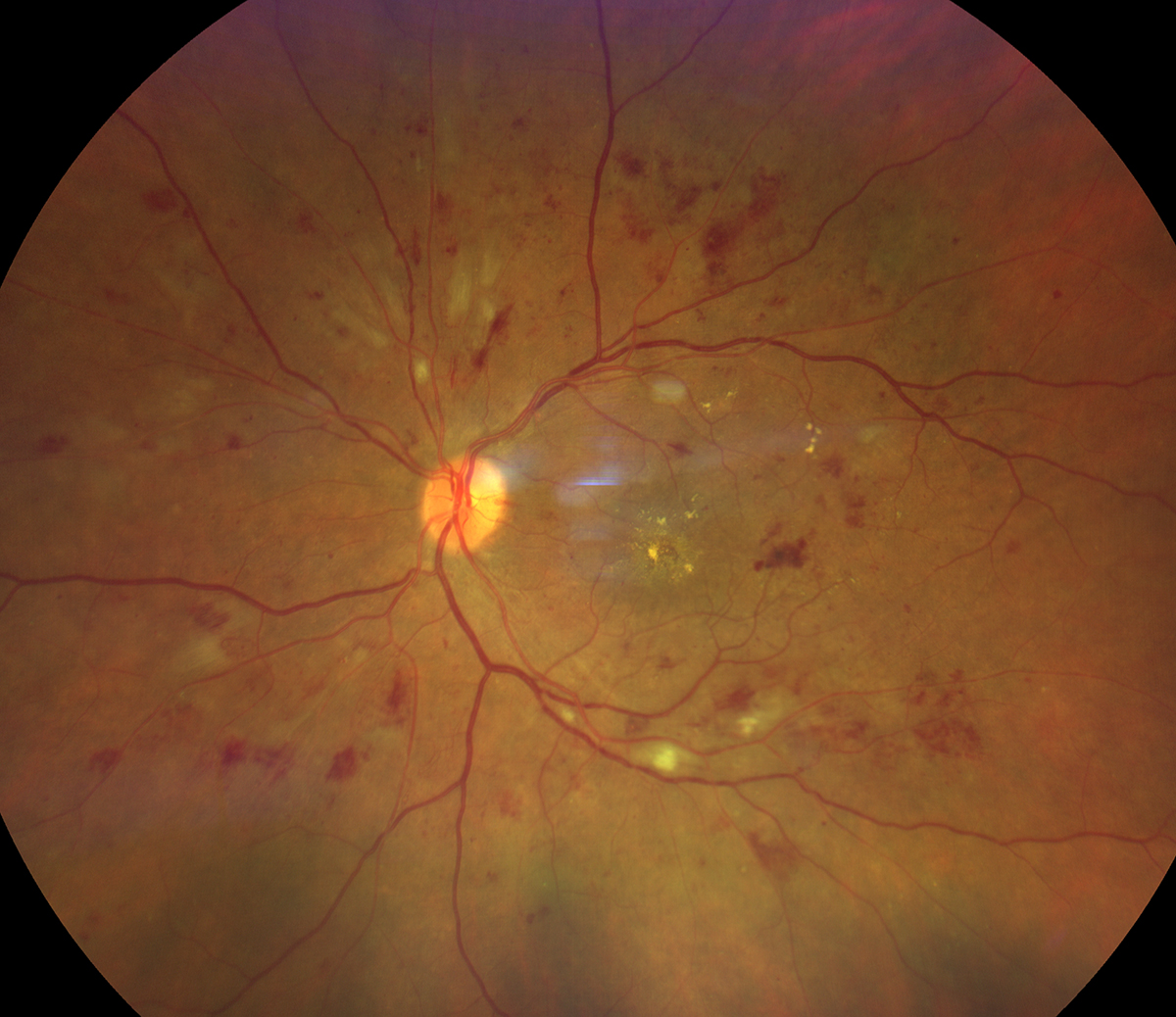
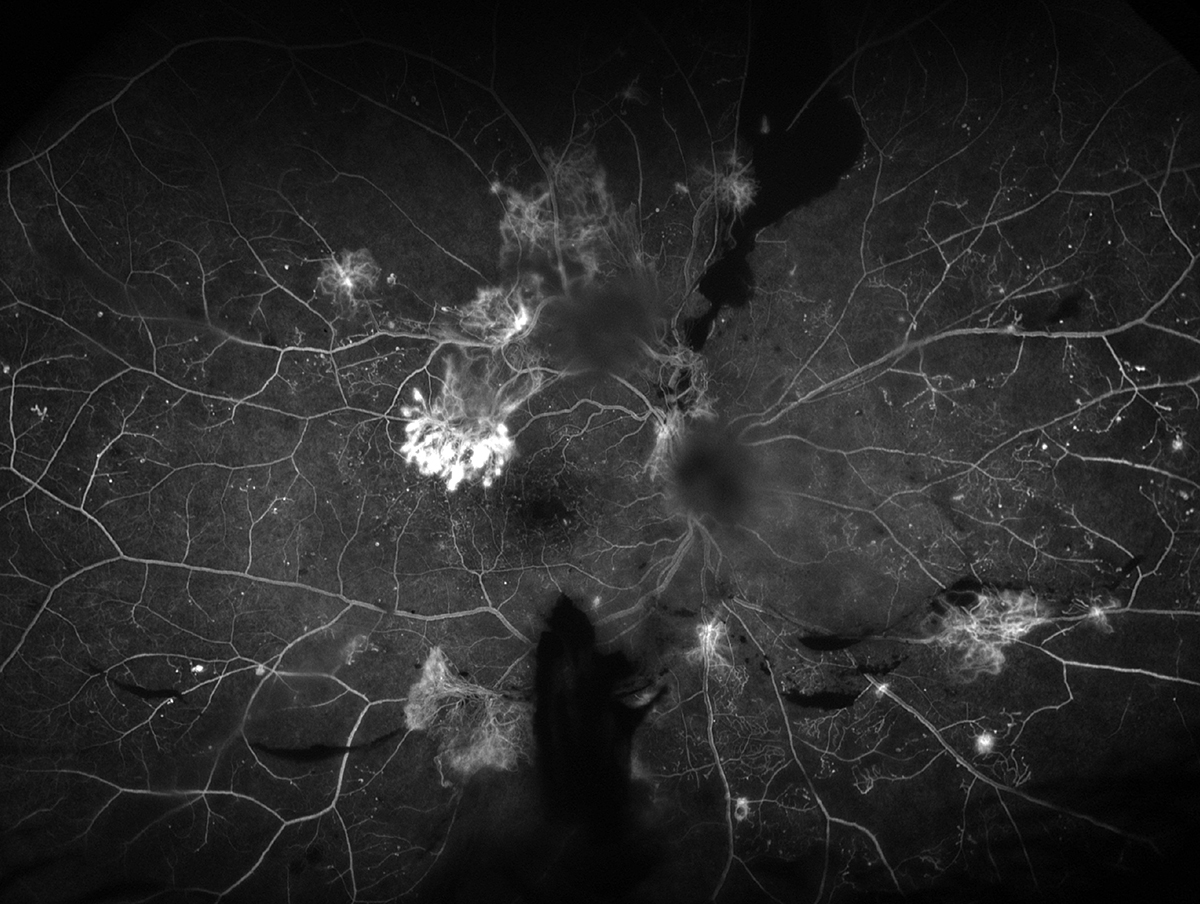
Proliferative diabetic retinopathy
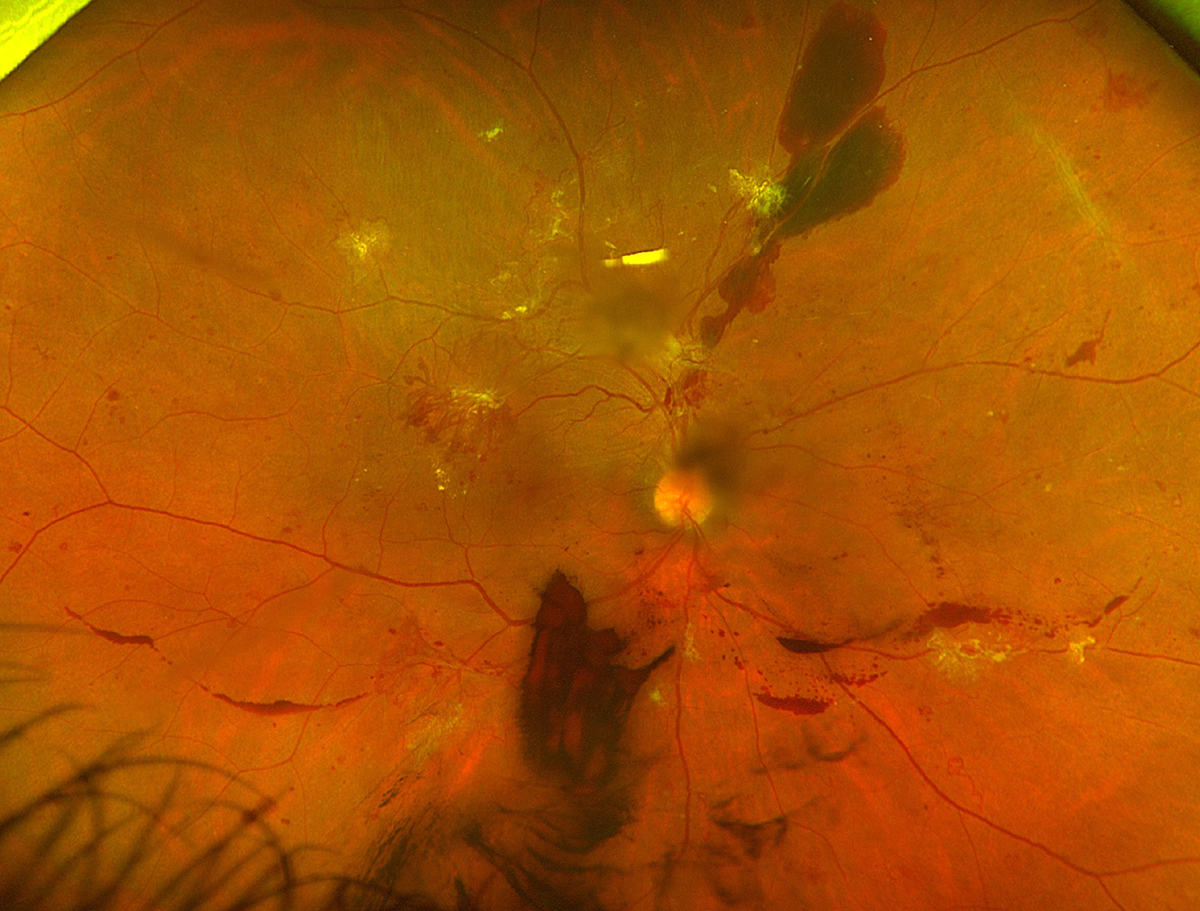 |
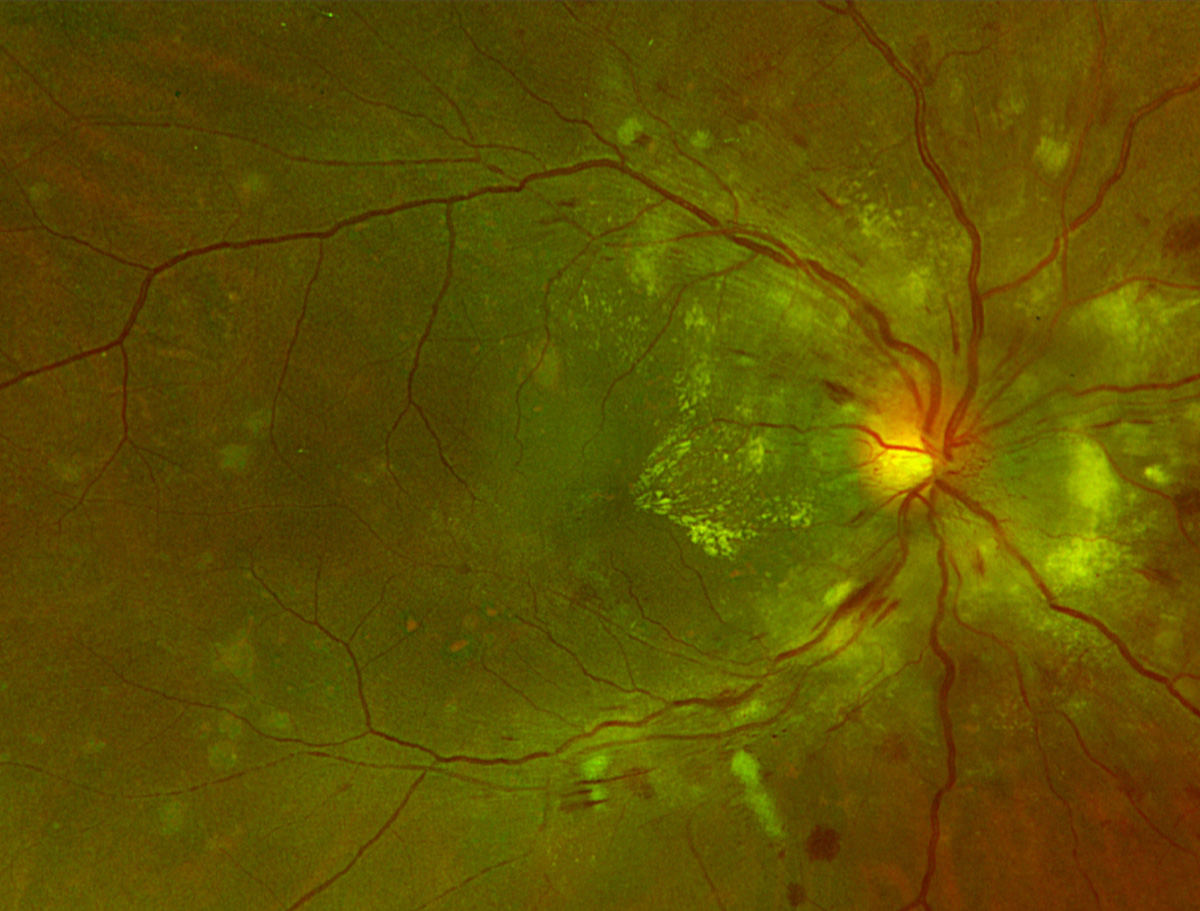
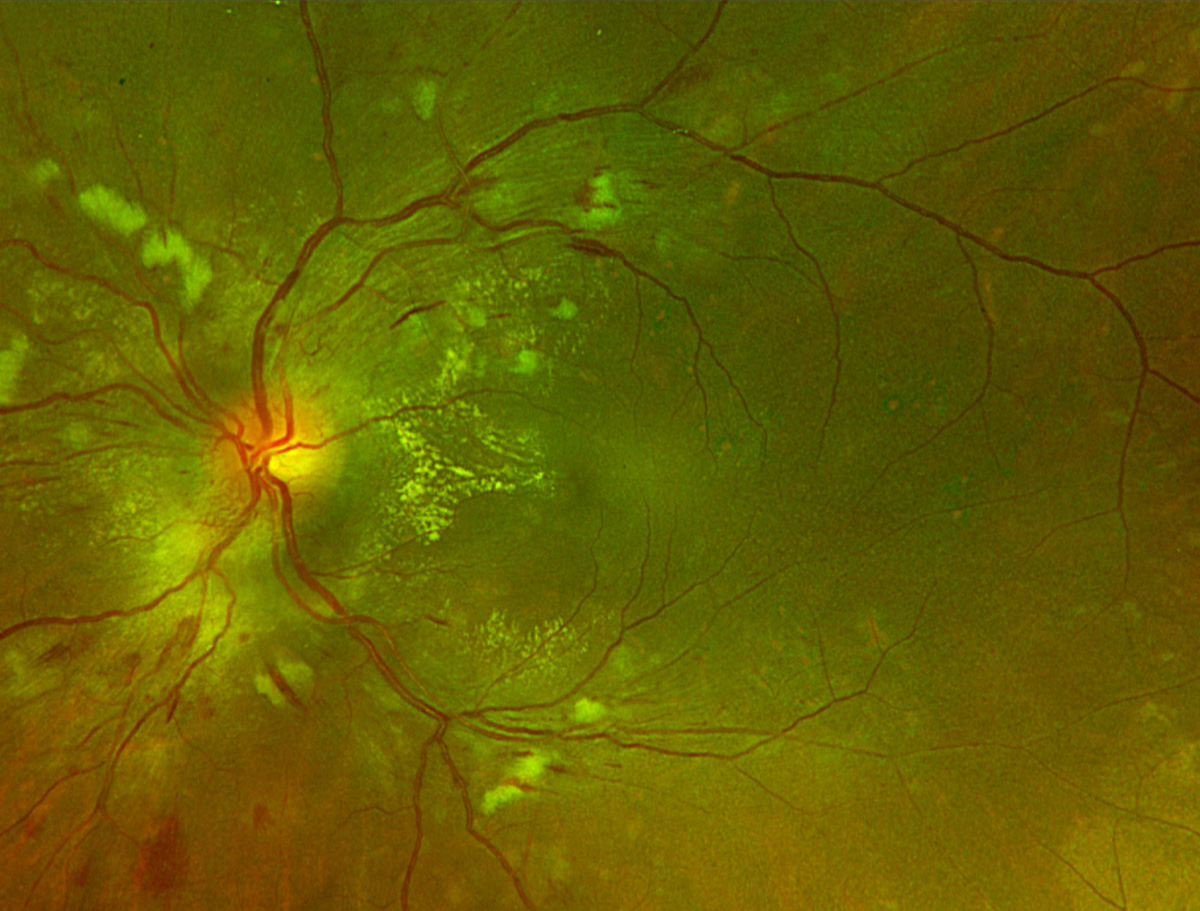
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
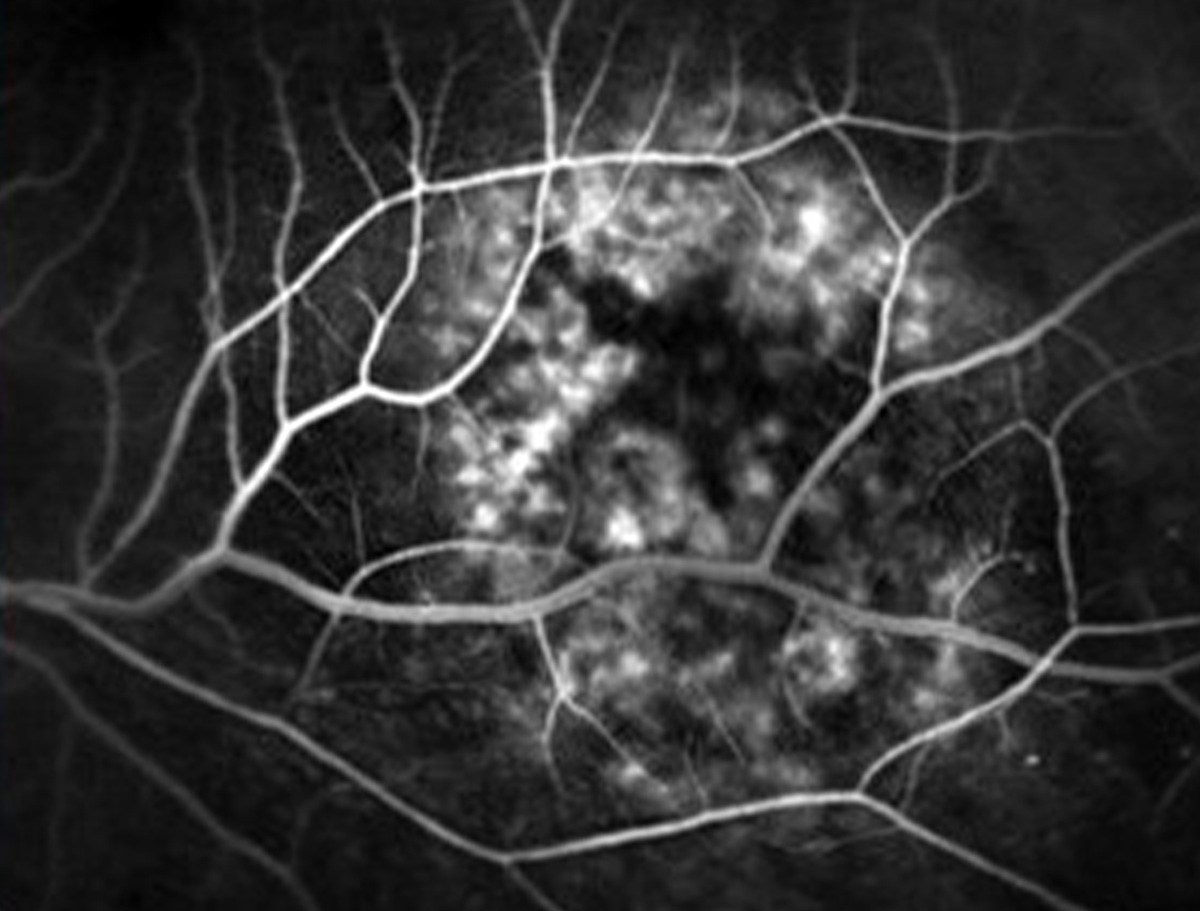
The fundus photo shows PDR in a patient with vitreous, preretinal and intraretinal hemorrhaging with multifocal fronds of retinal neovascularization. The fluorescein angiogram of the same patient shows multifocal leakage (consistent with neovascularization), IRMA, microaneurysms and peripheral capillary nonperfusion inferonasally.
Suggested reading:
My Patient Has Diabetic Retinopathy...Now What?
Diabetic Retinopathy by the Numbers
Reconsider Your Approach to Diabetic Retinopathy
Type 1 Diabetes, Longer Disease Duration, Comorbidities Associated with PDR
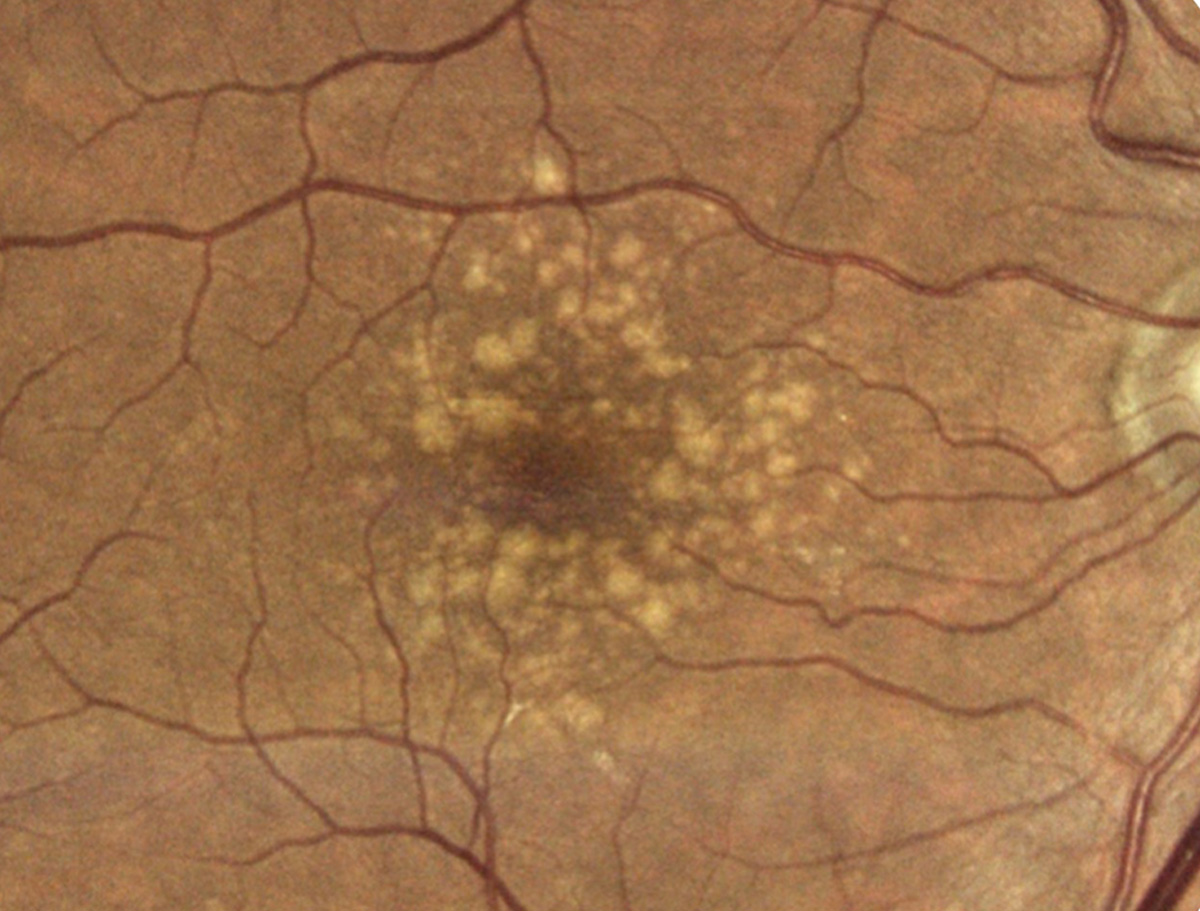
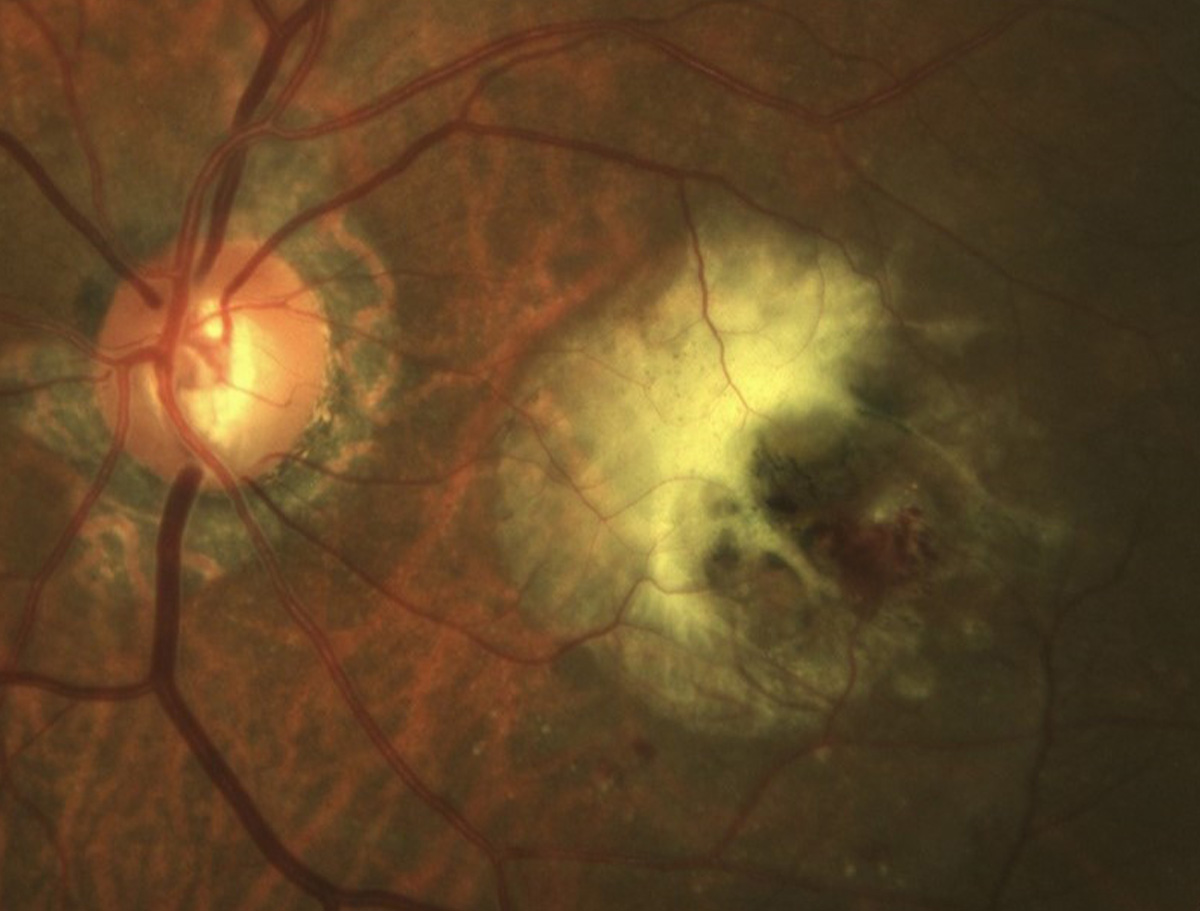
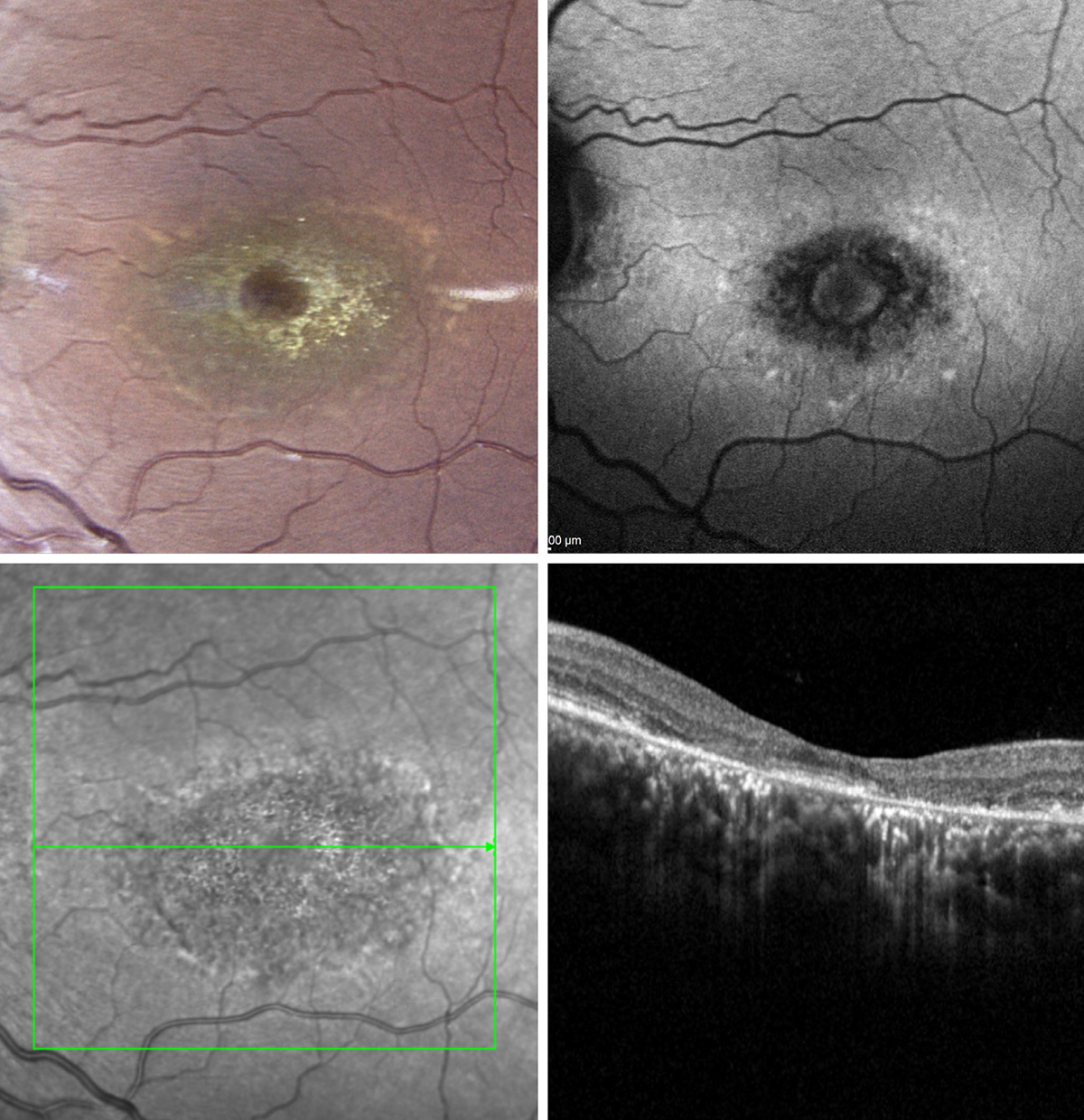
Stargardt's disease
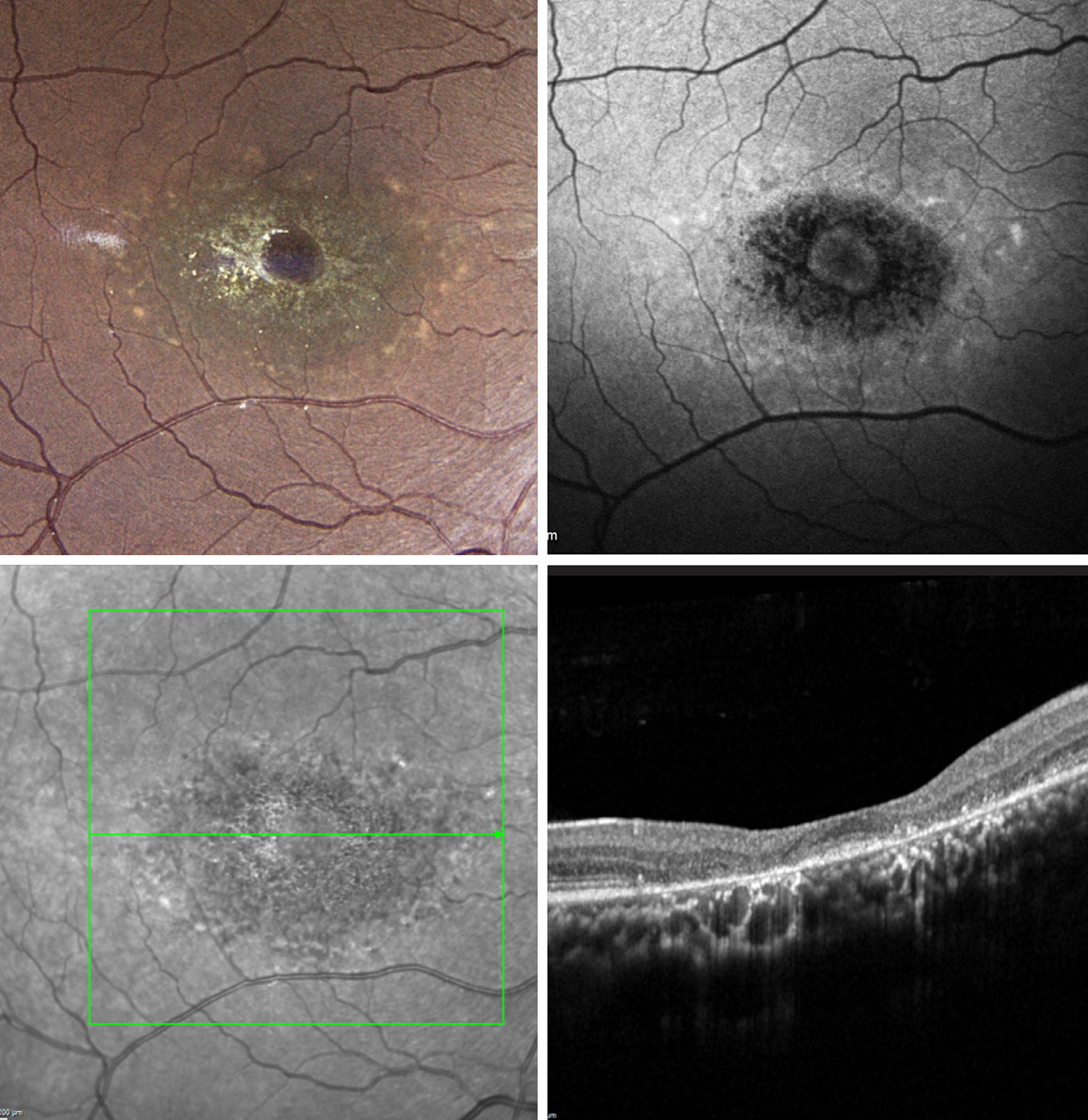 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
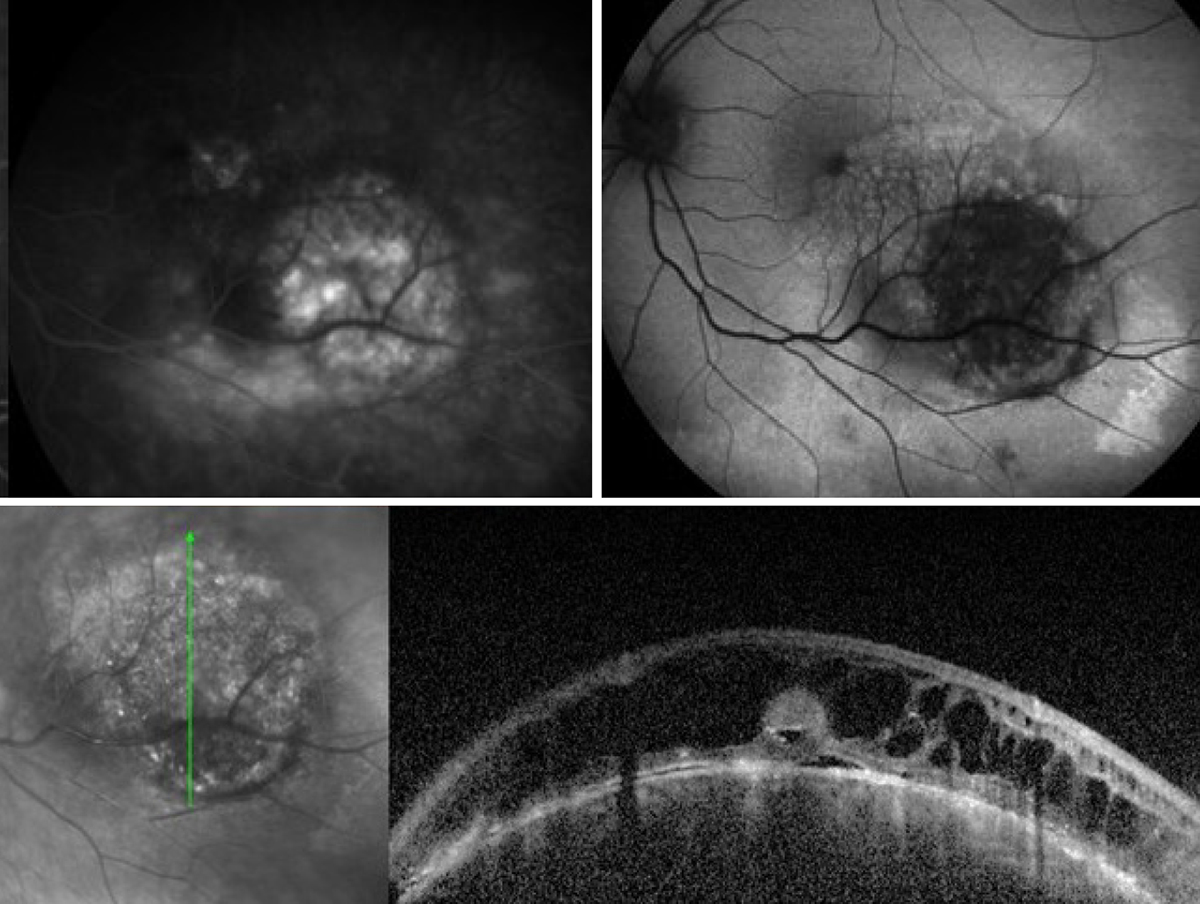
Stargardt's is the most common inherited macular dystrophy. It is typically bilateral, as in this case.OCT and FAF are highly valuable tools to aid in evaluation of the macula in patients with this disease.
The fundus photos (upper left of each set) illustrate the classic beaten bronze appearance of the macula with accompanying yellow deposits in Stargardt's disease.
Fundus autofluorescence (upper right) will likely show a bilateral, symmetric alteration in the autofluorescent signal often presenting in a bull’s-eye like pattern. These FAF images demonstrate hypoautofluoresence in areas of RPE atrophy and surrounding hyperautofluorescent pisciform lesions. Some patients present with milder phenotypes of the disease where pisciform-shaped deposits are present without such severe retinal atrophy. This presentation has historically been called fundus flavimaculatus.
OCT (bottom row) shows loss of outer retinal layers, including a loss of the photoreceptor integrity line.
Suggested reading:
Avoid Misdiagnosing Late-Onset Stargardt’s Disease for AMD
Pattern Recognition: How to Identify and Confirm Multifocal Pattern Dystrophy
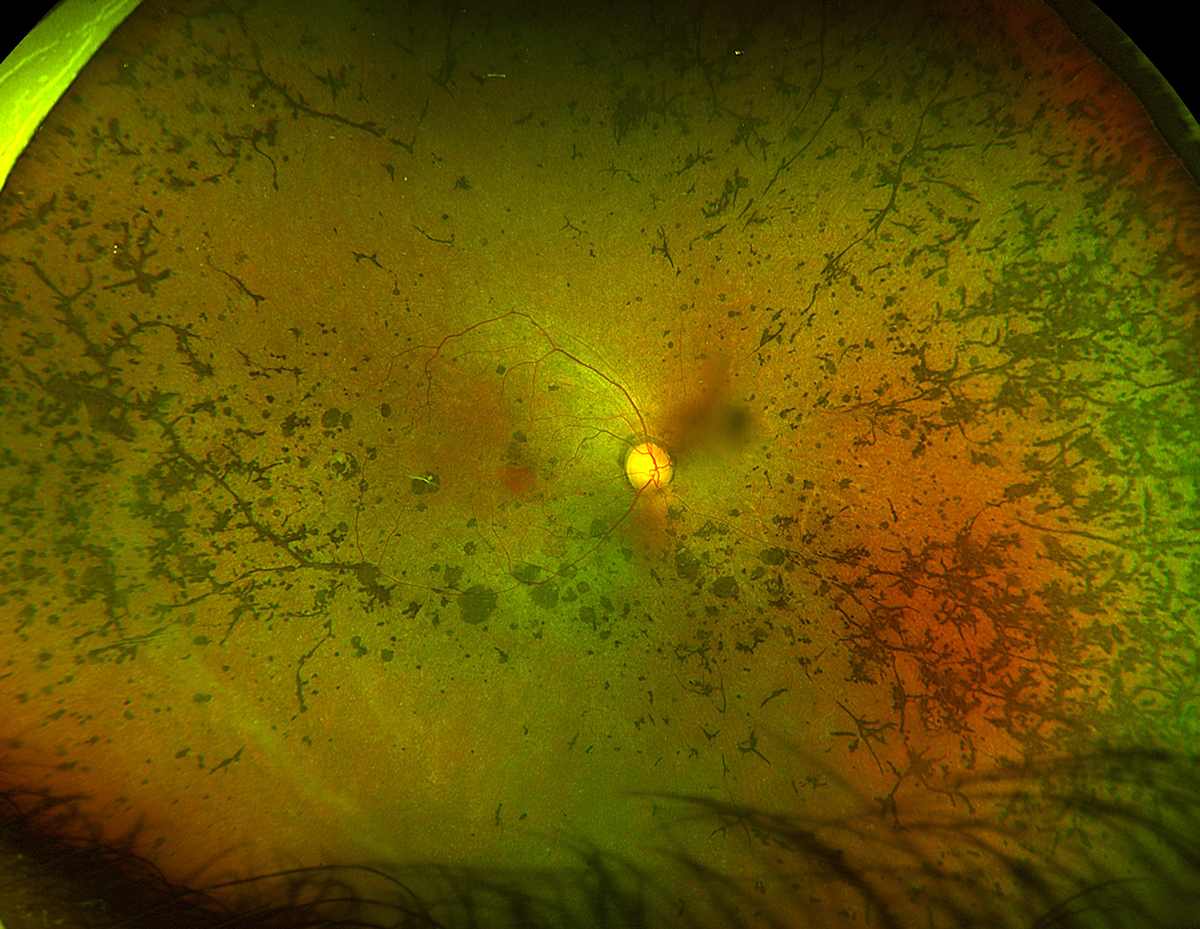
Retinitis pigmentosa
 |
| Photos: Rami Aboumourad, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
 |
| Click image to enlarge. |
 |
| Click image to enlarge. |
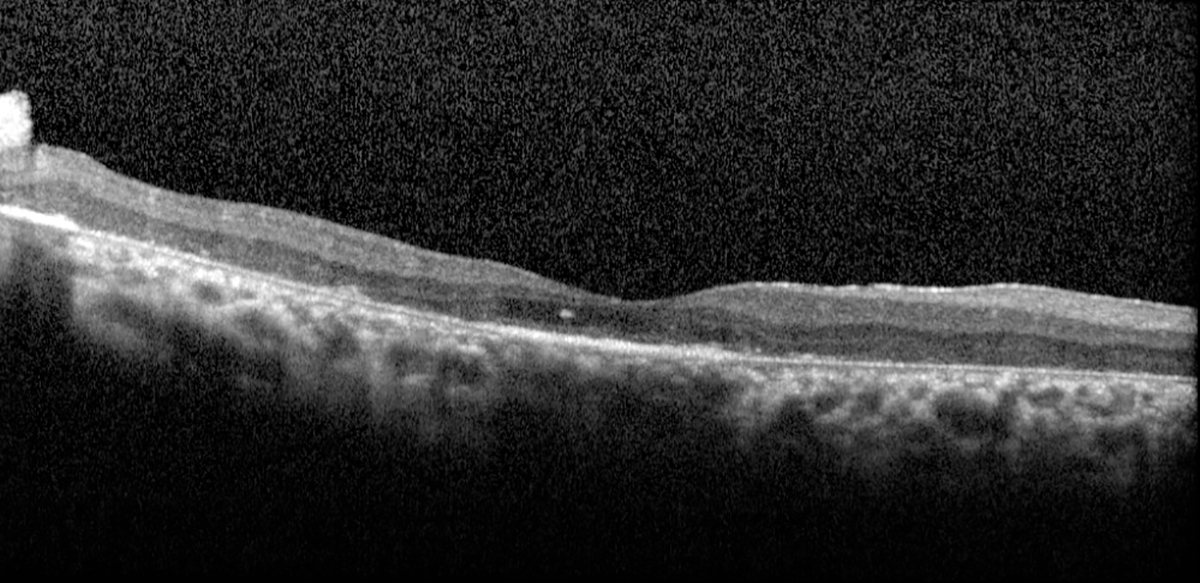
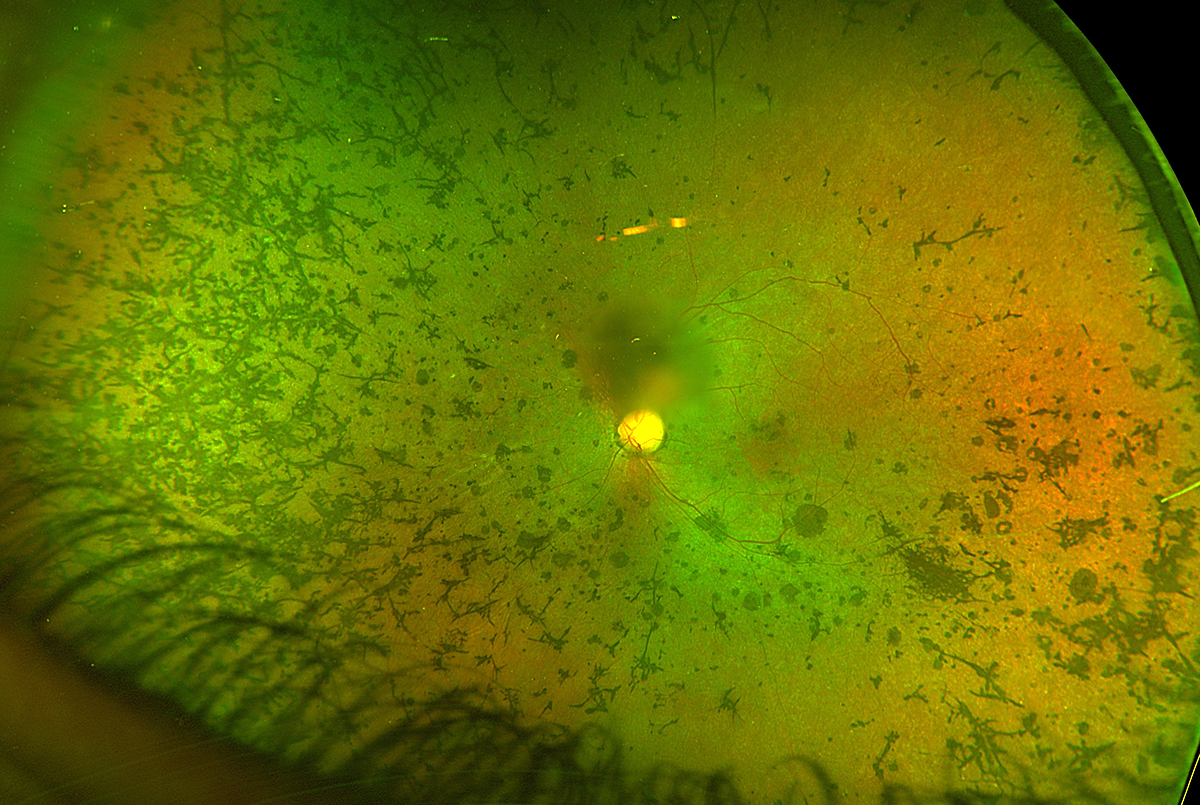
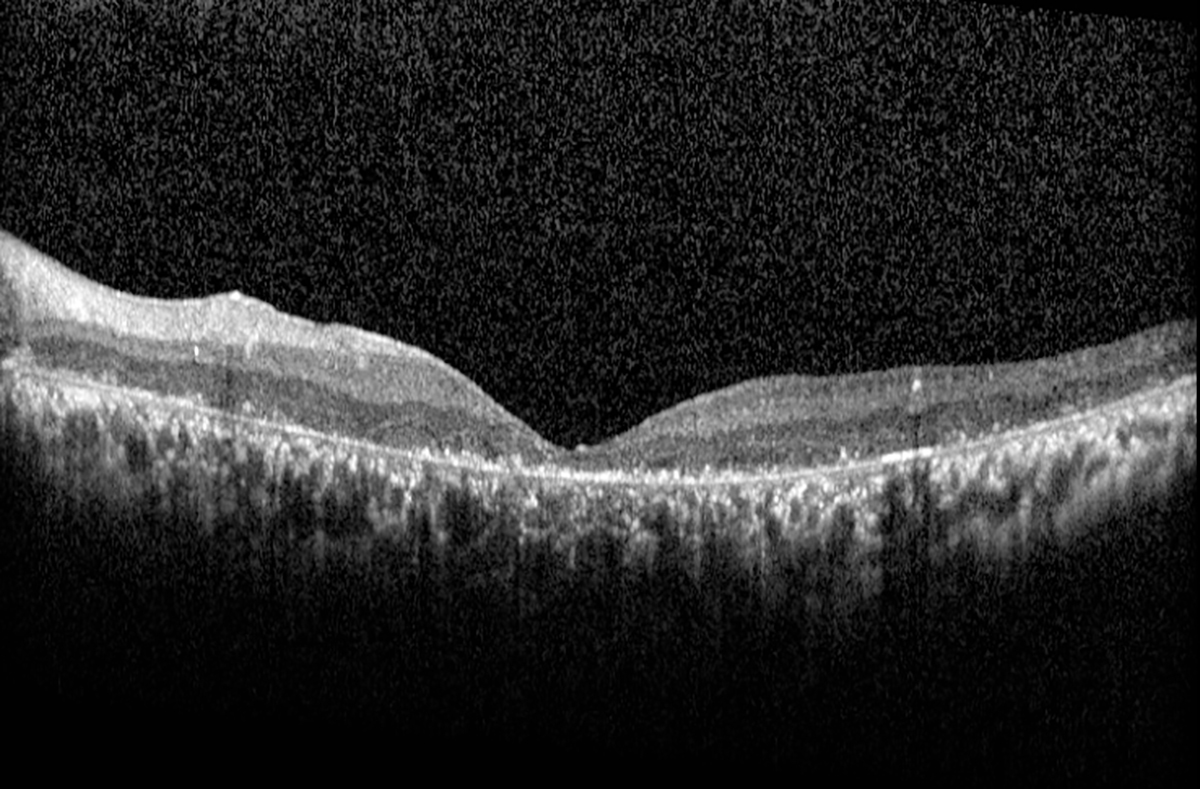
RP is a group of inherited disorders that results in the degradation of the rod (and eventually cone) photoreceptors. The classic presentation includes the triad of bone spicules, arteriolar narrowing and waxy optic disc pallor. These images show OD and OS findings in a typical case.
First image: Retinitis pigmentosa OD showing extensive retinal pigmentary changes (bone spicules) with a central island of remaining fovea. Of note, the optic nerve does not appear pale.
Second image: OCT OD of RP showing a central foveal island of remaining IS/OS with otherwise diffuse outer-retinal and RPE atrophy.
Third image: Retinitis pigmentosa OS showing extensive retinal pigmentary changes (bone spicules) involving the fovea. There is a central obscuration corresponding with posterior subcapsular opacification. Of note, the optic nerve does not appear pale.
Fourth image: OCT OS of RP showing extensive outer-retinal atrophy of the IS/OS line and RPE involving the fovea.
Suggested reading:
Tracing Clues Back to Retinitis Pigmentosa
Light at the End of the Tunnel
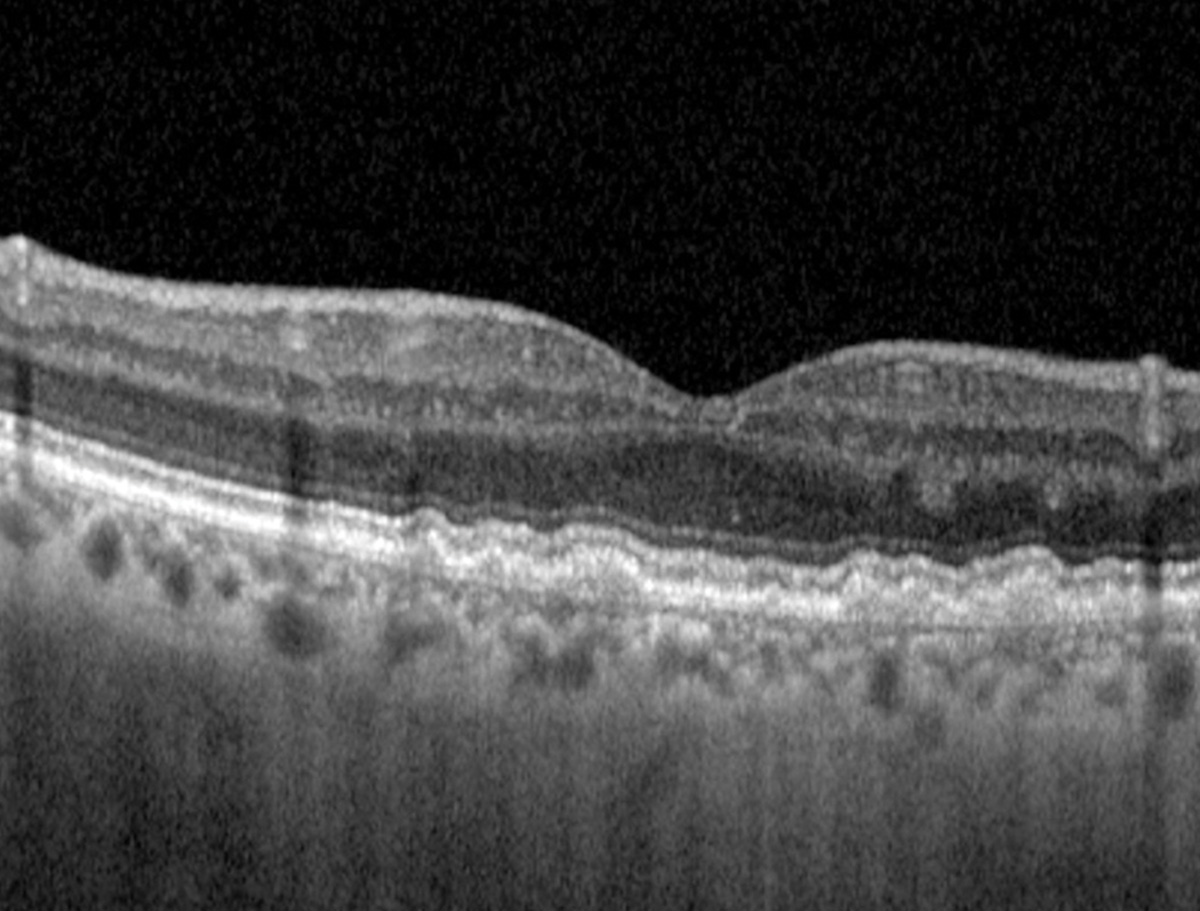
Vitelliform dystrophy
 |
| Photos: Jessica Haynes, OD. Click image to enlarge. |
 |
| Click image to enlarge. |
Adult-onset vitelliform dystrophy is one of the pattern dystrophies characterized by bilateral, round, yellow, vitelliform lesions that present in adulthood. On FAF, these lesions often appear hyperautofluorescent. On OCT they present as hyperreflective mounds between the RPE and PIL. Patients often maintain reasonable visual acuity unless they develop CNV or photoreceptor atrophy. Vitelliform lesions can easily be mistaken for choroidal neovascularizations.
Suggested reading:
Detecting and Managing Multifocal Vitelliform Dystrophy
Adult Vitelliform Maculopathy Management: From Anti-VEGF to Low Vision

